Should Supplemental Vitamins Be Taken If So Which Ones
Again, that depends on the extent and location of the disease. As noted above, vitamin B-12 is absorbed in the lower ileum. That means that people who have ileitis or those who have undergone small bowel surgery may have a vitamin B-12 deficiency because they are unable to absorb enough of this vitamin from their diet or from oral supplements. To correct this deficiency , a monthly intramuscular injection of vitamin B-12 may be required. Folic acid deficiency is also quite common in patients who are on the drug sulfasalazine. They should take a folate tablet, 1 mg daily, as a supplement. For most people with chronic IBD, it is worthwhile to take a multivitamin preparation regularly. If you suffer from maldigestion or have undergone intestinal surgery, other vitamins-particularly vitamin D-may be required. Affecting as many as 68 percent of people, vitamin D deficiency is one of the most common nutritional deficiencies seen in association with Crohns disease. Vitamin D is essential for good bone formation and for the metabolism of calcium. Supplementation of this vitamin should be in the range of 800 I.U./day, especially in the non-sunny areas of the country, and particularly for those with active disease. Together with vitamins A, E, and K, vitamin D is a fat-soluble vitamin these tend to be less easily absorbed than water-soluble vitamins. Consequently, they may be absorbed better in liquid rather than pill form.
You May Like: Is Ibs And Ulcerative Colitis The Same
Role Of Histamine And Mast Cells
Knuston et al observed that patients with CD of the distal ileum had a significantly greater mean histamine secretion rate within the small intestine than did healthy controls , and that histamine secretion was related to disease activity . Further study also suggested that histamine secretion was significantly increased in inflamed colonic mucosa in patients with both CD and UC when compared to their non-inflamed colonic mucosa or colonic mucosa in healthy controls. A more recent study showed that urinary excretion of N-methylhistamine was significantly increased in patients with active IBD when compared to inactive IBD or non-IBD controls and such urinary histamine excretion strongly correlated with endoscopic activity of CD measured by the CD Endoscopic Index of Severity . Greater expression of tumor necrosis factor- by mast cells was also found in the submucosa and muscularis propria of the ileum in patients with CD when compared to controls significantly greater numbers of TNFlabeled mast cells were noted in the muscularis propria both in uninflamed and in inflamed ileum . In addition, TNF- expression was found to be greater in the submucosa in inflamed vs uninflamed ileum in CD patients , while it was lower in the lamina propria in inflamed vs uninflamed ileum in CD patients . This is noteworthy as TNF- has been shown to be an important factor in the inflammatory cascade leading to the inflammatory response in the murine model for IBD.
Certain Foods Can Trigger Uc Symptoms In Some People
Has ulcerative colitis made you hesitant to eat for fear of causing painful symptoms? If you know for sure what foods make you feel worse, it’ll be easier to live with the disease. A review published in April 2019 in the journal Current Treatment Options in Gastroenterology noted that people with inflammatory bowel disease who had a diet full of fiber from fruits and vegetables, and low in animal fats, dairy, and processed food, had the fewest flares and best health outcomes. Doctors and nutritionists recommend that people who are diagnosed with ulcerative colitis change their dietary intake to ensure that they are consuming much-needed nutrients without exacerbating symptoms.
Whats the best way to identify what not to eat if you have UC? According to the research review mentioned above, starting an elimination diet for patients with Crohns disease or UC allowed 73 percent of patients to achieve remission in a six-week period. . Elimination diets, where patients remove certain foods from their diet to see if their symptoms abate, are a good way to identify common food triggers.
To get started on one, record all the food you eat during the day in a diary or journal along with any symptoms you experience. You can do this with pen and paper or with phone apps.
Recommended Reading: Pressure Ulcer Wound Care Dressings
Energy And General Health
If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.
Symptoms Similar In Celiac Gluten Sensitivity And Ibd
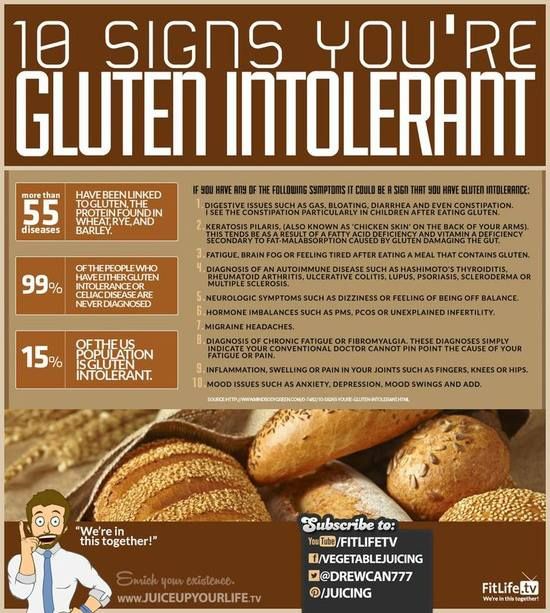
Celiac disease occurs when your body mistakes the gluten protein in wheat, barley, and rye for a foreign invader, triggering your immune system to attack your small intestine. Symptoms of celiac disease can vary widely , but many people with celiac suffer from diarrhea or constipation, stomach pain, fatigue, and anemia.
Symptoms of non-celiac gluten sensitivity can mimic those of celiac diseaseboth conditions include similar types of digestive issues. Those with gluten sensitivity, though, seem to suffer from more headaches and other neurological symptoms , such as nerve damage that causes a feeling of “pins and needles” in the arms and legs, than those with celiac disease.
Finally, symptoms of inflammatory bowel disease differ depending on which specific condition you have . Both Crohn’s and ulcerative colitis can cause abdominal pain, cramping, severe diarrhea, and bloat.
Read Also: Best Prebiotic For Ulcerative Colitis
Possible Links Between Celiac And Ibd
Some early studies found that people with celiac disease were at much higher riskpotentially as high as a 10-fold increase in riskof also being diagnosed with either Crohn’s disease or ulcerative colitis. However, more recent research has indicated that those with IBD have rates of celiac disease that are similar to those in the general population.
Still, there does appear to be some association between the two conditions, and genetics may explain part of that association. Recent genetic research has found that celiac disease and Crohn’s disease share four genes that appear to raise risk for both conditions. In addition, researchers have identified genes that appear to raise risk both for celiac and for ulcerative colitis.
Both IBD and celiac disease are considered autoimmune diseases, which means they involve a mistaken attack by your immune system on a part of your body. Both conditions also appear to involve problematic changes in your intestinal microbiome , that may cause or support inflammation.
Foods To Avoid During Flares
Diet doesnt cause flares, but your food choices can make symptoms worse if your IBD becomes active.
How foods affect people who are flaring varies from person to person. But here are some of the foods that may worsen symptoms of a flare and cause complications:
- Beverages containing alcohol or caffeine.
- Sugar alcohols used to sweeten in sugar-free foods
- Raw fruits and vegetables
Read Also: Can You Eat Cheese In Keto Diet
Read Also: What Medications Are Used For Ulcerative Colitis
More Information About Ulcerative Colitis
According to George Washington University, colitis is a chronic digestive disease characterized by inflammation of the inner lining of the colon. Infection, loss of blood supply in the colon, Inflammatory Bowel Disease and invasion of the colon wall with collagen or lymphocytic white blood cells are all possible causes of an inflamed colon.
The following diseases fall into the colitis/IBD category they all can be treated with a combination of medication and improvements to your eating habits:
Lactose Challenge Test And Lactose Sensitivity
It is important to distinguish between hypolactasia, assessed either by the polymorpisn CC13910 or through small intestinal biopsy and lactose sensitivity. The key clinical criterion for diagnosing lactose sensitivity in this study was the effect of an oral lactose challenge on breath hydrogen and methane, and the appearance of gut and systemic symptoms. Thus, participants were given 50g lactose as previously described. They were asked not to smoke for 4h prior to the breath test. They had also not received any antibiotic treatment or had bowel preparation for GI investigation in the 4weeks before the study. Lactose sensitivity was defined on the basis of breath analysis for hydrogen and methane over 6h as previously described, together with a record of both gut and systemic symptoms for up to 48h after the lactose challenge. Transit times through the small intestine vary considerably between individuals. This is why, on the basis of our previous study, we measured breath hydrogen and methane up to 6h after the lactose challenge. The initial rise in breath gases can give an indication of the transit time. However, unlike one report in a Greek population, we did not find this to be of value in assessing whether a patient was lactose sensitive or not.
Recommended Reading: How To Check A Horse For Ulcers
Read Also: What Causes Venous Stasis Ulcers
Digestive System Parts: A Brief Anatomy Overview
Now that we got that out of the way, lets take a deeper look at each of these conditions of the digestive tract.
Special Diets May Help
A variety of organizations and individuals recommend many different diets to help UC. Research generally warns against restrictive diets for UC because no one diet works for everyone. Also, very little research supports the idea that one diet by itself helps all people with UC.
However, these special diets may give you some ideas to work into your nutritional program. They all have slightly different takes on which vegetables are best. Look into them and see what works for you:
- Mediterranean diet
Read Also: What Are Ulcers In Horses
Don’t Miss: Stage 2 Pressure Ulcer Sacrum
Treatment For Celiac Disease
Treatment for celiac disease is far more simple.
Gluten-free diet: This is the centerpiece of treatment for celiac disease. The doctor will tell you to start eating this way before you leave the office. Most people with celiac have to avoid these foods for the rest of their lives:
Once you stop eating gluten, the inflammation in your gut should get better. If your small intestine is severely damaged, you may need steroids.
Also Check: Jasons Deli Allergy Menu
Foods To Eat During Ulcerative Colitis Flares

A bland diet is best during periods of active ulcerative colitis, when you may experience abdominal discomfort, blood in your stool, loss of appetite, fatigue, weight loss, vomiting, nausea, abdominal pain, and diarrhea. A safer diet during flares might include dry toast, applesauce, and white rice. Although some foods are more likely to be safe for those with UC, individual experiences can vary, especially during flares.
Here are some safer foods to try during ulcerative colitis flares:
- Low-fiber refined grains, such as oatmeal, potatoes, and sourdough bread
- Well-cooked vegetables that are easier to digest
- Vegetable broth, which can be added to grains like rice for additional nutrients
- Fruits or vegetables that contain more soluble fiber than insoluble fiber, such as bananas, carrots, and apples
- Bland protein, such as nut butters, eggs, tofu, and chicken
Diarrhea specifically raises concerns for loss of nutrients, such as potassium, sodium, magnesium, and phosphorus, through bodily fluids. If you choose to drink an electrolyte beverage, choose low sugar versions such as G2, Propel, or BodyArmor Lyte. You can also cut regular Gatorade or BodyArmor with water, diluting it by half.
You May Like: What Can Ulcers Do To You
Do Inflammatory Foods Play A Role In Ulcerative Colitis
If youre searching for an ulcerative colitis treatment that starts with your diet, you are far from alone. David Schwimmer, M.D., a board-certified gastroenterologist at Florida Digestive Health Specialists in Sarasota, Florida, sees ulcerative colitis patients on a daily basis and has even lived with the condition himself since he was 18 years old. I think every patient that has a GI illness certainly thinks that what they are consuming and what theyre eating has an impact on their disease, he says.
Exclusion diets like the specific-carbohydrate diet, the semi-vegetarian diet, and the IBD-inflammatory diet continue to grow in popularity within the IBD community. But research to prove that these diets are helpful for ulcerative colitis lags behind the trend. As recently as 2019, a study published in the journal Nutrients concluded that the mechanism by which dietary interventions impact inflammation in IBD remains unknown1. Basically, theres a lot more scientists need to learn before one type of diet reigns supreme for people with IBD.
High Calorie Gluten Free Snacks Suggestion
You May Like: Mouth Ulcers Treatment Home Remedies
Telling The Difference Between Conditions
Obviously, there’s considerable overlap between the symptoms of celiac disease, non-celiac gluten sensitivity, and inflammatory bowel disease, and that can make getting an accurate diagnosis somewhat challenging.
Healthcare providers use blood tests to screen for celiac disease , and confirm the diagnosis with an endoscopy and biopsy to look directly at the lining of your small intestine to see if it’s damaged.
To diagnose Crohn’s disease or ulcerative colitis, your healthcare provider likely will perform a colonoscopy and/or an endoscopy to look for specific signs, which are different from those of celiac disease. There’s no one blood test for inflammatory bowel disease, although more general blood testssuch as one to screen for anemiamay provide some information.
Finally, there’s no accepted medical test for non-celiac gluten sensitivity . The only way to know if you have it is to follow the gluten-free diet strictly and see if you feel better. But even that’s not definitive: you may feel better because you’ve reduced or eliminated junk food from your diet along with the gluten, for example, or just the idea that you’re doing something positive for your health may help lessen your symptoms. Still, research shows that some people do, indeed, seem to react to gluten grains with symptoms that are similar to those of celiac disease, even though those people definitely don’t have celiac disease.
Accomplishments Despite My Chronic Illness
Ive been working from home since 2015, and that definitely has helped me keep my condition under control. Despite everything I went through, Ive accomplished so many things.
- I worked as the CMO at Kinsta for 3+ years.
- I started a company, forgemedia LLC, with my brother. We now work on this full-time together.
- Even with all the medical bills, I managed to pay off all my student loan debt and am happy to be living life completely debt-free.
- My has generated more growth than I ever thought possible.
You can read more about my bio and accomplishments on my website: brianleejackson.com.
Also Check: Offloading The Diabetic Foot For Ulcer Prevention And Healing
What To Expect After Your Surgery
Most people do very well after their surgery and are able to return to work and their normal daily activities after they recover.
-
You should expect an adjustment period of up to one year to get used to the changes in your body after your proctocolectomy.
-
Some patients may still feel as if they need to have a bowel movement after their surgery, just as people who have lost a limb sometimes still feel as if the limb is still there. This called phantomrectum and it completely normal. It does not require any treatment and often subsides over time.
-
Your doctor may recommend a physical activity restriction for a minimum of six weeks, depending on what type of surgery you had.
-
Talk to your doctor about resuming normal sexual activity after your surgery. Some people find their sex life improves some time after surgery due to improvements in pain, inflammation, and other ulcerative colitis symptoms.