What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohn’s disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
Vitamin And Mineral Supplementation
Nutritional supplements are great for patients with inflammatory bowel disease who may need a bit of extra help preventing a nutritional deficiency.
Your healthcare providers may also recommend a vitamin and/or mineral supplementation plan if your tests show you already have a nutritional deficiency.
You may be able to get all your necessary vitamins and minerals from eating a well-balanced, nutrient-rich diet. But flares, severe symptoms, surgeries, and other complications may make it difficult for some patients with Crohns disease or ulcerative colitis to get enough nutrients from food alone.
Check with your doctor or other healthcare providers before taking any supplements, including over-the-counter medications, herbs, and other complementary therapies.
-
Some supplements can cause gastrointestinal symptoms, including nausea and diarrhea.
-
Check the labels on your supplements for lactose, artificial colors, sugar alcohols, or preservatives, all which can aggravate your IBD, especially when you are in a flare.
-
Most supplements should not be taken on an empty stomach.
Video Length00:02:00
Vitamin and Mineral Supplementation in IBD Often times, when you have Crohn’s disease or ulcerative colitis, you may need to take vitamins or minerals to prevent or make up for a nutritional deficiency. Watch and listen this video to learn more about common vitamin and mineral supplements for IBD patients.
Crohn’s Disease Exclusion Diet
The CDED is a whole foods diet designed to limit or exclude foods that may negatively affect the gut microbiome, inflammation, and the intestines ability to absorb nutrients or other functions. CDED excludes wheat, dairy, animal fat, additives, processed foods, and red meat. It includes readily available foods such as fruits, vegetables, rice, potatoes, lean meats, and eggs. In order to achieve energy needs and provide an extra supply of protein, calcium, and vitamin D it is recommended, in practice, to combine the diet with a variable amount of a formula as partial enteral nutrition .
The diet is set in three phases designed to gradually reintroduce diversified foods, provides progressively greater flexibility and improved quality of life. In phase 1, PEN comprises 50% of your calories during the first 6 weeks, decreasing to 25% of your calories over the following 6 weeks. After 12 weeks, there is a maintenance phase, where additional foods are included in the diet, the formula is maintained at 25% or adapted levels recommended by your specialized doctor or dietitian.
CDED has been shown to induce clinical remission and mucosal healing in pediatric and adult Crohn’s disease.
Clinical studies using Modulen IBD® as PEN show that CDED + PEN was as effective as the current EEN standard in achieving remission, but the CDED + PEN was better tolerated and superior for sustaining remission.
References
You May Like: Icd 10 Venous Stasis Ulcer
What Is The Outlook
With modern medical and surgical treatment, there is just a slight increase in the risk of death in the first two years after diagnosis, compared with the general population. After this there is little difference in life expectancy from that of the general population. However, a severe flare-up of ulcerative colitis is still a potentially life-threatening illness and needs expert medical attention.
As mentioned, if you do not take medication to prevent flare-ups, about half of people with ulcerative colitis have a relapse on average once a year. This is much reduced by taking regular medication. However, even in those who take regular medication, some people have frequent flare-ups and about a quarter of people with ulcerative colitis eventually have an operation to remove their colon.
A year from diagnosis, about 9 in 10 people with ulcerative colitis are fully capable of work. So, this means that, in the majority of cases, with the help of treatment, the disease is manageable enough to maintain a near-normal life. However, the condition can cause significant employment problems for a minority.
Treatment for ulcerative colitis is an evolving field. Various new medicines are under investigation. These may change the treatment options over the next ten years or so and improve the outlook .
What About Contests And Sweepstakes
When we run a contest or sweepstakes relating to our Sites, it will be accompanied by a set of rules. The rules for each contest/sweepstakes will specify how the information gathered from you for entry will be used and disclosed, if it is different than as described in this Privacy Policy. In conjunction with your entry in such contest or sweepstakes, Personal Information will be collected only if you voluntarily submit it to.
You May Like: What Do Venous Leg Ulcers Look Like
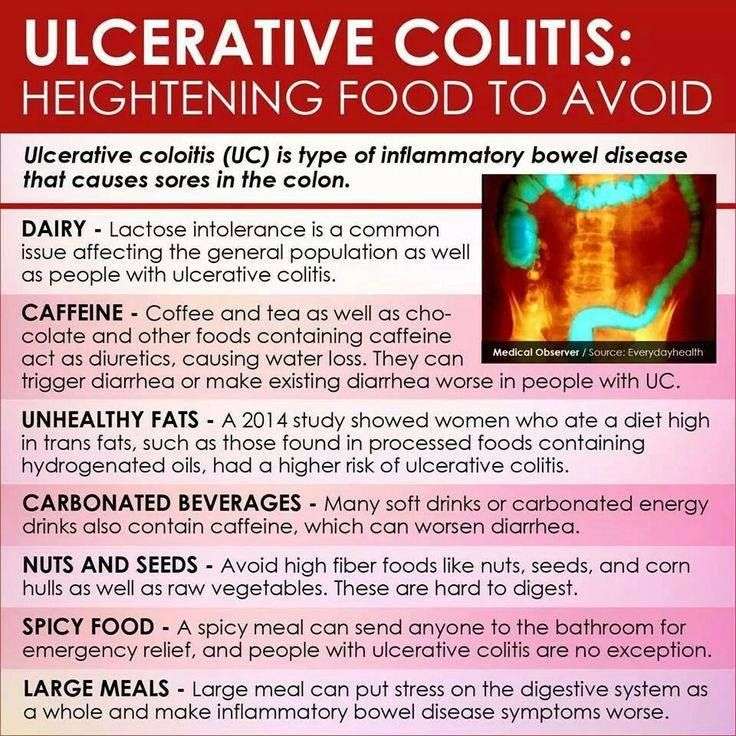
Other Foods Are Known Uc Harmers
On the other hand? Things like full-fat dairy, red or processed meats, unhealthy fats, and fried or greasy meals are thought to have the opposite effect, per recent guidance developed by the International Organization for the Study of Inflammatory Bowel Diseases . If trying to get more of the good stuff and less of the bad seems overwhelming, read on. Here, Stein and Rogers share some of their favorite UC-friendly food strategies that can reduce your symptoms and even make it easier to manage your UC long-term.
Types Of Inflammatory Bowel Conditions
Studies in large populations of patients with ulcerative colitis show the following conditions:
- 30% have limited proctitis , 30% have pancolitis , and 40% have left-sided colitis .
Although there are several layers that make up the colon, the inflammation of ulcerative colitis involves only the innermost lining called the mucosa. Over time, some patients who are initially diagnosed with limited disease like proctitis may progress in a continuous fashion from the rectum to parts of the colon and develop inflammation in these areas of the colon.
Snippet Highlight: Ulcerative colitis goes through cycles of flare-ups and remission when the disease is active. It usually requires some form of treatment before going back into remission when flare-ups happen.
Read Also: Infusion Medication For Ulcerative Colitis
Is Personal Information Collected From Children
Unless otherwise disclosed during collection and with parent or guardian consent, DashDiet.me does not knowingly collect personal identifiable information from children under 13 years of age. If you are under 13 years of age you should not under any circumstance provide personally identifiable information to DashDiet.me. If DashDiet.me discovers that a child under the age of 13 has provided DashDiet.me with personally identifiable information, DashDiet.me will immediately delete that child’s information from the Sites.
What Is The Best Natural Remedy For Ulcerative Colitis
A nutritionist experienced with ulcerative colitis can provide a detailed gut health nutrition plan with a day-to-day schedule, weekly menu ideas, and hopefully advice on eating out .
They will help you recognize your triggers and reduce flare-ups but also ensure that you get optimum nutrition that will be absorbed.
Gut microbiota contains trillions of bacteria that change continually with lifestyle factors such as food and drink we have, stress, what we breathe, medication, health conditions, and so on.
An alteration of your intestinal microbiome is a major factor in the pathogenesis of a chronic inflammatory disease of the gastrointestinal tract.
This means that promoting good microbiota with the right type and quantity of foods on a regular basis will reduce gut dysbiosis, promote regular immune activity, reduce inflammation and aid the healing and repair of the inflamed, permeable digestive tract and putting ulcerative colitis into remission.
Optimally modulating gut microbial diversity and stability will prevent gut dysbiosis. This will prevent chronic inflammatory diseases. Eating the right balance of good foods is imperative to further allow for nutrition absorption.
Pairing this ulcerative colitis nutrition protocol with an anti-inflammatory lifestyle will help you turn this all around. I assure you! It frees up a lot of thinking time.
Recommended Reading: First Line Treatment Ulcerative Colitis
What Happens When I Link To Or From Another Website
These Sites may contain links to other websites operated by affiliates of DashDiet.me or third parties. Please be advised that the practices described in this Privacy Policy for DashDiet.me do not apply to information gathered through these other websites. We are not responsible for the actions and privacy policies of third parties and other websites.
Supplements For Ulcerative Colitis
Because ulcerative colitis may interfere with your ability to absorb nutrients, its important that you use supplements to ensure that your body gets the vitamins and minerals that are necessary. Some supplements that may be helpful when combating the symptoms of ulcerative colitis include:
Also Check: What To Do When You Have A Stomach Ulcer
The Best Diet For Ulcerative Colitis
Most experts say that people with UC should simply try to eat a well-balanced diet whenever possible. This should include a variety of foods:
- Lean meat, fish, and poultry
- Low-fat dairy products
- Bread, cereal, and whole grains
- Fruits and vegetables
- Healthy fats such as vegetable oils
Keep a food diary to help you figure out which foods cause problems for you and whether or not youre getting enough nutrients.
If you lose weight because of your ulcerative colitis, try to eat five or six small meals and snacks during the day instead of two or three large meals.
When you have chronic diarrhea, drink plenty of water or other fluids to stay hydrated.
A dietitian can plan a diet that meets your calorie and nutrient needs. Before you take any dietary supplements, talk to your doctor or dietitian. Find out how to make a diet plan for ulcerative colitis.
You May Like: What Is Best Medicine For Ulcer
How Often Do I Need A Colonoscopy

Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
You May Like: H Pylori And Stomach Ulcers
Keeping A Food Journal
Everyones body is different, so its possible for two people who have UC to have different trigger foods.
Logging what you eat throughout the day and when digestive issues occur can help you and your doctor narrow down your personal food triggers.
A food journal can be especially helpful if youre trying a new diet.
What Foods Should I Not Eat When I Am Having An Ulcerative Colitis Flare
Certain foods can exacerbate or aggravate an UC flare and should be avoided. They are more likely to trigger cramping, bloating, and/or diarrhea and are also not recommended in people diagnosed with a stricture, which is a narrowing of the intestine caused by inflammation or scar tissue, or in those who have had recent surgery. Examples include:
- Foods high in insoluble fiber that are hard to digest, such as seeds, raw green vegetables , whole nuts, whole grains, or fruits with a skin
- Lactose, which is milk sugar found in dairy products, milk, cream, cream cheese, and soft cheeses
- Non-absorbable sugars such as sorbitol, mannitol, and other sugar alcohols that are typically found in sugar-free gum, candy, ice cream, and certain types of fruits and juices such as pear, peach, and prune juice
- Sugary foods such as candy, pastries, and juices
- High-fat foods such as butter or margarine, coconut oil, or fatty, fried, or greasy food
- Alcohol such as beer, wine, or spirits
- Caffeinated drinks such as coffee or energy drinks
You May Like: What To Drink With Ulcerative Colitis
Your Obligations To Keep Your Access Rights Secure
You promise to: provide true, accurate, current and complete information about yourself and your business as prompted by a Website’s registration form and maintain and promptly update the Registration Data to keep it true, accurate, current and complete. If you provide any information that is untrue, inaccurate, not current or incomplete, or DashDiet.me has reasonable grounds to suspect that such information is untrue, inaccurate, not current or incomplete, DashDiet.me has the right to suspend or terminate your account and refuse any and all current or future use of the Sites . You are entirely responsible for the security and confidentiality of your password and account. Furthermore, you are entirely responsible for any and all activities that occur under your account.
How To Prep Vegetables For Ulcerative Colitis
Cooked vegetables are often easier to tolerate than their raw counterparts, especially when youre in the middle of a flare. Altering the texture can be helpful, too. You can make veggies easier on your GI tract by:
- Peeling them Peeling vegetables such as carrots, parsnips, turnips, squash, and potatoes strips away some of the insoluble fiber, making them less irritating to the gut, say Warren and Leben.
- Cooking them until soft Methods that make veggies tender without the need for too much added fat tend to be best. Try baking, roasting, steaming, or lightly sautéing, Leben recommends.
- Mashing or pureeing them, if needed Particularly during a flare, purees and very soft textures can be easier to digest. Texture changes can help break down fibrous foods and improve tolerance, says Leben. Try mashing soft-cooked veggies or blending them into soups or smoothies, Warren recommends.
Recommended Reading: Best Alcohol To Drink With Ulcerative Colitis
Public Areas Chat Rooms Reviews And Community Areas
Please remember that any information you share in public areas, such as message boards or feedback sections, becomes public and anyone may take and use that information. Please be careful about what you disclose and do not post any Personal Information that you expect to keep private. Please consult the applicable guidelines, if any, for use of our chat rooms and other community areas for more information.
Best Foods For Ulcerative Colitis Patients
Ulcerative colitis is a health condition that is highly influenced by the diet of a person. Knowing which foods to eat can help avoid flares and make your symptoms better. Also, some foods can help avoid a ulcerative colitis flare. Here, we have mentioned a few food items that you can consider eating if you have this condition.
Here are the best foods for ulcerative colitis patients.
1. Refined GrainsPatients suffering from ulcerative colitis usually find it hard to digest whole grains. Hence, switching to cereal, bread, and pasta made from refined grains. You can also opt for bland items like cooked white rice if it is difficult to consume most foods.
2. ProbioticsYogurt is a good choice to add to your daily diet if you are suffering from ulcerative colitis. It contains live bacteria known as probiotics that help in digestion. Regular consumption of probiotics can reduce the symptoms and flares of ulcerative colitis. You can also choose probiotic supplements if you are lactose intolerant or do not prefer eating yogurt.
3. ApplesauceThis is one of the best foods for ulcerative colitis. However, try to avoid its consumption during a flare. Applesauce is soft, easily digestible, and a good source of nutrients. Make sure to choose unsweetened versions as the excess sugar can result in inflammation. It can be made at home by peeling and slicing up apples, cooking it in some water, and making a puree out of the mixture.
Dont Miss: Will Ulcers Cause Blood In Stool
Don’t Miss: Natural Cure For Stomach Ulcer
What To Eat During A Flare Up
It may be best to avoid more fibrous foods like whole grains, greens, and nuts when youâre having a flare up. Instead, look for easy-to-digest foods like:
- Refined breakfast cereals like cornflakes
- White rice instead of harder-to-digest brown or wild rice
- Low-fiber fruits like bananas, cantaloupe, honeydew melon, and cooked fruits
- Fully cooked non-cruciferous vegetables like asparagus tips, potatoes, squash without the peel, seeds, or stalks
- Refined, low-fiber pasta and noodles
- Lean meat and fish
For some people with UC, it also helps to break meals up into five or six smaller meals instead of three larger ones. You can talk to your health care team about going on an elimination diet. Thatâs when you stop eating different foods one at a time to see which ones tend to cause symptoms so you can remove them from your diet. Itâs important to work with your doctor or dietitian when you do this to make sure you get enough nutrients.
If you find that you are losing weight during a flare up, talk to your health care team. They might need to test to see if youâre getting enough of certain vitamins and minerals. They also may be able to help you zero in on foods that worsen your symptoms and help you replace them with healthy alternatives that will help you maintain a healthy weight. These might include some of the foods above, like bananas, eggs, lean meat, and noodles.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Don’t Miss: Evidence Based Practice Guidelines For Pressure Ulcer Prevention