Skin And Wound Care Practices Today
You will hear clinicians who would never dream of practicing medicine and nursing exactly the same way they did 30 years ago falling back on what they perceive as acceptable care for patients at risk for or presenting with a pressure ulcer. I STILL hear people promoting liquid antacids, povidone iodine, sugar, off the grocery shelf honeythe list seems endless. Yet they will swear their patient healed. My assertion is that some patients healed despite the awful things someone put on their wound. We need to apply evidenced-based practice in skin and wound care the same careful way we apply those principles to other aspects of health care.
About The AuthorPaula Erwin-Toth has over 30 years of experience in wound, ostomy and continence care. She is a well-known author, lecturer and patient advocate who is dedicated to improving the care of people with wounds, ostomies and incontinence in the US and abroad.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, Kestrel Health Information, Inc., its affiliates, or subsidiary companies.
Infrastructure To Support Change
Sarasota Memorial Healthcare System, a magnet recognized not-for-profit organization, is committed to delivering safe, high-quality care that results in desired outcomes and is consistent with current professional knowledge . The organizational culture is reflected in the mission statement as well as the organizations participation with several agencies including The Joint Commission, the Agency for Healthcare Research and Quality Patient Safety Indicators, the American Nurses Credentialing Center Magnet Program , and many other health care accrediting agencies. Interdisciplinary collaboration is encouraged as evidenced by interdiscipli-nary meetings that focus on identifying the need for change and implementing evidence-based practice . Change that results in improved patient outcomes is encouraged by the executive team, risk management, nurse educators, several practice councils, and unit managers. Initiation of and participation in change is recognized by nurse of clinical excellence awards. At SMH, proposed changes are commonly presented to unit practice councils throughout the organization. Council members vote on the proposed change, and if the majority of the UPC members and council chair agree upon the proposal, the specified change in practice is implemented systematically.
Evidence Is Lacking In All Areas Of Pressure Ulcer Prevention And Treatment
Other Cochrane reviews found insufficient evidence to inform practice on the use of nutritional interventions to prevent or promote pressure ulcer healing on topical agents and massage as preventive measures and on treatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. with pressure-relieving devices for heel pressure ulcers , ultrasound antibiotics and antiseptics , phototherapy reconstructive surgery electromagnetic therapy and bed rest for wheelchair users with pressure ulcers .
There is no good evidence to support any particular wound cleansing agent or technique for pressure ulcers . There was no evidence from randomizedRandomization is the process of randomly dividing into groups the people taking part in a trial. One group will be given the intervention being tested and compared with a group which does not receive the intervention . studies on the impact of wound-care teams for pressure ulcer prevention and management . Nor has the use of structured riskA way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as the chance of falling were one in four . This measure is good no matter the incidence of events i.e. common or infrequent. assessment tools been shown to be effective in reducing pressure ulcer incidence .
Read Also: Best Treatment For Diabetic Foot Ulcer
Learn The Risk Factors And Tailor Prevention To Device Type
Takeaways:
- Medical devicerelated pressure injuries are a common but preventable patient care issue with simple interventions.
- Prevention guidelines and evidence-based practices can help reduce MDRPIs.
Editors note: The author has provided the attached PDF file of a clinical tips card for preventing medical device related pressure injuries. The card is 2 inches by 7 inches the spot at the top indicates where a hole could be punched to put a laminated version of the card on a lanyard. It could also be carried in the pocket and posted in the unit.
THE Joint Commissions Quick Safety issue on managing medical devicerelated pressure injuries points out that nearly all hospital patients require at least one medical device for care and treatment, putting them at risk for injury. The National Pressure Ulcer Advisory Panel defines MDRPI as localized damage to the skin and/or underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear.
Nurses can take the lead in preventing MDRPIs by understanding risk factors, tailoring prevention to the device type, collaborating with other team members to ensure continuity of care, and monitoring for change.
Starting With A Clinical Problem
The initiative began in 1993 when an increase in the incidence of pressure ulcers was perceived in our setting. There had been more referrals to the enterostomal therapist and to plastic surgery, and sporadic reporting by clinical staff of their suspicions that skin breakdown was increasing in their areas. At that time no unit based mechanism for capturing reliable data on pressure ulcers was in place nor was it possible to retrieve data from the hospital information system.
Even though it is a quality issue, the pressure ulcer initiative was set in a larger context of professional practice by linking it to the existing nursing quality improvement, research, and education infrastructures. The nurse specialists for quality improvement and research and evaluation took the lead on the project with support from several clinical nurse educators and managers. Critical to the success of the project was the support of the chief nursing officer who was vice president of patient services.
The task force recommended that the following issues be addressed in planning for effective care and prudent use of resources:
-
Baseline assessment of the extent of the problem
-
Evaluation of the accuracy of a risk assessment method
-
Practice changes including development of an educational strategy to upgrade nursing skills in pressure area assessment using grading or staging of sores
-
A method for ongoing monitoring.
Also Check: First Line Treatment Ulcerative Colitis
Assignment: Pressure Ulcer In Icu In Uk
1- Critique different types of evidence 2- Analyse what constitutes Best Evidence for practice in the UK3- Critically reflect on the BENEFITS and LIMITATIONS of evidence based practice within nursing practice. Using Randomised Controlled Trial Student will critique a qualitative and quantitative research paper and explore how research and EBP apply to nursing practice.Harvard Reference, CINAHL, NICE,
Introduction
Pressure Ulcer Prevention: Evidence
The quality of healthcare services and the possibility to reach positive health outcomes depend greatly on various dimensions, and pressure ulcer rates are among them. They are defined as localized injury to the skin and/or underlying tissue, usually over a bony prominence, as a result of pressure alone or in combination with shear . This issue is often faced by individuals with limited mobility because they spend a lot of time in hospitals and have no possibility to move as needed. Professionals indicate that this problem is not rare and almost 3 million people in the USA suffer from it.
What is more critical, during the last decade of the 20th century, they were reported to cause the death of more than 110,000 individuals. In addition to that, about 21,000 deaths were connected with this problem indirectly. Such data makes professionals realize the severity of the situation and implement various initiatives to improve the situation. The purpose of this paper is to present a proposal for evidence-based practice project about the prevention of hospital-acquired pressure ulcer incidence rate during their hospital stay, discussing the influence of the Braden and Waterlow scale that can be used to predict pressure ulcers, compared to clinical judgment alone, on the basis of the adult population.
Also Check: What Is Best Medicine For Ulcer
Pressure Injury Prevention & Management
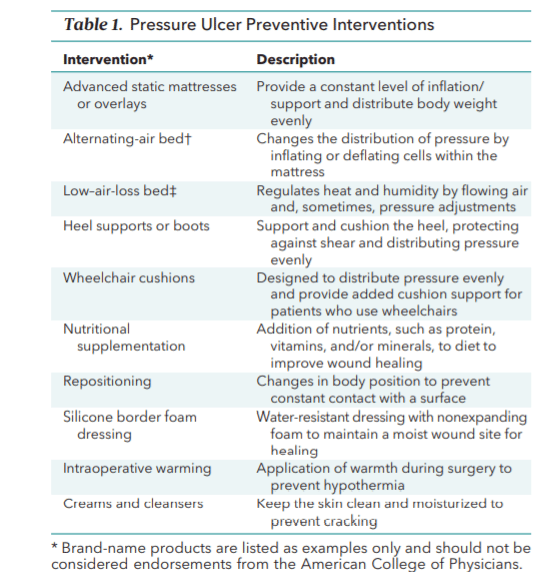
Implementing an evidence-based best practice system for pressure injury prevention and management can reduce the potential for pressure injury development and promote healing of existing pressure injuries.
Each person should be assessed for pressure injury risk factors on admission and receive an in-depth assessment of any existing pressure injuries. The assessment process drives the development of person-centered goals and interventions to prevent or heal pressure injuries.
The care plan should reflect the persons preferences, values and needs and identify the interventions necessary to meet his/her goals for treatment. The care plan should also include guidelines for reassessment to evaluate the effectiveness of the care provided and to prompt changes in treatment as needed. The use of any particular intervention should be based on the strength of the evidence provided by existing clinical trials or literature reviews.
Evaluation and monitoring outcomes are vital components of any program for managing pressure injury risk and treating existing pressure injuries. An effective system includes reassessment of the persons risk for developing a pressure injury. The frequency of reassessment will depend on a variety of factors, with more frequent assessments for people with existing pressure injuries, those who are at high risk for developing pressure injuries, or those who have experienced a significant change of condition.
Improving Patient Outcomes Through Evidence
Specialization and evidence-based practice have improved patient outcomes for a variety of conditions. The flip side of this coin is the care of the entire patient can be compromised. This is especially problematic when addressing the risk factors associated with the development of pressure ulcers. Over the years, medical and nursing care of pressure ulcers has evolved from trial and error and ‘that is how we have always done it’ to carefully investigating and analyzing the science behind our interventions and tracking patient outcomes. When I was a nursing student in the mid-1970s, the standard treatment for ‘decubitus care’ was applying a liquid antacid and placing the patient under a heat lamp for 10 minutes at least twice a day. I shudder when I think of the damage we inflicted on our patients with nothing but the best of intentions.
Don’t Miss: Foods For People With Ulcerative Colitis
Pressure Ulcer Prevention Practices And Associated Factors Among Nurses In Public Hospitals Of Harari Regional State And Dire Dawa City Administration Eastern Ethiopia
-
Roles Conceptualization, Investigation, Methodology, Resources, Software, Supervision, Validation, Writing original draft, Writing review & editing
Affiliation School of Nursing, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
-
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Software, Supervision, Validation
Affiliation School of Nursing, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia
What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
You May Like: Vitamin E And Ulcerative Colitis
Family And Individual Level
Healthcare professionals can have an impact on an individual level by:
- recognising the important role individuals, families and carers have in preventing and managing pressure ulcers
- engaging individuals, carers and families in what to look for and how pressure ulcers can be prevented
- using appropriate literature with visual images to explain how quickly pressure ulcers can develop
- educating the individuals and caregivers about the causes, assessment and management of pressure ulcers
- using appropriate terminology recognising and informing patients that pressure ulcers are another term for bed sores
- encouraging individuals to move independently whenever possible
- directing individuals to appropriate healthcare professionals if they suspect a pressure ulcer is forming or is present
- looking out for skin discolouration or soreness, particularly in areas where bones are close to the skin
- repositioning or turning patients frequently at least every 2 hours for those patients who need help
- using moving and handling aids to help reposition individuals who require assistance moving
- performing regular skin inspections to check areas at risk and document pressure areas at least once a day
- checking that patients with pressure ulcer risk factors are registered with a GP and receive primary health care support to minimise the risks
- providing holistic health assessments for people at risk of developing pressure ulcers
Priorities In Pressure Ulcer Research
Not only do we need research to be designed, implemented and reported in ways that ensure it is useful, but to address the most important aspects of pressure ulcer prevention and treatment.
One of the objectives of the Wounds Research for Patient Benefit Programme Grant was to research priorities for people with complex wounds from the perspectives of patients, carers and healthcare professionals. Pressure ulcers were selected as the focus for the first National Institute for Health Research James Lind Alliance Priority Setting Partnership on complex wounds and with this came the particular challenges of involving people with pressure ulcers in research associated with their age, multiple morbidities and social isolation. Indeed the service users who participated in this research prioritization exercise were generally younger and fitter than those most at risk of pressure ulcers, nevertheless the PSP succeeded in identifying research priorities which capture the views of patients, carers and healthcare professionals . Of the top 10 priorities, which were extended to 12 during the PSP prioritization exercise, the first five concern pressure ulcer prevention.
The Chief Investigator of the Programme Grant, Professor Nicky Cullum from the University of Manchesters School of Nursing, Midwifery and Social Work, who is also the Co-ordinating Editor of Cochrane Wounds, is looking to the future of wounds research:
Also Check: Can You Get Ulcerative Colitis At Any Age
Pressure Ulcers Are Common
A prevalenceThe proportion of a population who have a particular condition or characteristic. For example, the percentage of people in a city with a particular disease, or who smoke. survey conducted in the city of Leeds as part of an NIHR-funded five year programme of work, the Wounds Research for Patient Benefit , demonstrated that complex wounds are common, with an estimated point prevalence of 1.47 per 1000 people , and that pressure ulcers were the most frequent type of complex wound .
The survey also found that most people were receiving wound care from community nurses, with a median of two visits per week, lasting just under half an hour. The standard of care was generally high almost 95% of all pressure ulcers had a documented European Pressure Ulcer Advisory Panel ulcer severity classification in line with NICE guidelines and 73% of people with pressure ulcers had a pressure-relieving mattress.
Clearly nurses are working hard on pressure ulcer management. The cornerstones of care revolve around low technology interventions such as repositioning essentially nothing new. But is, what is considered to be best practice, actually evidence-based practice and does this matter?
Understanding The Extent Of The Local Problem
A 12 hour prevalence survey was done on all inpatient units to establish risk of pressure sore development and the proportion of patients with skin breakdown. Volunteer clinical nurses collected the data after instruction about evidence-based practice, clinical practice guidelines, and how to assess prevalence. After a 2 week follow up period, all new occurrences of pressure ulcers were documented and the accuracy of a risk assessment scale was evaluated.
Recommended Reading: Is Ulcerative Colitis Worse Than Crohn Disease
What Bundle Of Best Practices Do We Use
Given the complexity of pressure ulcer prevention, with many different items that need to be completed, thinking about how to implement best practices may be daunting. One approach that has been successfully used is thinking about a care bundle. A care bundle incorporates those best practices that if done in combination are likely to lead to better outcomes. It is a way of taking best practices and tying them together in a systematic way. These specific care practices are among the ones considered most important in achieving the desired outcomes.
The pressure ulcer bundle outlined in this section incorporates three critical components in preventing pressure ulcers:
- Comprehensive skin assessment.
- Standardized pressure ulcer risk assessment.
- Care planning and implementation to address areas of risk.
Because these aspects of care are so important, we describe them in more detail in the subsequent subsections along with helpful clinical hints. While these three components of a bundle are extremely important, your bundle may stress other aspects of care. It should build on existing practices and may need to be tailored to your specific setting. Whatever bundle of recommended practices you select, you will need to take additional steps. We describe strategies to ensure their successful implementation as described in Chapter 4.
The challenge to improving care is how to get these key practices completed on a regular basis.
Resources
Additional Information
Tools
Practice Insights
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Skin integrity .
Tools
Detailed instructions for assessing each of these areas are found in Tools and Resources .
Action Steps
Recommended Reading: How Does Ulcerative Colitis Affect The Large Intestine