Canned Or Cooked Seedless Skinless Vegetables And Fruits
As mentioned above, its important to avoid high-fiber fruits and vegetables during a flare-up. However, its still important to give your body the nutrients it needs. For this reason, youll want to make sure that you eat plenty of cooked or steamed fruits without skins or seeds. You can also safely eat pureed soups and sauces made from vegetables.
Protein Intake As A Risk Factor For Ibd
Similarly, according to Agus and colleagues , an excessive consumption of animal proteins is associated with an increased risk of developing CD while the consumption of fruit and vegetables was inversely related to the risk of CD . Patients with CD also showed a shift in the microbiota, with an increase of Proteobacteria and Bifidobacteria groups, and a decrease of Firmicutes . For UC, in addition to the large consumption of refined carbohydrates and simple sugars, the consumption of large amounts of fatty acids is also associated with an increased risk of the disease . A large prospective cohort study completed over a 10.5 year period found that a high protein intake, specifically animal proteins was positively associated with an increased risk of IBD . A systematic review reported an association of a high total protein intake with the development of UC and CD . A high protein intake was associated with a 3.3-fold increased risk of IBD, suggesting that a diet high in animal proteins could be a major risk factor for the development of IBD.
Know Your Trigger Foods
Some fruits and vegetables create more gas in our GI tract, says Manning, like broccoli and cabbage, as well as watermelon and cherries, so I advise against eating these when symptoms are severe. Instead, says Julia Zumpano, a registered dietitian at the Cleveland Clinic, try cooked carrots, peas, or green beans, or peeled white or sweet potatoes, squash, or cucumbers because these vegetables are usually well tolerated by people with ulcerative colitis. Fruits that you might more easily digest include bananas, cantaloupe, honeydew melon, papaya, mango, and apples that have been peeled and cooked into homemade applesauce.
Keep in mind, however, that foods can affect people differently. The fruits and vegetables mentioned here are only suggestions, and youll need to determine your personal triggers through trial and error. Many people are unsure what causes , says Manning, so they avoid whole categories of food unnecessarily. When this happens, nutrition can become compromised and deficiencies can occur. Keeping a food journal and working with a registered dietitian can help you detect patterns and identify troublesome foods.
Are you ready to put this knowledge to use? Here are five veggie-centric recipes to try. Omit any known food triggers, of course, and adjust the recipes to fit your needs.
Read Also: How To Treat H Pylori Ulcer
What Everyone With Ulcerative Colitis Should Know About Produce
People with ulcerative colitis often have multiple bouts of loose bowel movements during a flare-up. When this occurs, says Manning, one should alter the texture of the diet so as to make it less abrasive on an inflamed and ulcerated colon.
You may therefore find cooked fruit and veggies to be more easily tolerated. Cooking whether you bake, roast, or boil helps break down dietary fiber, making produce easier to digest.
Another trick is to peel your fruit and veggies such as apples, pears, cucumbers, and potatoes because the skins are particularly high in fiber. You don’t want large amounts of insoluble fiber in the foods you eat, Manning says. By simply peeling and cooking, the abrasiveness is significantly lower.
You can also try consuming fruit and vegetables in soups and smoothies. For smoothies, Manning suggests that you use a protein base, such as 100 percent whey protein powder or soy or rice protein powder. Your protein needs are higher with IBD especially in a flare state, she says. Then add fruits that are peeled, but don’t use fruits with seeds. Try bananas, peaches, mango, papaya, and melons. She also recommends adding smooth nut butters for nutrients and flavor. Vanilla extract and cocoa powder are some other flavorful options to include. Make sure you blend the ingredients until very smooth so that your drink is easier to digest.
RELATED:8 Foods to Eat During an Ulcerative Colitis Flare
Track The Good And The Bad
There’s no single diet that will help everyone with UC. The condition can also change over time, so your plan will need to be flexible, too. The key is to find what works for you.
To stay organized, keep a food diary. Use your smartphone or a small notebook to record what you eat and drink and how they make you feel, both good and bad. It takes a bit of time and patience, but it will help you track your condition and fine-tune your diet plan.
When you prepare your meals, don’t forget that a well-balanced diet gives you enough protein, whole grains, and fresh fruits and vegetables.
You might not be able to eat everything in the grocery store or on the menus at the restaurants you like. But try to focus on the ones that you can enjoy without triggering your symptoms. Some simple tweaks in your meal prep can make it easier to eat some foods, like steaming veggies or switching to low-fat dairy.
Some people follow a low-residue diet or low-fiber diet every so often, getting about 10-15 grams of fiber a day. That can help you go to the bathroom less often.
Watch out for items that can be troublemakers if you have UC, including:
Recommended Reading: Can Stomach Ulcers Cause Back Pain
How To Prep Vegetables For Ulcerative Colitis
Cooked vegetables are often easier to tolerate than their raw counterparts, especially when youre in the middle of a flare. Altering the texture can be helpful, too. You can make veggies easier on your GI tract by:
- Peeling them Peeling vegetables such as carrots, parsnips, turnips, squash, and potatoes strips away some of the insoluble fiber, making them less irritating to the gut, say Warren and Leben.
- Cooking them until soft Methods that make veggies tender without the need for too much added fat tend to be best. Try baking, roasting, steaming, or lightly sautéing, Leben recommends.
- Mashing or pureeing them, if needed Particularly during a flare, purees and very soft textures can be easier to digest. Texture changes can help break down fibrous foods and improve tolerance, says Leben. Try mashing soft-cooked veggies or blending them into soups or smoothies, Warren recommends.
How Can I Track Foods That Cause Flare
The Crohn’s and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohn’s and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
Recommended Reading: Foods Not To Eat When You Have Ulcerative Colitis
Who Should Avoid Chia Seeds
Zellner that people with known allergies to mint, sesame, or mustard seeds should be cautious about trying chia seeds. Symptoms of a food allergy can include nausea, vomiting, itching of the lips or tongue, and wheezing. If you have a food allergy, talk to your doctor or pharmacist. 5. Acids.
According to the National Institutes of Health, Omega 3 fatty acids are essential for brain and nervous system development and function. Omega 3s are found in fish, fish oil, nuts, seeds, flaxseeds, walnuts, soybeans and other plant-based foods.
Can Ulcerative Colitis Cause Rash And Skin Irritation
Swollen and painful areas of skin are common and affect up to 15 percent of individuals with UC. In general, skin irritation and rashes will get worse during a flare and resolve during periods of remission. These rashes oftentimes fluctuate in-line with the inflammation throughout your entire body. While most skin irritation and rashes are caused by Ulcerative Colitis inflammation, general UC symptoms do not always cause the irritation and rashes.
There are numerous skin conditions associated with Ulcerative Colitis, many of which are caused by auto-immune functions:
- Erythema nodosum
Learn more about these conditions and how to treat them in our full discussion on Ulcerative Colitis and skin irritation / rash.
You May Like: How To Cure A Bleeding Ulcer
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Ulcerative Colitis Diet: What To Eat To Manage Symptoms
A tailored diet for ulcerative colitis may provide you with some relief
Ulcerative colitis is a type of inflammatory bowel disease in which the immune system is thought to attack the gut lining, failing to recognise it as part of the body. A focused ulcerative colitis diet may therefore help with the management of symptoms. With the guidance of an IBD team or a dietician, those suffering from ulcerative colitis can be put on an elimination diet in order to identify potential trigger foods, or may be encouraged to keep a food diary in order to track links between certain foods and symptoms.
Those who have undergone surgery or are struggling with an ulcerative colitis flare up may be put on a low residue diet or a low fiber diet in order to manage symptoms and lessen the burden of their disease.
However, ulcerative colitis diets are often unique to the individual, so some experimentation under medical supervision may be necessary to find the right eating pattern for you. An ulcerative colitis diet may not work at all either, so it is important to collaborate with your medical team in order to properly manage your condition.
Recommended Reading: Ulcerative Colitis Flare Up Treatment Guidelines
What To Eat During Flare
Low-fiber foods are easiest to digest and are less irritating to the gut, especially with symptoms like abdominal pain or diarrhea. Choose:
- Grains/starches: White foods, instead of wheat or whole-grain, and those with less than 2 grams of fiber per serving
- Cooked vegetables: Well-cooked vegetables such as green beans, carrots, mashed potatoes without skin, steamed asparagus tips and pureed squash.Use fresh or frozen.
- Canned or soft fruits: Peeled apples, ripe bananas, cantaloupe, honeydew, watermelon, and canned fruit in fruit juice or light syrup
Be sure to eat enough protein Inflammation causes increased protein needs. Choose:
- Tender, well-cooked meats: Poultry, salmon or other fish, lean beef and pork prepared without added fat
- Deli meats: Low-sodium and low-fat varieties
- Eggs: Well-cooked
- Smooth nut and seed butters: Peanut, almond or sunflower seed
Drink plenty of fluids Aim for eight cups a day, and consider using oral rehydration beverages as needed. Try to limit caffeinated, sugar drinks and beverages made with sugar substitutes.
Limit added fats and oils Focus on oils instead of solid fats, and limit intake to less than eight teaspoons per day.
Consume adequate calcium, vitamin D, probiotics, and prebiotics Sources include:
Ulcerative Colitis: Let’s Talk

Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Recommended Reading: Treatment For Stomach Ulcers Caused By Stress
My Health Journey With Ulcerative Colitis
I feel like it is long overdue for me to share my health story on here! I have spent a long time trying to not talk about this disease, to downplay symptoms, and to pretend like it doesnt exist. But it is a part of me and always will be, so I am trying my best to be more open, more vulnerable, and more real. So let me tell you about my journey with ulcerative colitis.
I was first diagnosed with ulcerative proctitis, which is a pretty mild form of inflammatory bowel disease , in 2013. To be honest, once I started taking medication, I would completely forget I had it most days. I carried out life just as usual, eating whatever I wanted and going out all the time. Then things started to get a little more serious and I wasnt feeling so great. I got re-tested in 2017 and found out that things had progressed a lot, and I was then diagnosed with ulcerative colitis . UC and Crohns disease are the two diseases that make up IBD. Both UC and Crohns disease are autoimmune diseases UC affects just the colon , while Crohns can affect any part of the GI tract.
Its truly mind-blowing how prevalent autoimmune diseases are becoming especially in women. I can count four other people in my groups of friends that have autoimmune diseases most of them affecting the gut. I have become a tad obsessed with learning about autoimmunity and especially the role the gut microbiome plays in it, so you can expect more posts on these topics.
xx Cami
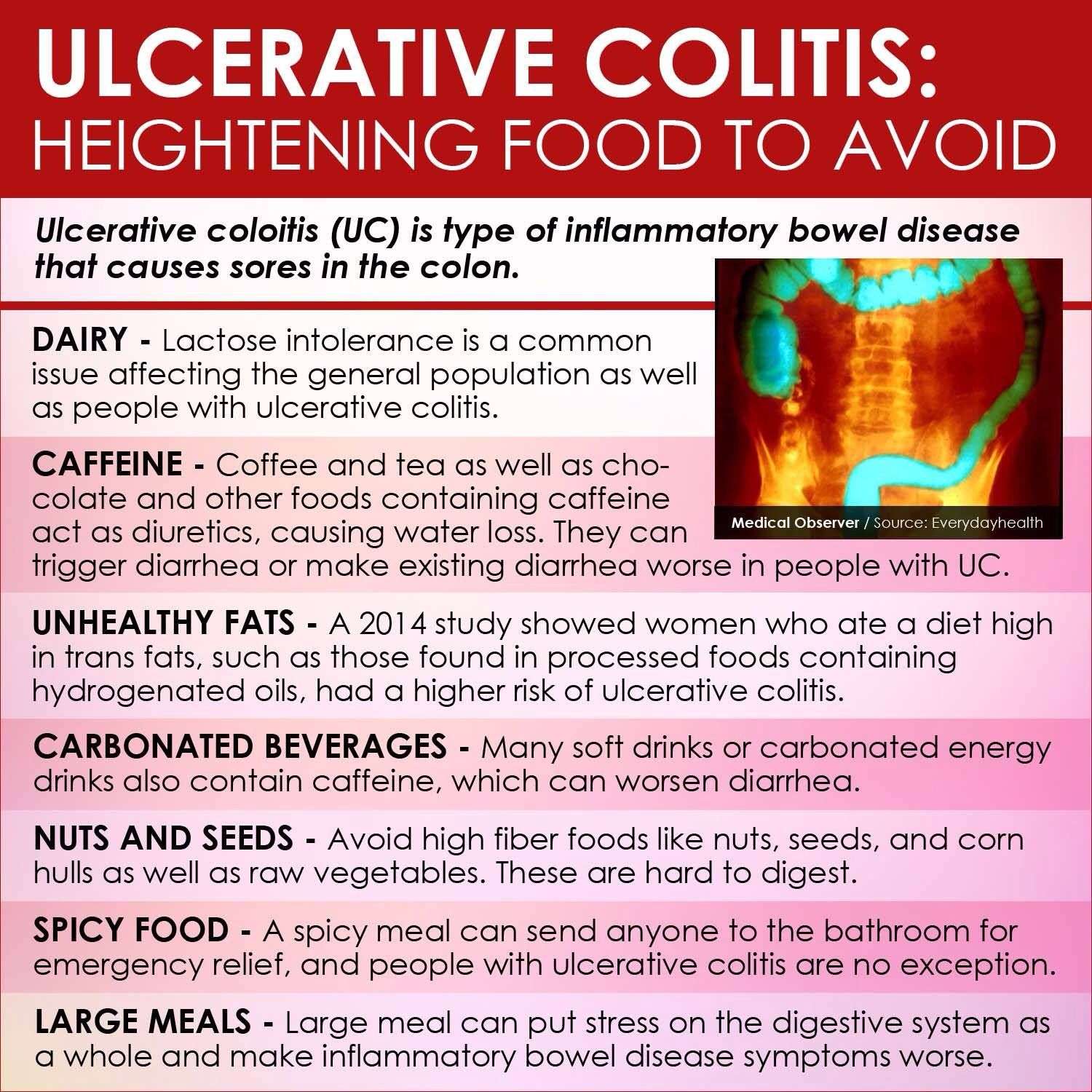
Foods To Avoid With Ulcerative Colitis
Although there are foods that are common triggers during both Ulcerative Colitis flares and remission, the list expands when youre experiencing active Ulcerative Colitis symptoms. Keep in mind that Ulcerative Colitis triggers differ from person to person, so the real key to long-term Ulcerative Colitis management is identifying what works for you. Easier said than done, right?
If youve ever searched on your own to figure out how to manage your Ulcerative Colitis, youve probably found a ton of information. The challenge is that the information on the internet can be contradicting and confusing. If youre struggling with Ulcerative Colitis, we recommend enlisting the help of a registered dietitian. They will be able to help you better understand your UC and determine what foods and behaviors most trigger your symptoms.
Remember to limit fiber when you are experiencing an Ulcerative Colitis flare. High fiber foods are part of a healthy, well-rounded diet. However, when UC symptoms are active, you may need to temporarily limit fiber intake to reduce inflammation and allow your gut to heal. High fiber foods are harder to digest and can trigger UC symptoms. High fiber foods include whole grains, fruits with skin and seeds, vegetables with skin and seeds, raw vegetables, cruciferous vegetables, nuts, seeds, beans and legumes.
Read Also: 5 Asa Drugs Ulcerative Colitis
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient.
Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high-calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAP stands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have an intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Dietary choices do not cause ulcerative colitis, but certain foods can trigger and worsen symptoms. Learning to identify trigger foods can help reduce the frequency and severity of ulcerative colitis symptoms.
Can Ulcerative Colitis Cause Me Constipation
Some individuals with Ulcerative Colitis experience constipation. No matter which symptoms you experience, learn how to prevent and treat your Ulcerative Colitis constipation before it affects your quality of life.
In general, Ulcerative Colitis causes inflammation in the large intestine and the rectum. When the inflammation associated with UC is concentrated in the rectum, you are likely to feel constipated. This happens because the inflammation in the rectum makes it difficult to pass stool out of your body. This form of Ulcerative Colitis is called proctitis. For individuals with proctitis, constipation may be accompanied by bleeding and a sense of urgency that are usually experienced with diarrhea. However, because the inflammation associated with proctitis is concentrated to the rectum the large intestine can successfully absorb water, which prevents diarrhea.
- Association / Trigger with other Gastrointestinal Symptoms: including gas and stomach pain, which may further complicate Ulcerative Colitis.
Read our full discussion of Ulcerative Colitis and constipation here.
You May Like: Ulcerative Colitis Medication Not Working