Ulcer Aids Sheets Boots Socks And Heel Protectors
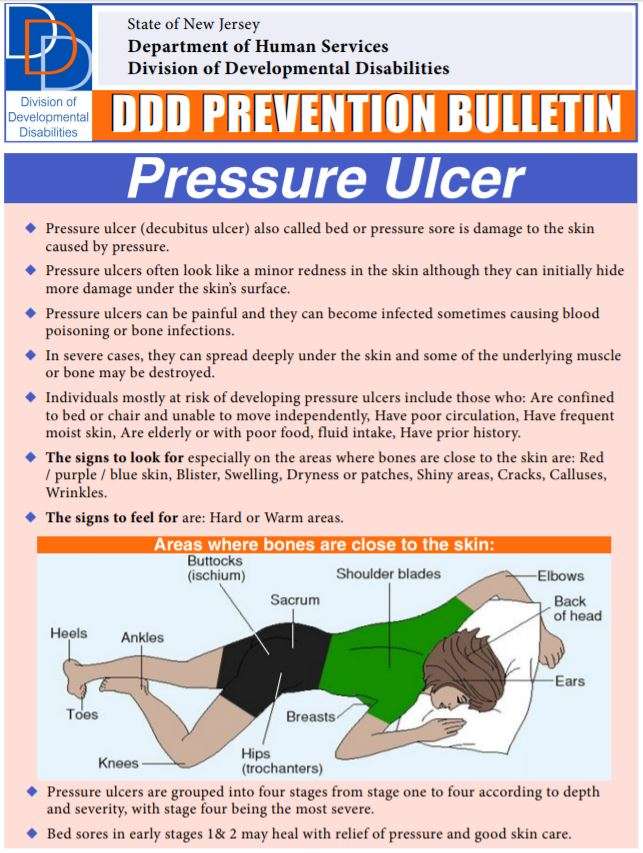
Ulcer Aids: Pressure ulcers are areas of injured skin that remain in the same position for too long. Continuing education for pressure ulcer prevention: Taking the pressure off!
They commonly form where the bones are closer to the skin, such as the ankles, heels and hips.
The risk is greater if you are confined in a bed, you use a wheelchair or you can not change positions.
Pressure ulcers can cause serious infections, some of which can be life-threatening.
They can be a problem for people in specialized care centers.
This is one of the most common health problems we face in our daily work.
The Repose Foot/heel Protector
Repose foot protectors are designed specifically to minimise the risk of pressure damage to heels. They come in the form of splints made of Platilon, a polyurethane material with unique stretch, thermal and vapour-permeable properties. They are most effective when the patient is recumbent, semirecumbent or upright while on bed-rest, as the heels are supported above a void and therefore close to zero pressure, while the malleoli are protected by air-filled compartments.
The foot protectors are inflated using a hand-help pump. A valve ensures they are inflated to the correct pressure with no chance of over-inflation. This provides a pressure-reducing splint where the weight of the lower leg is redistributed over a wider area.
Where To Get Help
- Hospital staff
- Domiciliary care staff
- Ricci JA, Bayer LR, Orgill DP. Evidence-Based Medicine: The Evaluation and Treatment of Pressure Injuries, Plast Reconstr Surg. 2017 Jan 139:275e-286e
- Walia GS, Wong AL, Lo AY, Mackert GA, Carl HM, Pedreira RA, et al. Efficacy of Monitoring Devices in Support of Prevention of Pressure Injuries: Systematic Review and Meta-analysis. Adv Skin Wound Care, 2016 Dec 29:567-574
- Wound, Ostomy and Continence Nurses Society-Wound Guidelines Task Force, WOCN 2016 Guideline for Prevention and Management of Pressure Injuries : An Executive Summary. J Wound Ostomy Continence Nurs. 2017 May/Jun 44:241-246
- Scafide KN, Narayan MC, Arundel L. Bedside Technologies to Enhance the Early Detection of Pressure Injuries: A Systematic Review, J Wound Ostomy Continence Nurs. 2020 Feb 13.
- Munoz N, Posthauer ME, Cereda E, Schols JMGA, Haesler E. The Role of Nutrition for Pressure Injury Prevention and Healing: The 2019 International Clinical Practice Guideline Recommendations. Adv Skin Wound Care, 2020 Mar 33:123-136.
- Qigui X, Qinling Y, Huapeng L. Meta-analysis of effect of foam dressing and hydrocolloid dressing on bedsore management. Chinese Nurs Res. 2017 31:3397-3400.
- Westby MJ, Dumville JC, Soares MO, Stubbs N, Norman G. Dressings and topical agents for treating pressure ulcers. Cochrane Database Syst Rev. 2017 6.
Recommended Reading: Worst Foods For Stomach Ulcers
Questions For Your Doctor
- What should I do if I or a loved one has pressure sores and is too heavy to move?
- Does an adjustable bed help reduce the risk of pressure sores?
- Can you die from an infected pressure sore?
- Is diabetic foot ulcer the same as a pressure sore?
- Can you get pressure sores from sitting in the same position in your job for longer than 2 hours at a time?
Use Pillows Cushions Or Special Mattresses
Using pillows or cushions as soft buffers between your skin and the bed or chair can be helpful. No two skin surfaces should rest against each other, eg, while lying in bed, place a pillow between your knees and ankles to prevent them from touching each other. If you are confined to bed, ask your healthcare provider about the use of heel and knee protectors or pressure relieving mattresses.
You May Like: Can Ulcers In The Colon Be Cancerous
What Are The Causes Of Pressure Injuries
Pressure injuries are caused when a force is applied to the skin, causing damage to the tissue. Several types of force include:
- Pressure: Constant pressure on the skin results from remaining in the same position for a prolonged period of time.
- Shear: Shear damage or a dragging force can occur when the head of the bed is raised and the body slides down. The skin sticks to the sheets, but internal structures are damaged.
- Moisture: Fluids that remains on the skin can cause the skin to become overly wet, which increases the risk for pressure injury development.
Treating And Preventing Pressure Ulcers
Treatment for pressure ulcers includes the use of dressings, creams and gels designed to speed up the healing process and relieve pressure. Surgery is sometimes recommended for the most serious cases.
For some people, pressure ulcers are an inconvenience that require minor nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning or gangrene.
Read more about the complications of pressure ulcers.
Pressure ulcers can be unpleasant, upsetting and challenging to treat. Therefore, a range of techniques is used to prevent them developing in the first place. These include:
- regularly changing a person’s position
- using equipment to protect vulnerable parts of the body such as specially designed mattresses and cushions
Read about treating pressure ulcers and preventing pressure ulcers for more information.
Unfortunately, even with the highest standards of care, it’s not always possible to prevent pressure ulcers in particularly vulnerable people.
Read Also: What To Take For Stomach Ulcer Pain
Preventing Pressure Ulcers In Hospitals
Each year, more than 2.5 million people in the United States develop pressure ulcers. These skin lesions bring pain, associated risk for serious infection, and increased health care utilization. The aim of this toolkit is to assist hospital staff in implementing effective pressure ulcer prevention practices through an interdisciplinary approach to care.
Prepared by: Dan Berlowitz, M.D., M.P.H. Bedford VA Hospital and Boston University School of Public Health Carol VanDeusen Lukas, Ed.D. VA Boston Healthcare System and Boston University School of Public Health Victoria Parker, Ed.M. D.B.A. Andrea Niederhauser, M.P.H. Jason Silver, M.P.H. and Caroline Logan, M.P.H. Boston University School of Public Health Elizabeth Ayello, Ph.D., RN, APRN, BC, CWOCN, FAPWCA, FAAN, Excelsior College School of Nursing, Albany, New York and Karen Zulkowski, D.N.S., RN, CWS, Montana State University-Bozeman.
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
Recommended Reading: Ulcerative Proctitis Vs Ulcerative Colitis
Why Do I Have Pressure Ulcers On My Feet And Ankles
Pressure sores on the feet and ankles are caused by pressure that limits blood flow through the skin in the affected area. This often occurs in people who are less mobilefor example, people who are bedridden or confined to wheelchairs.
Pressure from the weight of the affected person against the bed or the surface of a wheelchair can cause pressure ulcers.
Automatic Lateral Turning Systems
Within pressure care management, user turning, position and repositioning plays a key role in the prevention of pressure ulcers and their treatment. A turning plan is essential for the well-being of persons who are cared for around the bed, especially for those with a high risk of pressure damage or who have limited mobility. Effective positioning should be carried out every 2 to 4 hours depending on the nature of the circumstances such as skin condition, mobility, and other factors.
Automatic lateral turning systems are a highly effective way in the management and treatment of pressure ulcer development. Turning systems allow the user to be automatically repositioned for effective pressure relief and eliminate the need for manual turning. They ensure users are turned safely and correctly, which contributes to improves wellbeing and esteem and greater efficiency within care settings.
As there is no need for manual turning, care givers are not at risk of injury to their neck, back or shoulders. Meanwhile, users are not being disrupted during the night to be turned.
Recommended Reading: Hind Gut Ulcers In Horses Symptoms
Diet And Lifestyle Changes To Avoid Pressure Sores
Changes to avoid pressure sores include:
- Make sure you eat a healthy and nutritious diet. This includes a balanced diet and fluids/water. And if necessary,youre your doctor about vitamin and nutritional supplements .
- Low body weight or being overweight can cause pressure sores, so make sure you maintain heathy body weight
- If youre malnourished or at risk of malnutrition, protein, fluid and energy intake should be increased.
- Be aware of using good hygiene practices.
- Maintain activity levels, where appropriate.
- Make sure you quit smoking.
Older Signs Of A Pressure Ulcer
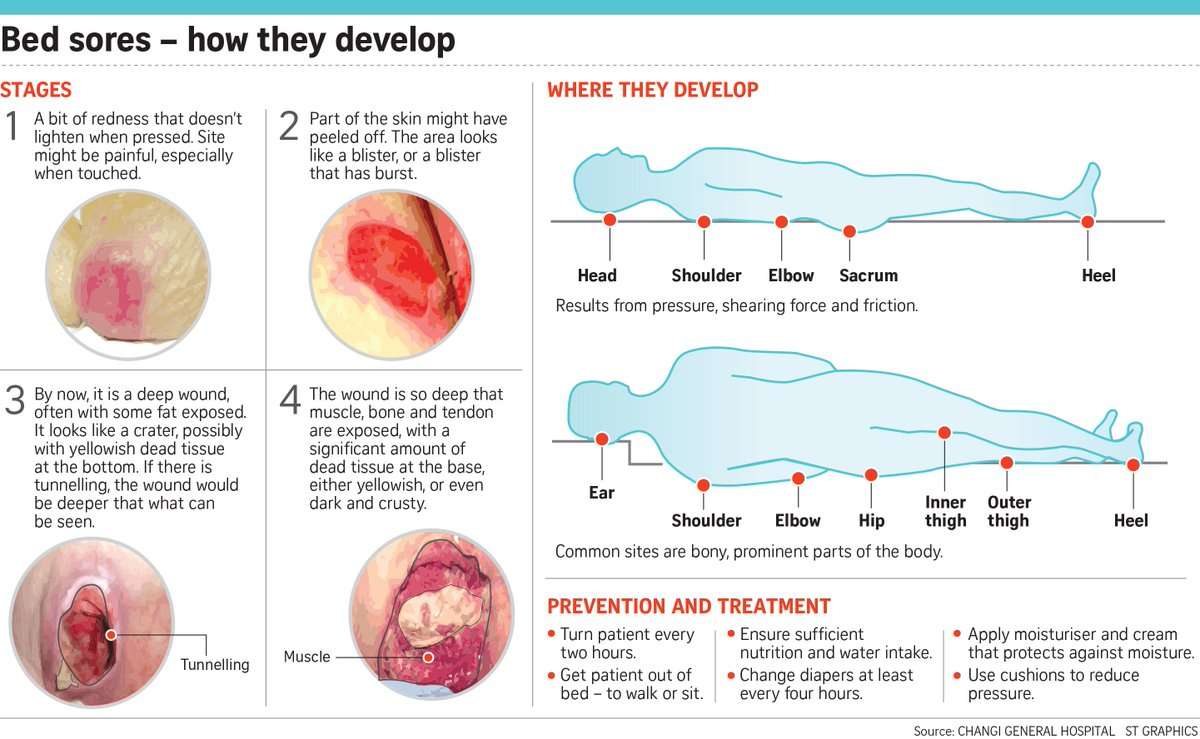
If a pressure ulcer is left untreated, it will worsen and has the potential to seriously affect a persons health, wellbeing and delay their recovery/wound healing. Even if the skin is not broken at first, when a pressure ulcer gets worse it can form into a higher category which become more painful and a longer recovery.
Category 2 An open wound or blister, sometimes can look like filled with clear liquid Painful to touch and tender Can look like a scrape , blister, or a shallow crater in the skin Partial thickness skin loss Recovery time: 3 days to 3 weeks
Category 3 A deep wound that reaches the deeper layers of the skin Wound tunnelling and odour Recovery time: 1 month up to 4 months
Category 4 Very deep wound that may expose tendons, muscle, or bone Skin has turned black and shows signs of infection Red edges, pus, odour, heat, and/or drainage Recovery time: From 3 months and possibly longer
Read Also: Peptic Ulcer Food To Eat
How Can Pressure Injury Be Prevented
Ways to prevent pressure injuries include:
What Bundle Of Best Practices Do We Use
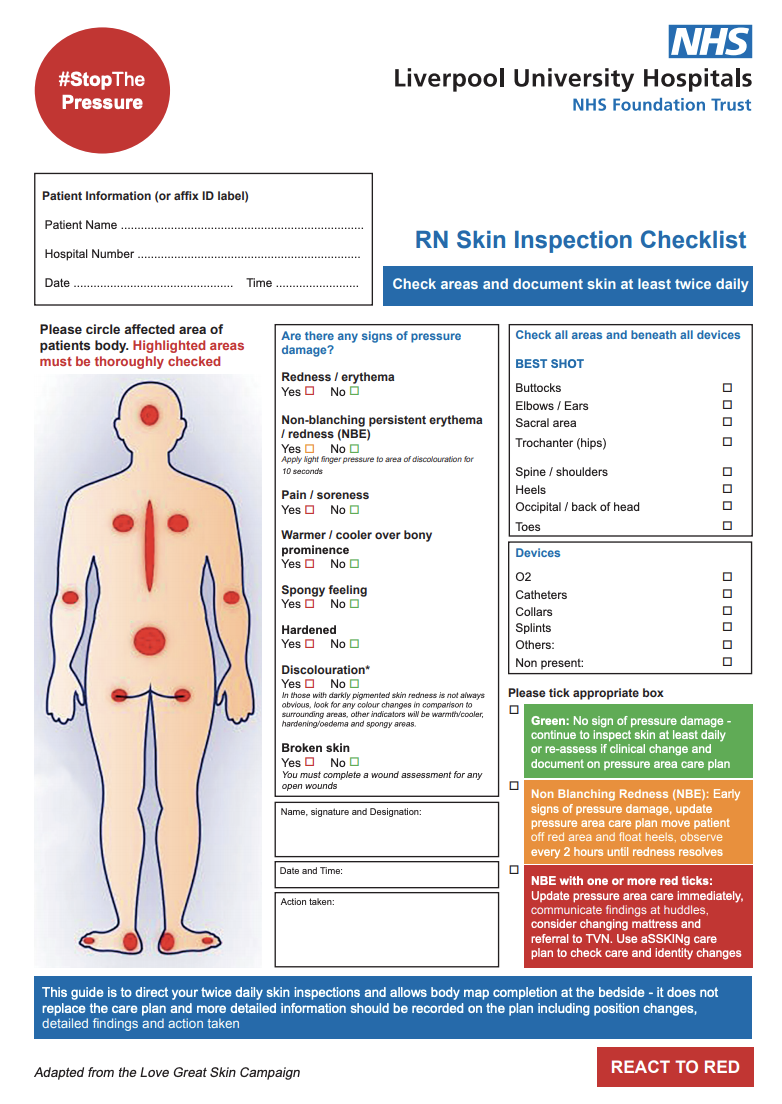
Given the complexity of pressure ulcer prevention, with many different items that need to be completed, thinking about how to implement best practices may be daunting. One approach that has been successfully used is thinking about a care bundle. A care bundle incorporates those best practices that if done in combination are likely to lead to better outcomes. It is a way of taking best practices and tying them together in a systematic way. These specific care practices are among the ones considered most important in achieving the desired outcomes.
The pressure ulcer bundle outlined in this section incorporates three critical components in preventing pressure ulcers:
- Comprehensive skin assessment.
- Standardized pressure ulcer risk assessment.
- Care planning and implementation to address areas of risk.
Because these aspects of care are so important, we describe them in more detail in the subsequent subsections along with helpful clinical hints. While these three components of a bundle are extremely important, your bundle may stress other aspects of care. It should build on existing practices and may need to be tailored to your specific setting. Whatever bundle of recommended practices you select, you will need to take additional steps. We describe strategies to ensure their successful implementation as described in Chapter 4.
The challenge to improving care is how to get these key practices completed on a regular basis.
Resources
Also Check: Can Diet Help Ulcerative Colitis
Nursing Diagnosis Impaired Skin Integrity Related To Pressure Ulcer
Ineffective peripheral Tissue Perfusion Pressure Ulcers occur when skin is in prolonged contact with an underlying bony prominence or other fixed objects. This can be due to improper positioning or activity restrictions. They are usually more severe than stage I and II pressure ulcers and can be dangerous if not treated properly. Pressure Ulcers are open wounds and should be cleaned regularly with mild soap, rinsed with clean water, and dried thoroughly.
Diagnosis Of A Decubitus Ulcer
Wound care physicians and nurses experienced in pressure ulcers are often consulted for decubitus ulcer diagnosis. Medical personnel may take samples of the pressure ulcer tissue and fluid to look for bacteria or cancer. They may also do blood cultures, bone scans or other tests depending on the seriousness of the ulcer. In addition, they will evaluate the condition of the ulcer according to:
- The size of the decubitus ulcer and depth of the crater
- What kind of tissue is affected by the ulcer: skin, bone, or muscle
- The color of the ulcer and skin around it
- The tissue death caused by the ulcer
- The presence of infection, bleeding or foul odor
Read Also: What Does Asacol Do For Ulcerative Colitis
What Tests Diagnose A Peptic Ulcer
To confirm a person has an ulcer a diagnostic imaging test will usually be ordered. The two most widely used tests are:
- Upper GI series : This is a type of X-ray. The patient is given a chalky liquid to drink that increases the contrast on the X-ray, making certain features easier to see. Because this liquid contains barium, this test is sometimes called a barium swallow.
- Endoscopy : An endoscope is a thin, flexible tube with a tiny camera at the end. The patient is given a mild sedative, and then the tube is passed through the mouth into the stomach. The doctor can see the lining of the stomach to diagnose a peptic ulcer. Tiny samples of the tissue will be taken , which are examined under a microscope.
If a diagnostic imaging test reveals an ulcer, the patient will most likely have a test to see if H pylori bacteria are present.
- It is important to be certain about this, because treatment of the H pylori is likely to heal the ulcer.
- Ulcers caused by H pylori are treated differently than ulcers caused by medications.
Three types of tests are available to detect H pylori.
Dont Miss: Why My Stomach Feels Full All The Time
How Do You Prevent Pressure Ulcers
Dr. Madhuri Reddy, from the Harvard-affiliated Hebrew Rehabilitation Center in Boston led a research paper into preventing bed sores which was published in the Journal of the American Medical Association in 2006. Her numerous studies found Given current evidence, using support surfaces, repositioning the patient, optimizing nutritional status, and moisturizing sacral skin are appropriate strategies to prevent pressure ulcers. So lets break this down a little more to find out how each can be achieved:
- Repositioning the study found that this is probably one of the most effective actions to take to prevent bed sores. If they are created through lack of movement causing a limit of blood supply to the skin, then frequent turning or repositioning of the patient is a good method of prevention. So that patients can remain in position the carer places them in,foam wedges for positioningare used to support the body. The best positioners for bedridden patients are made from high density orthopedic support foam that does not crush under weight, are curved to contour to the body for added comfort and have a wide buttress for added strength. The caregiver needs to be safe in the knowledge that the position they place their patient in is where they will stay.
Sources:
Read Also: How To Cure Tongue Ulcer
Students Who Viewed This Also Studied
eduaction quality of life 214.pdf
St. Johns University
PHD212 Powders Calculation discussion .pdf
St. Johns University
Introduction to semi solid dosage forms C.pdf
St. Johns University
Dashboard and Health Care Benchmark Evaluation.docx
St. Johns University
St. Johns University HSA NURSING RE
eduaction quality of life 214.pdf
St. Johns University HSA NURSING RE
PHD212 Powders Calculation discussion .pdf
St. Johns University HSA NURSING RE
Introduction to semi solid dosage forms C.pdf
St. Johns University HSA NURSING RE
Dashboard and Health Care Benchmark Evaluation.docx
St. Johns University HSA NURSING RE
Case 1.docx
St. Johns University HSA NURSING RE
Dashboard Benchmark Evaluation.docx
Upload your study docs or become a
Course Hero member to access this document
Upload your study docs or become a
Course Hero member to access this document
You May Like: How To Get Remission In Ulcerative Colitis
What Is A Pressure Ulcer
A pressure ulcer, also referred to as a pressure sore or bed sore, is damage caused to the skin and underlying tissue, primarily caused by prolonged pressure on the skin. Pressure ulcer development can happen to anyone, however typically they usually affect those who are confined to a bed or sit for long periods of time in a chair or wheelchair.
You May Like: What Does A Foot Ulcer Look Like
What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
The Importance Of Pressure Ulcer Prevention
Pressure ulcers are caused if the blood supply to the skin and the underlying tissues is compromised for prolonged periods of time due to mechanical compression of the local vasulature, with ensuing hypoxia and tissue necrosis. Most of the time, pressure ulcers significantly impact the patients morbidity, mortality and quality of life.
In some cases, these occur quickly – between the first hour and 4 to 6 hours after sustained loading.
Depending on population and ulcer grade, up to 50 percent of pressure injuries can be avoided.
Furthermore, research has proven that the costs of pressure ulcer treatment exceed those of prevention by 2.5 times.
Also Check: Ulcer In My Stomach Symptoms