C Diff Infection And The Effect On Ulcerative Colitis
C. diff infection is one of the most common complications to watch for if you have ulcerative colitis. It can happen even if you are not taking antibiotics, especially if you take steroid medications to keep the disease under control. A database of patients with IBD showed 10% will have at least one C. diff infection over the course of their lifetime. Half will have more than one.
When people with ulcerative colitis get a C. diff infection, they are more likely to need a colectomy, an operation to remove part or all of the colon. They also have a higher risk of developing complications after surgery, and they have a higher death rate.
A Mutually Beneficial Relationship
Dr. Ost highlighted that the relationship between C. albicans and its human hosts was potentially beneficial for both parties.
We found that the benefits are mostly from the clearance of the invasive form of this fungus. However, recent studies suggest that these fungi may help our body fight off infection by promoting protective immune responses, she said.
Gerard Honig, Ph.D., the director of research innovation at the Crohns & Colitis Foundation, which helped fund the new research, welcomed the findings:
Although treatments for IBD are available, they have major limitations. There is a critical need for therapeutic strategies that directly target and modulate the dysregulated interactions between the microbiome and the immune system that cause these diseases.
Dr. Honig said that several lines of evidence suggest that fungi play an important role in IBD, particularly Crohns disease.
He pointed out that blood tests for antibodies against microbes, including fungi, have been used for years to help in the diagnosis of Crohns and to determine patients prognosis.
However, the functional significance of antifungal immune responses in IBD has been unclear, and this question is elegantly addressed in this new work, he said.
Dr. Honig emphasized that more work would be needed to confirm and extend the findings before proceeding to clinical trials of potential new treatments.
Why Do I Often Get Thrush
Those most vulnerable to thrush: patients with compromised immune systems, older populations, infants as well.1Prednisone may also be a factor in thrush, as well as weakened immunity, vaginal yeast infections, some medications, and dentures.
You can help prevent oral thrush by maintaining good oral health and washing/swishing your mouth out VERY well after using inhalers if you use them for another medical condition.2
You May Like: How To Lose Weight With Stomach Ulcers
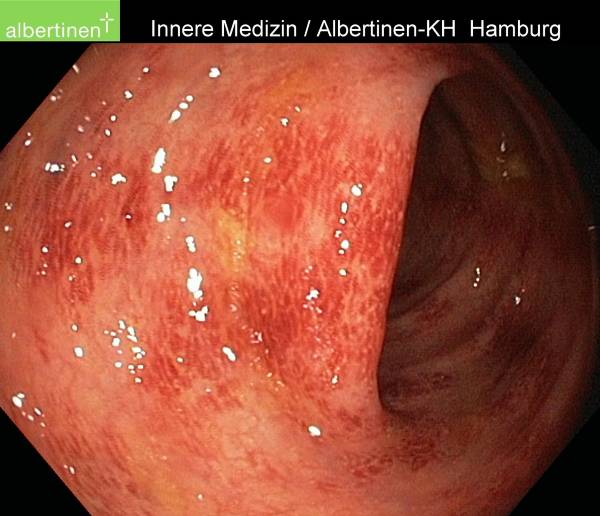
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Yeast Infections And Colitis
Hey UCers,
I need your help.
Yesterday I received an email from a concerned UCer who has been having an awful lot of trouble with chronic yeast infections. This is a topic that has not been discussed in any detail so far on the site, but Im really hoping that some of you might be able to shed some light on the subject and in turn help out the person who emailed me.
Below is the message that I received and if you have any input or ideas, please leave a comment. Hopefully, together, we can get to the bottom of this.
Hi Adam,
I have a question for you and I havent been able to find anything on your website regarding ithave you ever spoken to any females diagnosed with UC who began having chronic yeast infections shortly thereafter? I have had chronic yeast infections since shortly after my diagnosis seven years ago and have been to several doctors to try to figure out the cause. Ive been checked for everything under the sun and most recently went to a functional medicine doctor who did a stool test. It was found at the time that I do not have any elevated levels of yeast.
While researching online I found blogs in which a couple people, who also have chronic yeast infections, talked about the connection between yeast and sulfur drugs. When I was diagnosed, I was immediately treated with prednisone and sulfasalazine.
My gastro says theyre not related, however, I beg to differ. This is really frustrating and Im getting nowhere with doctors.
Thanks!
-Adam Scheuer
Don’t Miss: How Do You Treat An Ulcer Naturally
Other Women Can Be A Major Source Of Support
Talking to other women whove gone through what youre experiencing can be invaluable, says Bellaguarda. For instance, if youre in your 20s and facing surgery, and youre worried about how it may impact your life, talking to a woman who faced similar challenges at your age may be helpful.
Ask your provider if they have patients who have gone through this who may be willing to share their story with you, says Bellaguarda. Or, if that isnt possible, seek a support group.
Its good to hear from someone who has gone through this at your age to see how they feel about it.
Fungal Microbiome In Inflammatory Bowel Disease: A Critical Assessment
1F. Widjaja Inflammatory Bowel and Immunobiology Research Institute,
2Division of Gastroenterology, Department of Medicine, and
3Research Division of Immunology, Department of Biomedical Sciences Cedars-Sinai Medical Center, Los Angeles, California, USA
Address correspondence to: David M. Underhill, F. Widjaja Inflammatory Bowel and Immunobiology Research Institute, Cedars-Sinai Medical Center, 8700 Beverly Boulevard, Los Angeles, California 90048, USA. Email:
Find articles byUnderhill, D.in: |PubMed ||
1F. Widjaja Inflammatory Bowel and Immunobiology Research Institute,
2Division of Gastroenterology, Department of Medicine, and
3Research Division of Immunology, Department of Biomedical Sciences Cedars-Sinai Medical Center, Los Angeles, California, USA
Address correspondence to: David M. Underhill, F. Widjaja Inflammatory Bowel and Immunobiology Research Institute, Cedars-Sinai Medical Center, 8700 Beverly Boulevard, Los Angeles, California 90048, USA. Email:
J Clin Invest.
- Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Copyright: © 2022, Underhill et al. This is an open access article published under the terms of the Creative Commons Attribution 4.0 International License.
Reference information: J Clin Invest. 2022 132:e155786.https://doi.org/10.1172/JCI155786.
You May Like: What Should You Eat When You Have Ulcerative Colitis
Crohns Disease Ulcerative Colitis And Candida Whats The Connection
Crohns disease, ulcerative colitis, and candida share a common origin inflammation. One of the main reasons why candida is associated with more than 100 medical conditions and diseases is because of its ability to trigger chronic inflammation within the body.
Crohns disease and ulcerative colitis are both autoimmune diseases. When you have an autoimmune disease, this generally indicates that your immune cells are baffled and they have begun to attack your own tissue. The attack itself is always accompanied by inflammation. In Crohns disease, the most common area where the autoimmune attack takes place is somewhere towards the end of the small intestine or the beginning of the large intestine. In ulcerative colitis, the autoimmune attack occurs in more specific areas of the gastrointestinal tract, such as only the small intestine or only the large intestine.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
You May Like: Can Ulcerative Colitis Cause Fever
How Does C Diff Spread
C. diff is everywhere â in the environment â and in the intestines of many people. Your gut has trillions of microorganisms, including bacteria, fungi, and viruses. Most healthy people have a good balance of âhelpfulâ intestinal bacteria and harmful bacteria, including C. diff. If anything happens to mess up the balance in the gut, the harmful bacteria can spread.
Antibiotics are one cause of such an imbalance. Antibiotics kill harmful bacteria but also kill helpful bacteria. Another cause is ulcerative colitis. Upsetting the balance can allow C. diff to grow and release toxins that attack the intestinal wall.
C. diff infections spread easily, most often in hospitals, long-term care facilities, and other buildings where people are sick or in a weakened state. If a patient or resident has C. diff in their stool and if they or their caregiver donât wash their hands really well, they can leave the bacteria on anything they touch. Someone else then touches the contaminated surface. When they touch their face or prepare food without washing their hands properly, the bacteria can enter their body or spread to others.
While most people who get C. diff infections are in health care facilities, it is different for people with inflammatory bowel disease â the umbrella term for ulcerative colitis and Crohnâs disease. About 75% of people with IBD get C. diff from their community.
Things That Can Help With Thrush:
- Yogurt drinks – Chobani has some delicious yogurt drinks in many different flavors and I cant stress enough how much I live on these during the weeks I have thrush. Sometimes its all Im able to get into my body.
- There is also a very helpful resourceful diet that helps many patients who deal with chronic thrush called the candida diet.3
You dont have to go through the pain of thrush alone. So often many of us on steroids and inhalers deal with it, and it doesnt get easier until you know what you should be avoiding and what you should be putting into your body to make your mouth and throat feel better. It took my years to learn that soda and natural sugars were making my mouth completely worse and so much more painful than it had to be.
If you struggle with thrush, talk to your doctor to discuss your symptoms and how often youre getting it. Consider getting rid of the substances youre putting into your body that may be making the thrush worse.
You May Like: What Can I Drink With Ulcerative Colitis
Extraintestinal Manifestations And Complications
UC is characterized by immune dysregulation and systemic inflammation, which may result in symptoms and complications outside the colon. Commonly affected organs include: eyes, joints, skin, and liver. The frequency of such extraintestinal manifestations has been reported as between 6 and 47%.
UC may affect the mouth. About 8% of individuals with UC develop oral manifestations. The two most common oral manifestations are aphthous stomatitis and angular cheilitis. Aphthous stomatitis is characterized by ulcers in the mouth, which are benign, noncontagious and often recurrent. Angular chelitis is characterized by redness at the corners of the mouth, which may include painful sores or breaks in the skin. Very rarely, benign pustules may occur in the mouth .
UC may affect the eyes manifesting in scleritis, iritis, and conjunctivitis. Patients may be asymptomatic or experience redness, burning, or itching in eyes . Inflammation may occur in the interior portion of the eye, leading to uveitis and iritis. Uveitis can cause blurred vision and eye pain, especially when exposed to light . Untreated, uveitis can lead to permanent vision loss. Inflammation may also involve the white part of the eye or the overlying connective tissue , causing conditions called scleritis and episcleritis. Ulcerative colitis is most commonly associated with uveitis and episcleritis.
Q& a: Yeast Common In Cheese Processed Meats Impairs Healing In Crohns
Disclosures: We were unable to process your request. Please try again later. If you continue to have this issue please contact .
Researchers from Cleveland Clinic found an infection that prevents healing in patients with Crohns disease, according to study results published in Science.
Healio Gastroenterology spoke with Thaddeus Stappenbeck, MD, PhD, chair inflammation and immunity at Cleveland Clinic, about results from the study that examined the yeast, Debaryomyces hansenii. Investigators found higher levels of the yeast among patients with Crohns disease. The results showed D. hansenii was abundant in inflamed regions of the colon and small intestine, which may be a sign of unhealed intestinal wounds.
Debaryomyces hansenii,
Healio: What were the key results and conclusion from the study?
Healio: What were the key takeaways of the study that can be applied to patient care?
Healio: Will there be future research regarding this study?
Read Also: Bone Broth And Ulcerative Colitis
Your Doctor Wants To Hear Your Concerns
Many women are reluctant to broach the subjects of bowel movements, sex, and sex organs with their doctor, says Matro, but its important to bring your concerns out into the open.
Sometimes people feel embarrassed to talk about , says Gross. If youre hesitant to bring up a topic face-to-face, she suggests writing your concerns on the intake form used at many medical practices.
Another option, suggests Matro, is to contact your doctor in writing using a secure online messaging system. Many hospitals and practices now have such systems in place. That can trigger a response from the doctor to see you for an appointment, she says, or at least let the doctor know struggling with that problem.
Remember, Matro adds, that however odd or embarrassing your concern might seem, your doctor has probably heard it before. Youre going to be taken seriously, she says. Your doctor will want to help in any way that he or she can or will refer you to someone else if your problem would be best addressed by another healthcare professional.
Shd Exhibits Therapeutic Effects In Mice With Dss Colitis Administered C Albicans
A C. albicans colonized-UC animal model was established and described in Fig. A. C. albicans overtly aggravated UC as indicated by more pronounced body weight loss, elevated DAI and histological score, reduced colon length and more severe colonic epithelial mucosa damage compared with the DSS group . These changes were mitigated after SHD administration. Compared with the Model group, body weight loss was reduced and DAI was decreased in the SHD groups . Besides, colon lengths were increased while histological scores were lower in the SHD-H group compared with the Model group , suggesting that SHD-H had better effects than SHD-L.
Fig. 1
SHD attenuates the development of DSS colitis with C. albicans. A Experimental design of C. albicans administration in mice with colitis and SHD treatment. B Body weights. C Disease active index values. D Colon lengths. E Histological scores. F Colonic tissue samples after H& E staining . Data are mean±SD. #P< 0.05, ##P< 0.01 versus normal group *P< 0.05, **P< 0.01 versus Model group
Recommended Reading: Best Vitamins For Ulcerative Colitis
What Are C Difficile Infection Symptoms
C. diff infection symptoms begin with frequent, watery, foul-smelling bowel movements and cramps in your abdomen.
If the infection goes untreated or gets worse even after treatment, symptoms can include:
- Diarrhea or watery stool as many as 15 times a day
- Blood in the stool
- Signs of dehydration
- Swelling of the abdomen
- Rapid heartbeat
C. diff infections can cause a serious complication called Clostridioides difficile colitis, which is inflammation of the colon wall. It also can cause toxic megacolon, which damages the deeper layers of the colon. People with uncontrolled ulcerative colitis are also at increased risk for toxic megacolon. If left untreated, it can cause the colon wall to rupture, releasing bowel contents into the abdomen.
How I Know That Thrush Is Coming
Your spit is thick, you can clear your throat 100 times, but it wont feel clear. Thats my big uh-oh indicator to knowing thrush is coming for me. You cant swallow comfortably and everything hurts to eat.
Ill leave some foods to avoid based on previous GI recommendation and based on my own personal experience. Eating or drinking the wrong thing can actually irritate your infection more and feel like youre swallowing parts of a cactus.
You May Like: How Does Ulcerative Colitis Affect The Large Intestine
Your Children May Or May Not Be At Greater Risk For Uc
The risk that you will pass your IBD on to your child is between 5 and 7 percent, according to the AGA. If your partner also has IBD, the risk may increase to about 35 percent.
Whether someone will inherit UC isnt fully understood, as its likely due to a number of genetic and environmental factors, according to the U.S. National Library of Medicine.
Predictors Of Fungal Infections In Ibd
Different demographic variables were studied for prediction of Fungal infections in IBD . Age above 50 showed increased risk. The highest risk of developing fungal infection was associated with concomitant AIDS HR 5.99 . Other risk factors which showed significantly increased risk were congestive heart failure, anemia, diabetes mellitus COPD, pulmonary circulation disorders, rheumatoid arthritis/collagen vascular disease. solid organ malignancy, metastatic malignancy, lymphoma and weight loss were also found to increase the risk of opportunistic fungal infections in IBD patients.
Table 3
Also Check: Diabetic Foot Ulcer Treatment Guidelines
Inflammatory Bowel Ulcerative Colitis Linked To Intestinal Fungi
- Copy Link URLCopied!
Bacteria in the gut play a crucial role in human health, and imbalances in bacterial populations can contribute to many disorders. New research suggests that fungi, though not as common in the intestines as bacteria, may also play a role in causing and modulating disease.
The results could lead to new treatments for conditions such as inflammatory bowel disease, ulcerative colitis and Crohns disease. An estimated 1.4 million Americans have some form of inflammatory bowel disease, which can cause inflammation, ulcers in the bowel, abdominal pain, diarrhea, bleeding, fatigue, weight loss and loss of appetite. An additional 30,000 cases are diagnosed annually.
An estimated 100 trillion individual bacteria reside in the intestines — more than the number of cells in the human body. They play crucial roles, such as aiding digestion of food, producing necessary vitamins and suppressing the growth of harmful microbes.
But according to Dr. David M. Underhill of the Inflammatory Bowel and Immunobiology Research Institute at Cedars-Sinai Medical Center, there has been little corresponding study of fungi in the intestine.
Working with mice, Underhill and his colleagues looked for fungal DNA in the animals bowels. The team reported this week in the journal Science that they identified more than 100 species. We were truly stunned to see just how common fungi are, he said.
LATimesScience@gmail.com