What You Need To Know About Covid
We know youre concerned about the coronavirus. We are, too. Thats why were staying as informed as possible. Well update this page as we learn more about how this situation impacts those with IBD.
Theres a lot we dont know about COVID19, but heres a list of reliable resources of information:
Recommended Reading: Safe Desserts For Ulcerative Colitis
What Is Acid Reflux
Acid reflux also known as heartburn, pyrosis, or acid indigestion is a common problem that causes a burning pain in the lower area of the chest.
According to the American College of Gastroenterology, more than 60 million Americans experience monthly heartburn.
Acid reflux occurs when the sphincter weakens or relaxes, allowing acid to travel back up the esophagus.
Particular food aggravates acid reflux more than others.
These include alcohol, orange juice, coffee, tomatoes, grapefruits, fried foods, spicy foods, and chocolate.
In addition, you can trigger heartburn when you consume large quantities of food.
Symptoms of acid reflux include a burning pain in the chest combined with a sour taste at the back of the throat.
And these symptoms generally worsen if you bend over or lie down. Other signs of heartburn include hiccups or a cough.
If acid reflux occurs more than twice a week, a doctor may diagnose you with GERD or Gastroesophageal reflux disease.
Abdominal And Rectal Pain
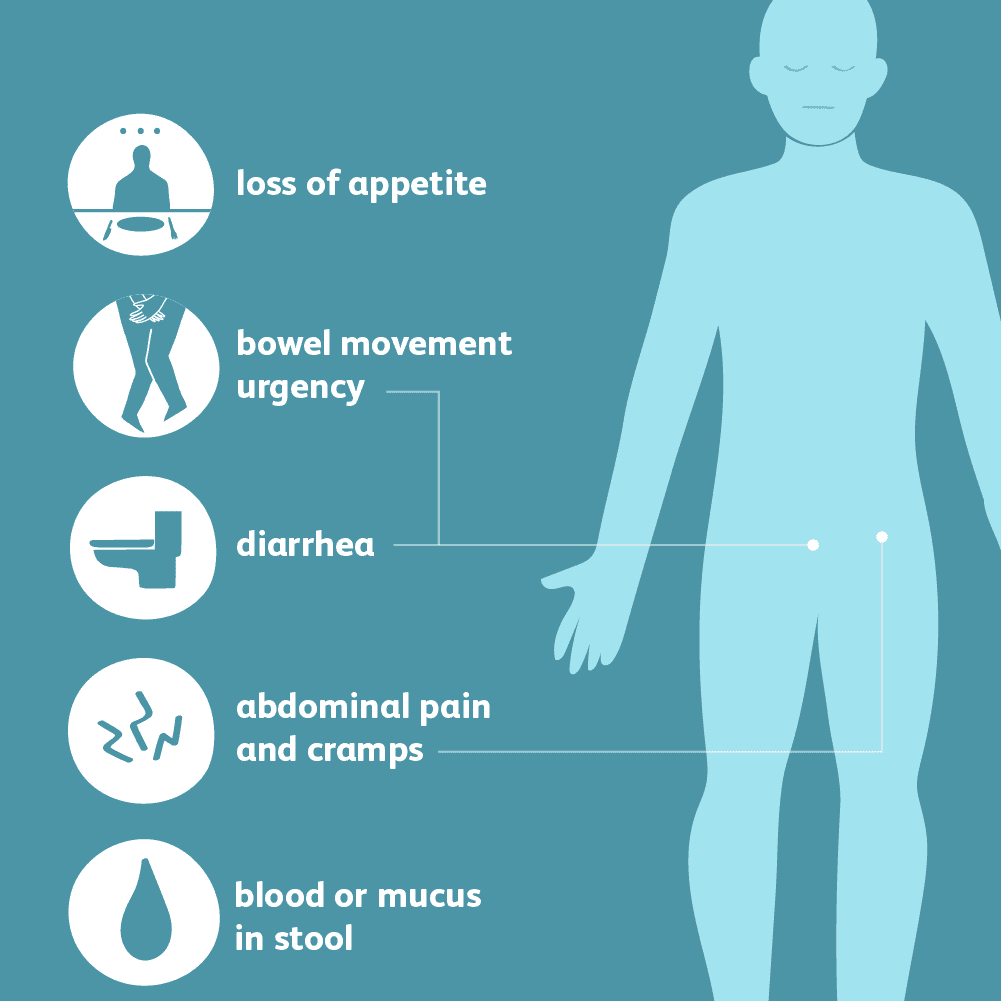
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
Also Check: What Is The Recommended Diet For Horses With Ulcers
The Difference In Extraintestinal Manifestations Of Inflammatory Bowel Disease For Children And Adults
Hyo-Jeong Jang1, Ben Kang2, Byung-Ho Choe2
1Department of Pediatrics, Keimyung University School of Medicine , 2Department of Pediatrics, School of Medicine, Kyungpook National University , South Korea
Contributions: Conception and design: All authors Administrative support: All authors Provision of study materials or patients: All authors Collection and assembly of data: All authors Data analysis and interpretation: HJ Jang, B Kang Manuscript writing: All authors Final approval of manuscript: All authors.
Correspondence to:
Abstract: Extraintestinal manifestations are frequently observed in adult and pediatric patients with inflammatory bowel disease . The most common EIMs involve the joints, skin, and eyes, but they can affect various organs and result in significant morbidity. Since EIMs can appear years before the diagnosis of IBD is made, clinicians should be aware of their various manifestations to help decrease diagnostic delay of IBD and establish appropriate treatment plans.
Keywords: Inflammatory bowel disease extraintestinal manifestations pediatric Crohns disease ulcerative colitis
Submitted Dec 22, 2018. Accepted for publication Jan 23, 2019.
doi: 10.21037/tp.2019.01.06
Consider Therapy To Help Manage Stress And Pain
Working with a therapist on certain mind-body techniques can help you control ulcerative colitis symptoms.
Cognitive behavioral therapy and a technique called biofeedback may be useful, as these processes teach skills to cope with stress and pain. In CBT, you learn to recognize and change behaviors and emotions that affect you physically. According to an article in Therapeutic Advances in Gastroenterology, CBT can ease abdominal pain for some people. Biofeedback will teach you how to identify and control some bodily processes, such as heart rate or tension in your muscles, and it can be effective in helping manage chronic pain.
You May Like: Ulcerative Colitis Rectal Pain Relief
Menstrual Cycle & Ulcerative Colitis
Women with UC, experience changes in their menstrual cycle and start to experience irregular periods or changes in their flow. The prostaglandins that cause uterine contractions and other menstrual symptoms also cause colon contraction, which in turn make the period pain more intense.
When women with UC menstruate they face an increased risk for anemia. The anemia risk is high for women with high flow. Losing a lot of blood during the flow can use up more red blood cells than the body can produce, thus reducing iron stores.
Articles On Ulcerative Colitis Overview
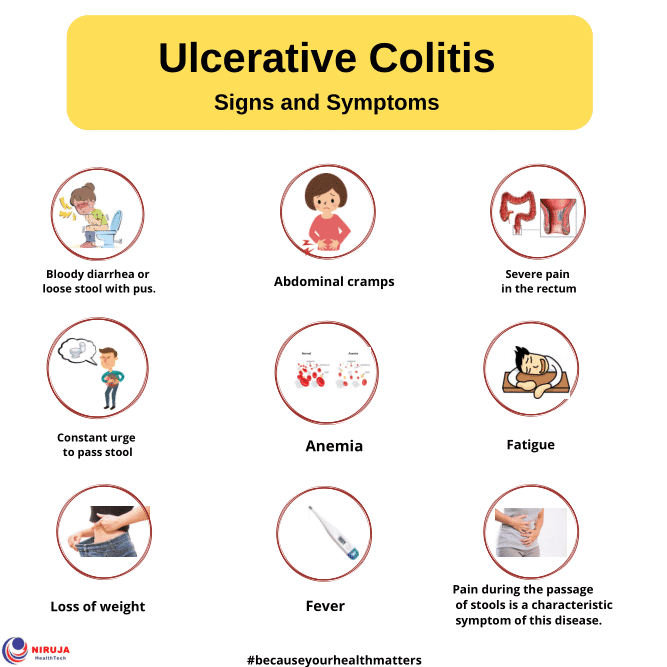
Ulcerative colitis affects your colon, which is part of your digestive system. A lot of things can cause trouble in that general area, so how do you know what it feels like to have ulcerative colitis?
It depends on how severe it is, and on what part of your colon is affected.
Also, symptoms can come and go. You might not have any for weeks, months, or even years, and then they come back. Chances are about 50-50 that the effects will be mild.
Still, most people with the disease have a few common issues:
Don’t Miss: How To Heal Mouth Ulcers
How Do You Get An Ulcerative Colitis Diagnosis
One important thing to note is that people with more severe cases of ulcerative colitis are at an increased risk of developing colon cancer and other serious health conditions, like liver disease, Rudolph Bedford, M.D., a gastroenterologist at Providence Saint John’s Health Center in Santa Monica, California, tells SELF. Thats why its important to reach out to a medical professional if you do have any of the above symptoms.
However, an ulcerative colitis diagnosis can be challenging because other conditions can mimic symptoms of IBD, like infections or even hemorrhoids, Dr. Sinha says. In terms of differentiating between Crohns and ulcerative colitis, he says, Theres no single test that we have that 100% distinguishes between the two. We rely on the patient history and other information such as radiographic imaging and endoscopy. Doing a colonoscopy, for example, can be one of the most reliable ways to identify IBD and to then distinguish between Crohns and ulcerative colitis.
While a colonoscopy is an effective tool, Dr. Sinha clarifies that its not the only way. Rather, theres an entire constellation of tests and data that can be considered, including imaging, lab tests, and a detailed intake of the patients symptoms and presentation.
How Is Ulcerative Colitis Diagnosed
Establishing a diagnosis of ulcerative colitis requires a clinic visit and medical exam with a gastroenterologist who specializes in treating patients with GI symptoms. Testing includes blood tests for anemia, elevation of inflammatory markers or signs of ongoing protein loss. Stool tests look for infections and inflammation.
If these labs or the clinical history suggest IBD, both an upper and lower endoscopy are performed. This procedure involves the use of a small flexible tube with a camera on the end to evaluate the lining of the GI tract. Pictures and tissue samples are obtained while the patients are asleep with anesthesia. These procedures look for inflamed tissue, ulceration, or sites of bleeding to confirm the diagnosis of UC.
Don’t Miss: What Are The Early Signs Of An Ulcer
Complications Of Ulcerative Colitis
UC increases your risk of developing colon cancer. The longer you have the disease, the higher your risk of this cancer.
Because of this increased risk, your doctor will perform a colonoscopy and check for cancer when you receive your diagnosis.
Repeat screenings are recommended thereafter, according to the American Cancer Society. Regular screenings help lower your risk of colon cancer. Follow-up screenings can detect precancerous cells early.
Other complications of UC include:
- thickening of the intestinal wall
- intestinal bleeding
Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
Read Also: Ulcerative Colitis Where Is The Pain
Types Of Ulcerative Colitis
UC can be categorized according to the parts of the GI tract that it affects.
- Ulcerative proctitis. In ulcerative proctitis, only the rectum is inflamed. Its considered a mild form of UC.
- Left-sided colitis. Left-sided colitis causes inflammation in the area between the splenic flexure and the last section of the colon. The last section of the colon, known as the distal colon, includes the descending colon and sigmoid colon. Left-sided colitis is also known as distal ulcerative colitis.
- Proctosigmoiditis. Proctosigmoiditis is a form of left-sided colitis. It causes inflammation in the rectum and sigmoid colon.
Different tests can help a doctor diagnose UC. UC mimics other bowel diseases such as Crohns disease. A doctor will order multiple tests to rule out other conditions.
Tests to diagnose UC often include:
Urgency To Pass A Stool
Not only will the stool consistency change if you have ulcerative colitis, but the urge to pass could hit suddenly and strongly even though nothing comes out. If you have inflammation in the rectum, you have this sense of needing to get rid of something, even though its not there, says Dr. Englander.
Read Also: Ulcerative Colitis And Colon Cancer Statistics
The Crohns Disease Diet Plan:
The internet is filled with diet plans for Crohns disease. But as we have mentioned before, there is no one-size-fits-all diet plan to cure the condition. The best treatment for those with the disease is to avoid foods that trigger the symptoms.
Not sure which foods are creating a problem? Keep a food journal and write down the foods that you eat every day. Assess how they make you feel. Do they create more digestion issue or are they well-tolerated? Following this for a few days will help you pinpoint the foods that you should be taking and avoiding.
Also Check: Foods Okay To Eat With An Ulcer
Effects Of Crohns Disease And Ulcerative Colitis
Every person responds differently to IBD. The severity of symptoms will vary from time to time and from person to person. IBD is not a progressive disease . Rather, flare-ups can range from mild to severe and back to mild again. Some people will experience periods of relief from symptoms in between flare-ups.We cannot predict how long a person will stay free from symptoms, or when their next flare-up will occur. Some flare-ups settle down quite quickly with treatment. Other times, it may take months for a persons symptoms to respond to treatment.IBD interferes with a persons normal body functions. Signs and symptoms can include:
- pain in the abdomen
Don’t Miss: Medications Used For Ulcerative Colitis
What Are The Symptoms Of Ulcerative Colitis With Constipation
Thereâs no agreed-upon definition for UC with constipation. But a group of experts came up with a set of guidelines to better pinpoint it. In general, youâll need to have at least two of the following symptoms for at least 3 days a month during the prior 3 months:
- A sensation that you canât get all your stool out
Constipation may also cause:
- A sick feeling in your stomach
The above symptoms can lead to other health issues, especially if you strain really hard when you poop. You may get:
- Hard stool that gets stuck in your rectum
Measurement Of Clinical Disease Activity
Disease activity scores were calculated using the SCCAI. This was modified to allow inclusion of patients with active proctitis, but without increased stool frequency. The modification involved altering the scores for stool frequency so that patients recording zero or one bowel movement in a day scored zero, those with 23 stools scored 1 point, those with 46 scored 2, those with 79 scored 3 and those with > 9 scored 4. To confirm the validity of this minor modification, we showed that, in patients at baseline, the SCCAI was significantly negatively correlated with the IBDQ it also correlated positively with the Baron sigmoidoscopic score .
Read Also: What’s The Difference Between Ulcerative Colitis And Crohn’s Disease
Is Almond Milk Actually Healthy
Almond milk is low calorie, lactose-free, and contains enough vitamin E to act as a solid antioxidant. Antioxidants can help reduce the risk of strokes, heart disease, and certain cancers. Some almond milk brands fortify their products with ingredients like calcium, phosphorus, magnesium, iron, and copper.
On the surface, almond milk looks really nutritious. But things might get more complex depending on what brand you pick. Some brands are full of added sugars that might not be great for your health.
Read Also: How To Stop Peptic Ulcer Pain
Medical Therapyeffectiveness And Persistence
Every type of drug, from mesalazine through steroids, immunomodulators, and biotechnological therapies, used in adult UC are also indicated in older patients with UC limitations and contraindications depend on coexisting comorbidities. There is a lack of specific studies addressing efficacy of mesalazine, steroids, especially low bioavailability steroids, or immunomodulators in the older UC population. As shown by Kochar et al. in a recent systematic review , < 1% of patients included in randomized clinical trials were 65 years. The evidence reported in literature in real-life studies concerning effectiveness of available therapies and persistence in therapy is therefore summarized in Table 2, divided into late-onset and older patients with long-standing disease .
Table 2 Effectiveness of and persistence in therapies in patients with late-onset ulcerative colitis and with long-standing UC in comparison with younger adult patients unless otherwise indicated
You May Like: Meals For People With Ulcers
You May Like: Ulcerative Colitis Symptoms Mayo Clinic
What To Eat During A Flare
Like so much else with Crohns disease, experiencing a flare is highly individual. Some people may find a few dietary adjustments are all thats needed, while others will have symptoms that prevent them from eating a normal diet for days or even weeks at a time. It takes a little detective work to discover your triggers: Use a notebook to track everything you eat, how you feel afterwards, whether or not symptoms follow, and the overall status of your disease at the time.
In general, youll probably want to avoid:
-
Foods with sugar , artificial sweetener, and sugar alcohols
-
Insoluble fiber, including fruits with skin and seeds, raw green vegetables, whole nuts, and whole grains
Some fiber may be OK during a flare, just be sure to peel, de-seed, and cook it first. A Granny Smith is a no go, for instance, but applesauce is probably alright.
Bottom line: Eat like a picky kid during a flarebland and boring are your best friends. Try these options:
You also may be able to tolerate yogurt, smoothies, protein shakes, canned fruit without added sugar, and pureed vegetable soups. Dont be afraid to experimentjust take it slow by trying a little at a time and waiting a day or two to see if symptoms develop before you have more or try something else new.
What Are The Symptoms And What Else Could It Be
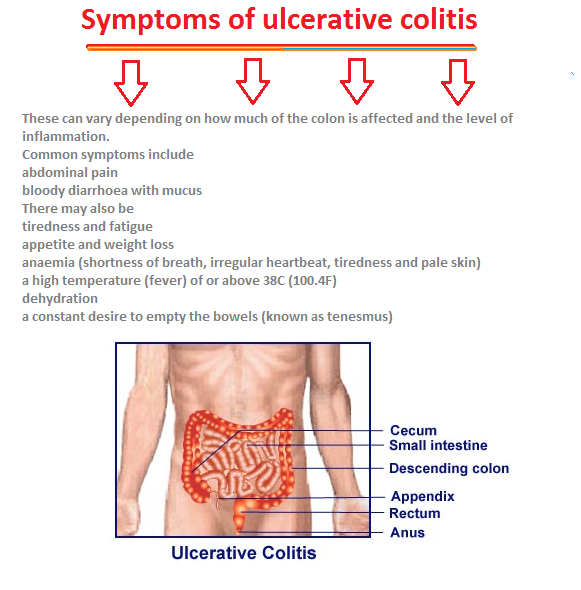
The most common symptoms of UC include diarrhea with or without blood, abdominal cramping, urgency to stool, and rectal bleeding. Sometimes children may have weight loss or poor growth over time. Other common symptoms can include fatigue, loss of appetite, and anemia caused by ongoing blood loss. Pus, mucus, and bleeding are caused when cells on the surface of the colon lining die and fall off.
Less common symptoms of ulcerative colitis include lesions, joint pain, eye inflammation, liver problems, osteoporosis, rashes, and kidney stones .
Because a variety of infections can also cause diarrhea, cramping, or sometimes blood in the stool, testing for infections is usually performed. Irritable bowel syndrome is another common cause of change of GI symptoms that must be differentiated from IBD.
You May Like: Can Alcohol Cause Stomach Ulcers
What Are Ulcerative Colitis Treatment Options
Depending on the location and severity of your case of ulcerative colitis, there are different treatments that can help you feel better. For a long time, corticosteroids were the main form of medical treatment for IBD, but they can potentially have adverse effects when used long-term. With more research, options like immunosuppressants arrived. According to the Centers for Disease Control and Prevention , the newest type of medication approved for the treatment of IBD is biologics. These medications are made from living thingsrather than chemical compoundsand work to target proteins made by the immune system to reduce inflammation. If medication isnt effective, surgery is also an option.
Dr. Sinha emphasizes that keeping your health care team informed is key to managing ulcerative colitis. Having this regular communication helps facilitate labs, imaging, or endoscopy that may be necessary, he says. It also allows the providers to understand many other facets of the disease’s impact on the patient, such as the psychosocial impact.
Inflammatory Bowel Disease: Extraintestinal Manifestations
Extraintestinal manifestations of inflammatory bowel disease can complicate treatment regimens and reduce patient quality of life. An understanding of the clinical presentations and treatment options for this disease may aid in improving patient outcomes, according to an article published in Gastroenterology.
Unlike extraintestinal complications of IBD, EIMs are not a sequela of intestinal inflammation, and may present before or after the development of gastrointestinal symptoms. Evidence suggests the likelihood of developing EIMs is tied to genetic variants and smoking. The presence of EIMs is common in both ulcerative colitis and Crohn disease. The relationship between EIMs and immune system response, as well as microbiota, is hypothesized but requires more research.
Musculoskeletal EIMs, affecting up to 46% of patients with IBD, are the most prevalent type. Categorized within the spondyloarthritis family, there may be axial or peripheral involvement. Treatment of the underlying IBD often improves musculoskeletal EIMs, though symptoms may persist despite adequate control of intestinal inflammation.
Cutaneous, ocular, and hepatobiliary EIMs are present in up to 15%, 7%, and 5%, of patients with IBD, respectively. Episcleritis, a common ocular EIM, is closely tied to intestinal inflammation and treatment of the underlying IBD is key. Other manifestations, such as the cutaneous EIM pyoderma gangrenosum, require treatment independent of IBD control.
Reference
You May Like: Ulcerative Colitis Shortness Of Breath