Patient And Public Involvement
All the patients were recruited from the outpatient clinic. Their experiences and related clinical needs drove the research question, and no patients were involved in the study design, recruitment, conduct or analysis. The results were released to study participants after the clinical trial. The aggregate data will be made publicly available. During the examination, we found that some UC patients may have been misdiagnosed therefore, those patients were not included in the UC prognosis analysis. In this study, the patients evaluated the burden of the intervention by themselves.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
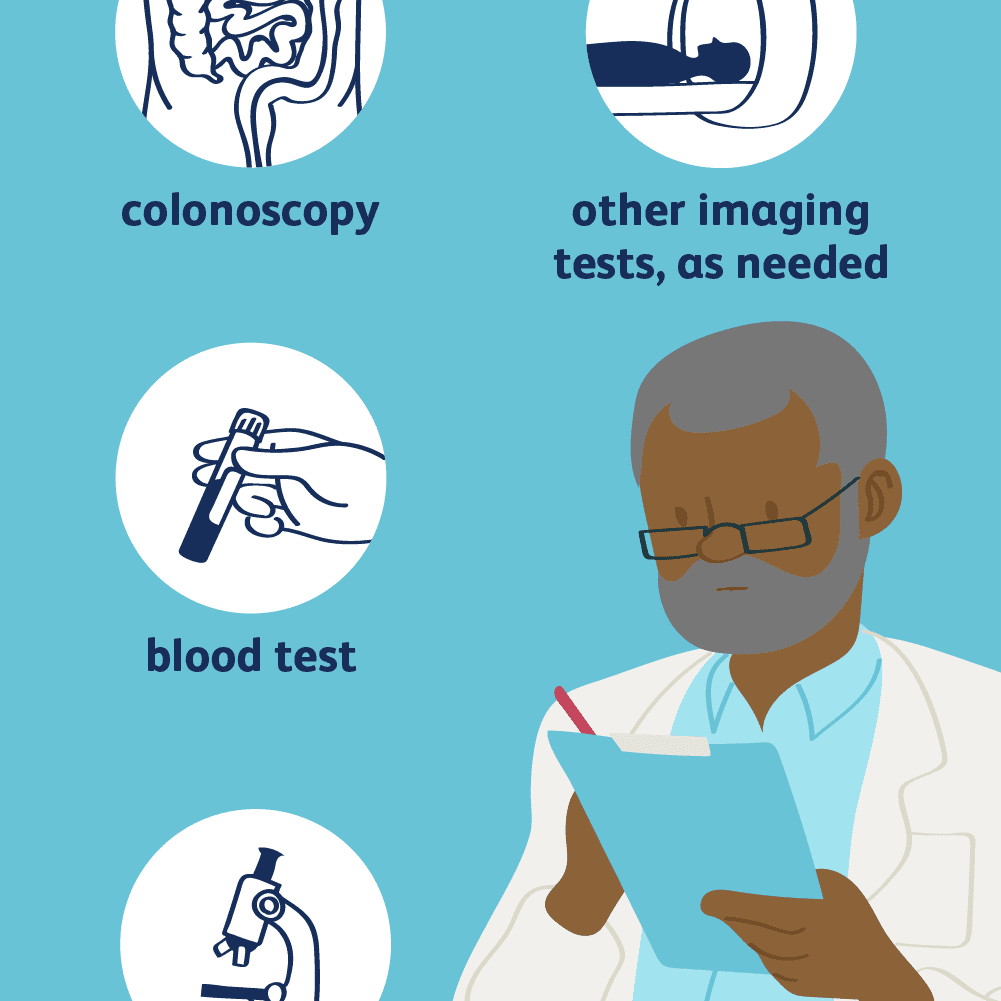
What Laboratory Tests Help Diagnose Ulcerative Colitis
Your doctor would conduct a few blood tests and a stool test to identify if the cause of your symptoms is ulcerative colitis or something else.
Blood tests: A low red blood cell count and low hemoglobin level indicate that you have anemia, which is a symptom of ulcerative colitis.
If you have ulcerative colitis, your blood test may show an increase in white blood cells, a low level of the protein albumin and an elevated C-reactive protein level.
Stool test: Your stool test can let your doctor know if your symptoms are due to infections, such as gastroenteritis.
Read Also: How Can You Tell If You Have An Ulcer
How Do We Diagnose Ulcerative Colitis
The Digestive Health Center at Stanford Health Care delivers expert diagnosis for all forms of inflammatory bowel disease, including ulcerative colitis. Part of what makes Stanford different is our expertise in measuring the degree of intestinal injury for each patient. This helps us understand the severity of your condition and how best to treat it.
Vitamin And Mineral Supplements For Ibd
A person with IBD who eats a healthy, varied diet does not usually need to take vitamin supplements. But if they have a dietary deficiency, they may need tablets or occasional vitamin B12 injections. For example, a person on a low-fibre diet may need extra vitamin C and folic acid because they dont eat enough fruit and vegetables.A person with Crohns disease who experiences steatorrhoea may need calcium and magnesium supplements. Most children with IBD should take supplements to help them grow and develop normally.
Also Check: Ulcerative Colitis And Apple Cider Vinegar
Blood And Stool Tests
A blood test can show if you have anemia, which is a symptom of ulcerative colitis. Anemia happens when your red blood cells decrease and there arenât enough of them to carry adequate oxygen to your tissues. A blood test will also help identify or rule out other infections.
The blood test can also detect an increase in white blood cells, a low level of the protein albumin, and an elevated C-reactive protein level — all indications of inflammation in your body.
When you go to the doctorâs office, they will take a little of your blood and send it off for analysis. The results will come back anywhere from a couple of days to several weeks later.
A stool test may be ordered to rule out infection. Learn more about stool testing.
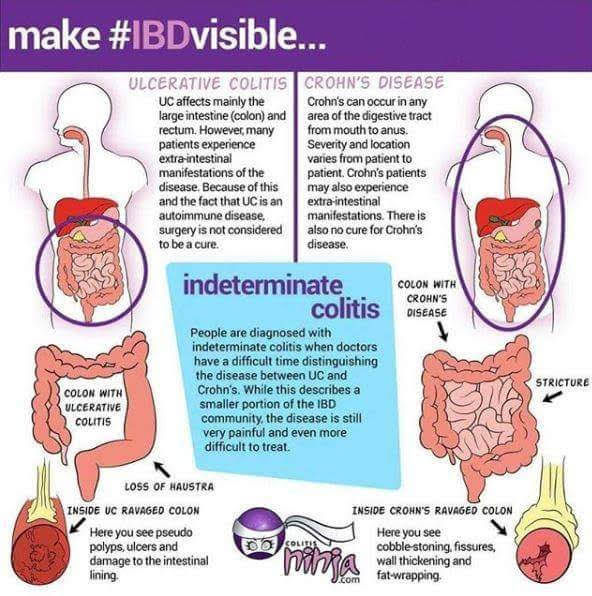
Ulcerative Colitis In Children: Symptoms Diagnosis And Treatment
Inflammatory bowel diseases, which are chronic inflammatory conditions that affect the gastrointestinal tract, include ulcerative colitis and Crohns disease . While Crohns disease can affect any area of the GI tract, ulcerative colitis involves only the colon, also known as the large intestine. Inflammation associated with UC begins in the rectum and can involve the entire colon.
Nearly 25 percent of patients with IBD are diagnosed as children and about one-third of children with IBD have ulcerative colitis. Over the past several decades, IBD has become increasingly common.
You May Like: Can Ulcers Make You Throw Up
History Examination And Diagnosis
3.2.1. Medical history
A full medical history should include detailed questioning about the onset of symptoms, rectal bleeding, stool consistency and frequency, urgency, tenesmus, abdominal pain, incontinence, nocturnal diarrhoea, and extra-intestinal manifestations. Recent travel, possible contact with enteric infectious illnesses, medication , smoking habit, sexual behaviour, family history of inflammatory bowel disease or colorectal cancer, and previous appendectomy should be recorded
The diagnosis of UC is suspected in the context of compatible clinical symptoms. Infectious or drug-induced forms of colitis should be excluded. Family history and EIMs should be discussed.7,159164
3.2.2. Examination
Physical examination should include pulse, blood pressure, temperature, weight and height, and abdominal examination for distension and tenderness. Perianal inspection and digital rectal examination may be performed if appropriate. Physical examination may be unremarkable in patients with mild or moderate disease
Findings on physical examination depend on the extent and severity of disease. Examination of patients with mild or moderate activity is usually unremarkable, apart from blood on rectal examination. Patients with a severe attack may exhibit fever, tachycardia, weight loss, abdominal tenderness, abdominal distension, and reduced bowel sounds.165
3.2.3. Diagnosis
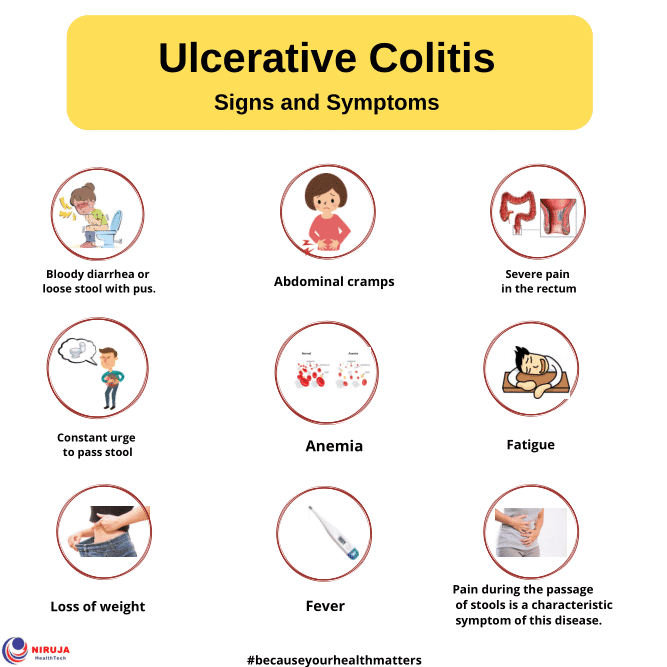
Daisys Story: Symptoms And Medical History
I was 16 years old when I first noticed symptoms that I later found out were due to ulcerative colitis. The first symptom I noticed was severe fatigue, but I put this down to the exams I was taking at the time. I was also noticing abdominal pain more frequent bowel movements, and I was also passing blood. I noticed mucus in my stools and was experiencing frequent bouts of diarrhea.
At first, doctors thought that my symptoms were happening because of hemorrhoids, a stomach bug, parasite, or possibly a small tear. As my exams finished and my stress levels decreased, my symptoms became less noticeable too. However, they still persisted, and I was admitted to the hospital when I began to lose weight after not being able to eat drink.
When the doctors asked my mother and me about my family history, we explained that bowel cancer had affected some family members in the past. The doctors then ordered some blood and stool tests to investigate further.
You May Like: Stomach Ulcer Pain Relief Medicine
Daisys Story: Blood Tests
My symptoms worsened as I went through various tests to work out their cause. One of the first tests was a blood test, which doctors ordered when they believed my symptoms were happening due to a parasite. When the results came back, the doctors told me I had clear signs of inflammation.
I began taking some medications to ease my symptoms, and after these blood test results came back, the doctors referred me for further tests.
How Is It Treated
While there isnt a cure for ulcerative colitis, there are a number of well-established and newer medications that are effective for long-term management. These medications aim to heal the prior inflammation in the colon and keep it under control. Improvement in this inflammation helps to eliminate the symptoms and to normalize childrens weight gain and growth. Of equal importance, these therapies can return kids to their normal activities and optimize their quality of life. Children with well controlled ulcerative colitis can participate in their normal sports, extra-curricular activities, and pursuing all of their life goals.
While some patients may experience a disease flare where the active inflammation of the colon returns, this can usually be treated and patients can reenter remission. In some cases, despite optimization of medication strategies, the colon remains inflamed and children may require hospitalization. In severe cases not responding to medications, we may have discussions with families about surgical removal of the colon to reduce the risks of severe complications of active UC such as ongoing bleeding , perforation of the colon, or cancer risk.
In all children with IBD, adequate nutrition is very important. Many children living with ulcerative colitis are deficient in certain minerals and vitamins related to diarrhea or bleeding, so nutritional balance in their diet and input from an IBD registered dietician is vital.
You May Like: Stage 1 Vs Stage 2 Pressure Ulcer
What Happens During These Ulcerative Colitis Tests
If youve ever found yourself with nothing but a thin hospital gown separating you from a room full of medical professionals ready to look in your colon, you probably know it can feel a little weird. But lets not scare those who havent been there yet. Its really not that bad. In the case of a colonoscopy, youll likely be sedated, and wont be aware of anything anyway.
That said, youll be asked to lay on your side with your knees tucked up by your chest. Your doctor will then insert the scope into your rectum and pump air or carbon dioxide as they move through, which inflates the colon so they can see the lining better. The camera sends images to an external monitor, where the doctor will look for any issues. Other tools can also be inserted to take a biopsy or remove abnormal tissue, such as polyps, according to the Mayo Clinic.
The exam itself can take anywhere from 15 minutes to 30 minutes to an hour for a colonoscopy. If you have a colonoscopy, youll have to stick around for an hour or so as the sedative wears off and have someone drive you home. As you recover, you might feel some abdominal cramping and the urge to pass gas. Our advice? Just let it go, everyone else in recovery is doing it too.
Investigation And Procedures To Establish A Diagnosis
3.3.1. Initial investigations
Initial investigations should include full blood count, electrolytes, liver and renal function, iron studies, vitamin D level, C-reactive protein, and faecal calprotectin . The immunisation status should be assessed . Infectious diarrhoea including C. difficile should be excluded . Endoscopy and histology should be performed
3.3.2. Microbial investigations
Microbial testing is recommended in patients with colitis relapse. This includes testing for C. difficile and Cytomegalovirus infection
Nosocomial C. difficile infection is a growing health problem and has been associated with higher mortality and health resources’ utilisation.172177 ECCO guidelines now recommend screening with every disease flare.11 Moreover, microbial stool tests should be performed in the case of treatment-refractory or severe relapse.178182
3.3.3. Biomarkers
The most widely studied serological markers are perinuclear anti-neutrophil cytoplasmic antibodies and anti-Saccharomyces cerevisiae antibodies . Usually, pANCAs are detected in up to 65% of patients with UC and in less than 10% of patients with Crohns disease.190,191 Given the current limited sensitivity of these markers, their routine use for the diagnosis of UC and for therapeutic decisions is not clinically justified.
You May Like: Antibiotics And Antiseptics For Venous Leg Ulcers
Reaching For My Goals
Seeing others reach for their dreams despite having IBD inspired me to keep dreaming, to keep moving towards the goals and values that matter to me. Those goals and values may have changed some, but I am still as relentlessly pursuing them today as I was prior to my diagnosis.
Today, however, I am strengthened by the knowledge of what I can handle, by the skills Ive gained advocating for myself in doctors offices and on calls with insurance companies, and by the support team I have been lucky enough to assemble around myself.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Recommended Reading: Do Probiotics Help Ulcerative Colitis
Classification According To Disease Extent
Disease extent influences treatment modality, whether oral and/or topical therapy , and determines onset and frequency of surveillance . It is defined by the maximal macroscopic extent at colonoscopy, classified as proctitis, left-sided colitis, and extensive colitis
Extent of inflammation influences the patients management and the choice of delivery system for a given therapy. For example, topical therapy in the form of suppositories or enemas is usually the first-line choice for proctitis and left-sided colitis, respectively, whereas oral therapy is appropriate for extensive colitis. Extent of colitis influences the risk of development of dysplasia or colorectal cancer , and thus the start and the frequency of colonoscopic surveillance.4042
Patients with extensive colitis have the highest risk of developing CRC, whereas those with proctitis alone have a risk similar to the general population. Patients with left-sided colitis carry an intermediate risk however, their risk approaches that of patients with extensive colitis as disease duration increases.4346 Therefore, patients with left-sided and extensive colitis are generally advised to have surveillance colonoscopy, whereas patients with proctitis do not need such surveillance46 .
Focusing On What I Can Control
I realized what I did have control over. My knowledge and my actions were all in my control.
I also realized that I wasnt alone in not knowing the future. While UC obviously adds another layer to this uncertainty, no one truly knows whats to come even with the best-laid plans.
My life is still open with many paths before me. My ulcerative colitis, while a piece of my identity, is not the only piece.
You May Like: What Do Diabetic Ulcers On The Feet Look Like
How Do I Prepare For A Sigmoidoscopy Or Colonoscopy
Truly the worst part of these tests is the prep you have to do before. Both require that you follow a special diet before the procedurethink clear liquidsand take a laxative, to effectively clean out your colon for the scope. You may also be asked to fast for a period of time and use an enema to flush out anything that remains in your colon . Your doctor may also need to adjust your medication schedule, if you take any, according to the Mayo Clinic.
How Long Will Ulcerative Colitis Symptoms Last
Ulcerative colitis is a chronic disease with intermittent flares. A flare, or flare-up, is a period of time in which symptoms of ulcerative colitis are severe. Generally speaking, flares can last for weeks or even months, although ulcerative colitis is experienced differently from person to person, and the duration of symptoms varies greatly for each individual.
People living with ulcerative colitis typically experience periods of both active disease and remission.
The goal of treatment is to achieve remission.
Don’t Miss: Best Over The Counter Ulcer Medication
Watch A Video On Uc Testing And Disease Management
Understanding ulcerative colitis, or UC, doesnt stop at the diagnosis.
Its important to understand testing and disease management, too. We know this can be a lot, but youve got this.
Your doctor will discuss with you the proper tests that can help you find the proper treatment to manage your UC.
Because UC can progress over time, its important to ask your doctor how routine testing after diagnosis may help ensure your treatment is working.
Often together, doctors may test your blood, test biological molecules, called biomarkers, and take images throughout your body.
The results, along with the severity and area of inflammation in your large intestine, may influence how you manage your disease.
Prescription medication can be a common option to treat inflammation in your large intestine. Your doctor may suggest a range of things from changing your diet to surgery.
Ongoing testing is part of disease management, just like treatment.
Knowing more means you can do more. Youre in control of your condition, and now that youre in the know, you can better manage your UC.
When youre living with UC, tests are a routine part of taking care of yourself and managing your condition. Watch this video to understand the basics and help prepare for future visits to your gastroenterologist.
What Are The Extraintestinal Manifestations
Extraintestinal manifestations are common. They may or may not be related to the activity of the colitis.
Box 1: Diagnosing ulcerative colitis
Relevant history
Stool frequency, consistency, blood and mucous
Nocturnal diarrhoea
Extraintestinal manifestations
Travel abroad
Abdominal distension
Investigations
Full blood count liver function tests erythrocyte sedimentation rate measurement of C reactive protein, urea, and electrolytes
Stool culture and Clostridium difficile toxin assessment
Sigmoidoscopy and biopsy
Related to the activity of the colitis:
- Erythema nodosum
- Aphthous ulcers
Usually related to the activity of the colitis:
- Pyoderma gangrenosum
Not related to the activity of the colitis:
- Primary sclerosing cholangitis .
Read Also: Celiac Disease And Ulcerative Colitis
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
What Else Should I Know
It can be a challenge to deal with the symptoms of ulcerative colitis. But many people with the condition can stay well and have few symptoms for long periods of time. Talk to your doctor about ways you can feel better during flares. Because stress can make symptoms worse, its important to get enough sleep and manage stress in positive ways. Yoga, meditation, breathing and relaxation techniques, music, art, dance, writing, or talking to a friend can help.
If you feel sad or anxious about your symptoms, it may also help to talk to a therapist or other mental health professional.
As you get older, you can take on more responsibility for managing your health care. Getting treatment for ulcerative colitis, managing your symptoms, and keeping a positive attitude can help get you back on track.
You also can find more information and support online at:
Don’t Miss: Is Salmon Good For Ulcerative Colitis