What Foods Should I Avoid
Certain foods can exacerbate UC flares, but everyone has different trigger foods. For some, it might be a juicy burger and for others, it could be their morning latte.
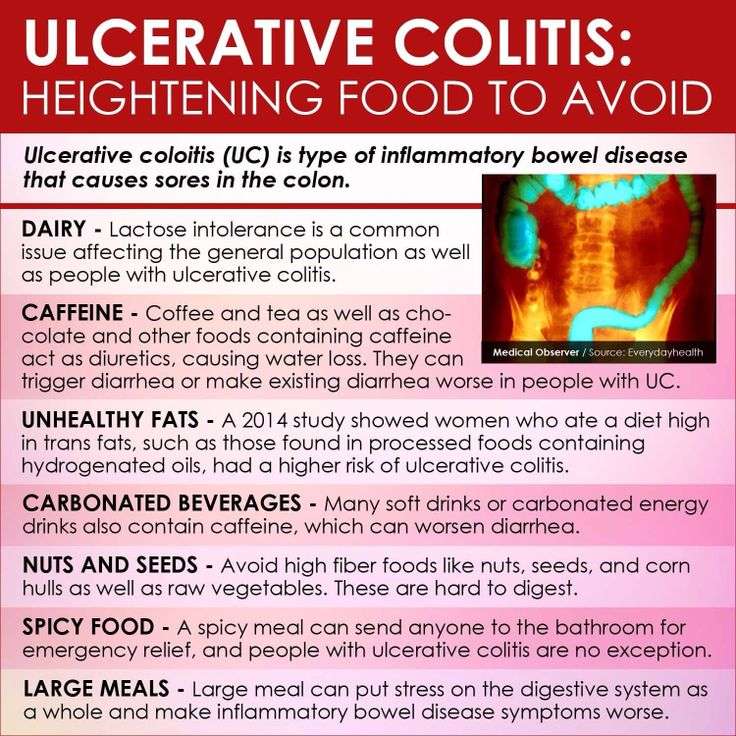
In general, inflammatory foods, like fast food, processed food, alcohol, and sugary drinks contribute to the development of flares, says Dr. Singh. Freuman adds that saturated fat, specifically, can be an issue for certain people. Foods that contain significant amounts of saturated fat include:
- Whole-milk dairy, such as cheese, cream, butter, and full-fat yogurt
Lactose is the sugar present in milk and dairy products, and lactase is the enzyme people need to break down those sugars during digestion. If someone is lactose-intolerant, it means they dont produce enough lactase to break down the sugars, which can cause cramps, bloating, diarrhea, and gas.
To complicate matters, UC is sometimes coupled with lactose intolerance. But lactose intolerant dairy lovers, take heart: Its often possible to still consume dairy with lower lactose content, like cottage cheese and yogurt. Because these products contain live cultures that produce their own lactase, your body doesnt have to do all the work to break down lactose5.
Thats a win-win, since dairy foods provide important nutrients, like calcium and vitamin D, to your diet. In fact, avoiding them completely is not recommended unless 100% necessary.
Dont Miss: Diet Plan For Ulcerative Colitis Flare Up
How A Professional Can Help
Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
Tips For Meal Prepping
Now that you have a sense of what to eat for ulcerative colitis, its time to get in the kitchen. Meal prepping some simple ingredients can make your life easier and prevent a UC flare. Here are some simple strategies:
- Buy pre-chopped fruits and veggies. Having produce in your fridge that dont require any preparation will make you more likely to add them to your plate at mealtime.
- Go frozen. Frozen fruits, veggies, and whole grains are generally as nutritious as fresh produce. Buy frozen fruit for smoothies, frozen veggies for soups and casseroles, and frozen grains to heat up in the microwave as a side dish.
- Pick up ready-made proteins. Stock up on simple options, like a rotisserie chicken or canned beans.
- Make a big batch of soup. Not only is soup soothing, its also an easy way to add a ton of veggies to your diet and is super easy to make in big batches.
- Stock up on healthy fats. Load up your cabinet with nuts, oils, and seeds for snacking, cooking, or adding texture to a recipe.
Don’t Miss: What Diet Is Good For Ulcerative Colitis
Its Not Irritable Bowel Syndrome
IBD and irritable bowel syndrome are confused a lot because their abbreviations are so similar, said Dr. Streett, noting that irritable bowel syndrome is much more common.
In people who have irritable bowel syndrome, they have symptoms that are linked to digestive function, but they do not have objective findings such as inflammation in the GI tract, she explained.
Inflammatory bowel diseases are disorders where there is inappropriate inflammation in different segments of the GI tract, Dr. Streett said. It is diagnosed by doing a colonoscopy to look for and biopsy areas that are inflamed.
Some of the symptoms overlap, but theyre really completely two different diseases and syndromes, said Dr. Gruss. Additionally, if you have IBS, it is not a precursor of IBD.
What To Eat During Flare

Low-fiber foods are easiest to digest and are less irritating to the gut, especially with symptoms like abdominal pain or diarrhea. Choose:
- Grains/starches: White foods, instead of wheat or whole-grain, and those with less than 2 grams of fiber per serving
- Cooked vegetables: Well-cooked vegetables such as green beans, carrots, mashed potatoes without skin, steamed asparagus tips and pureed squash.Use fresh or frozen.
- Canned or soft fruits: Peeled apples, ripe bananas, cantaloupe, honeydew, watermelon, and canned fruit in fruit juice or light syrup
Be sure to eat enough protein — Inflammation causes increased protein needs. Choose:
- Tender, well-cooked meats: Poultry, salmon or other fish, lean beef and pork prepared without added fat
- Deli meats: Low-sodium and low-fat varieties
- Eggs: Well-cooked
- Smooth nut and seed butters: Peanut, almond or sunflower seed
Drink plenty of fluids — Aim for eight cups a day, and consider using oral rehydration beverages as needed. Try to limit caffeinated, sugar drinks and beverages made with sugar substitutes.
Limit added fats and oils — Focus on oils instead of solid fats, and limit intake to less than eight teaspoons per day.
Consume adequate calcium, vitamin D, probiotics, and prebiotics — Sources include:
Also Check: Immune Modifiers For Ulcerative Colitis
Supplements And Other Lifestyle Changes To Try
Besides diet and medicine, there are a few other therapies that could be helpful for people with ulcerative colitis.
Dr. Singh suggests focusing on adequate sleep and reducing stress to prevent flares. One of the most common causes of flare can be stress, so stress reduction is probably the best medicine I talk about when I see patients, he says.
There is also limited research surrounding the use of certain supplements and probiotics as a therapy for IBD, but more evidence is needed before recommendations are made12,13.
Other Foods Are Known Uc Harmers
On the other hand? Things like full-fat dairy, red or processed meats, unhealthy fats, and fried or greasy meals are thought to have the opposite effect, per recent guidance developed by the International Organization for the Study of Inflammatory Bowel Diseases . If trying to get more of the good stuff and less of the bad seems overwhelming, read on. Here, Stein and Rogers share some of their favorite UC-friendly food strategies that can reduce your symptoms and even make it easier to manage your UC long-term.
Don’t Miss: Does Ulcerative Colitis Get Worse With Age
Nutrition And Ulcerative Colitis
There is no special diet for people with Ulcerative Colitis . This means that research has not shown any particular foods to either help or worsen disease activity.
However, ensuring good nutrition is an important part of managing UC.
People with UC are at risk for developing malnutrition and nutrient deficiencies. Poor nutrition makes it more difficult for your body to heal and fight infection. Malnutrition may also cause you to feel tired.
There are several reasons why people with UC may be at risk for poor nutrition, including:
|
So, people with UC should follow a balanced diet and be sure to get enough calories, protein, vitamins, minerals, and fluid. No specific foods must be avoided, but some people may notice that certain foods cause discomfort. If this is true for you, avoid these foods. Nutrition needs vary from person to person, so it is best to meet with a Registered Dietitian who can help you individualize your diet.
Calories and Protein
Vitamins and minerals
Low Fiber/Low Residue: Is it necessary?
What about the special diet I read about?
Special Situations
Lactose intolerance
Strictures, partial obstruction, or narrowed areas of bowel
Additional Resources
Lcerative Colitis Diet Plan
Following an Ulcerative Colitis diet plan is a bit more complicated than something like an IBS plan. The ideal diet for UC patients will vary depending on their symptom severity. For example, during flare-ups, youll want to be gentle on your intestines, eating low-fiber foods. However, when you arent having flare-ups, its healthier and more protective to feed your gut bacteria the fiber it needs.
There is a delicate balance that UC patients need to maintain, and its often a fine line with much back-and-forth from week to week. Your best option is to keep a food journal and log all of your symptoms each day. This way, you can find what works best for you. If you have any questions about how to create a food journal or about other treatments to minimize your UC symptoms, get in touch with the colorectal experts at the Colorectal Clinic of Tampa Bay.
Don’t Miss: What Is A Decubitus Ulcer Why Does It Occur
Vegetables For Ulcerative Colitis: The Bottom Line
Vegetables are worth eating if you have ulcerative colitis, but its important to find options that work with your GI tract and dont trigger symptoms. Soft-textured vegetables that are higher in soluble fiber and lower in insoluble fiber are often more easily tolerated, especially during a flare-up.
If youre having trouble finding vegetables that work for you, talk with a registered dietitian specializing in ulcerative colitis or inflammatory bowel disease. They can help determine how much fiber and what choices are best for each patient, Leben says.
You May Like: How Fast Does Humira Work For Ulcerative Colitis
What Is A Good Diet For Severe Colitis
Yogurt mixed with soft fruits is also a good addition to a diet for colitis sufferers. Try to avoid meat, junk foods and any food that has refined flour when you are suffering from colitis. Ripe bananas are a good addition to the diet of someone suffering from ulcerative colitis .
What foods cause colitis?
Foods with high fiber content like brown rice, quinoa, oats can trigger the symptoms of Colitis especially Ulcerative colitis . It is difficult to digest high fiber foods which increase the bowel movements and abdominal cramps. Caffeine. Coffee, tea and other caffeine-rich drinks are known to flare up the UC.
What is the best diet for UC?
Most experts say that people with UC should simply try to eat a well-balanced diet whenever possible. This should include a variety of foods: Lean meat, fish, and poultry. Low-fat dairy products. Bread, cereal, and whole grains. Fruits and vegetables. Healthy fats such as vegetable oils.
You May Like: Is Keto Good For Ulcerative Colitis
Can Certain Foods Really Cause Inflammation
The link between what we eat and chronic inflammation in the body isnt fully understood. What is known is that there does seem to be some connection.
Lets jump into the science: The liver produces something called C-reactive protein as a response to inflammation in the body. In short, higher levels of CRP mean more inflammation, and certain foods have been shown to increase levels of CRP in the blood.
Now, the specifics of what foods cause this increase is somewhat up for debate, but its possible that things like processed sugar can trigger the release of inflammatory messengerslike CRPa sign that they may potentially be contributing to an inflammatory state.
On the other hand, foods like fruits and vegetables may help fight oxidative stress, which is a trigger for inflammation. Certain diets, like the Mediterranean diet, already include many foods that are considered to be anti-inflammatory such as whole grains, legumes, a rainbow assortment of fruits and vegetables, and fish.
Medication For Ulcerative Colitis
If diet alone doesnt control your symptoms, your doctor may suggest medication. Some medications address inflammation so your bowel can heal. Other medications help you stay in remission when your ulcerative colitis is under control.
Aminosalicylates: These anti-inflammatory drugs treat mild or moderate ulcerative colitis or help extend remission.
Corticosteroids: Steroids provide short-term help for moderate to severe ulcerative colitis.
Immunosuppressants: These treat people with moderate to severe ulcerative colitis and help them stay in remission. Immunosuppressants can also treat severe ulcerative colitis in people who are hospitalized.
Biologics: These drugs are derived from naturally occurring chemicals. They treat people with moderate to severe ulcerative colitis and help them stay in remission.
If you have ulcerative colitis, ask your doctor what treatments will work best for you.
Dont Miss: Can You Develop Ulcerative Colitis Later In Life
You May Like: Diet For People With Ulcers
Ulcerative Colitis Diet: What To Eat To Manage Symptoms
A tailored diet for ulcerative colitis may provide you with some relief
Ulcerative colitis is a type of inflammatory bowel disease in which the immune system is thought to attack the gut lining, failing to recognise it as part of the body. A focused ulcerative colitis diet may therefore help with the management of symptoms. With the guidance of an IBD team or a dietician, those suffering from ulcerative colitis can be put on an elimination diet in order to identify potential trigger foods, or may be encouraged to keep a food diary in order to track links between certain foods and symptoms.
Those who have undergone surgery or are struggling with an ulcerative colitis flare up may be put on a low residue diet or a low fiber diet in order to manage symptoms and lessen the burden of their disease.
However, ulcerative colitis diets are often unique to the individual, so some experimentation under medical supervision may be necessary to find the right eating pattern for you. An ulcerative colitis diet may not work at all either, so it is important to collaborate with your medical team in order to properly manage your condition.
What To Eat During Remission
Increase fiber and reintroduce whole grains — Slowly incorporate foods higher in fiber when gastrointestinal symptoms lessen.
Consume omega-3 fatty acids — Consider eating more fresh or canned fatty fish or taking a fish or flaxseed oil supplement.
Focus on wholesome foods in their natural state — This includes foods with minimal processing and minimum ingredients.
Dairy and lactose products will be better tolerated — If you have a lactose intolerance, avoid dairy or eat low-lactose or lactose-free products.
Added fats will be better tolerated — Continue to focus on using oils, such as olive oil or canola oil, instead of solid fats.
Continue to focus on protein foods — Consume beef, eggs, poultry and other lean meats or plant-based proteins, such as soy products.
Be sure to drink plenty of water — Drink water instead of fruit juices, soft drinks, alcohol and caffeinated beverages such as coffee or tea.
Read Also: Ulcerative Colitis What Vitamins Can I Take
Risk Factors Signs And Symptoms Of Ulcerative Colitis
Ulcerative colitis occurs due to an immune system dysfunction. Normally, the immune system safeguards the body against disease-causing bacteria by sending fighter cells to counter-attack pathogens. However, people develop UC when the immune system mistakes food, beneficial bacteria, and cells lining the colon for intruders. As a result, the white blood cells meant to protect you attack the colonic walls, resulting in inflammation and ulcers.
Ulcerative colitis is an idiopathic inflammatory condition because doctors dont know why people experience on and off UC symptoms. Nonetheless, UC is associated with various risk factors that include:
- Age UC prevalence rate is high among individuals of 15-30 years and those older than 65.
- Ethnicity The risk of developing UC is highest among people of Ashkenazi Jewish descent.
- Family history If you have a close relative with UC, your chances of developing the condition are 30% and above.
Dont Miss: Is Nausea A Symptom Of Ulcer
Inflammatory Bowel Disease Community
The Carlino Family Inflammatory Bowel Disease Center is committed to serving its community. Through a variety of events, including educational programs, community lectures, and support groups, our providers are able to give back to the community and help to spread awareness about IBD.
To learn more about upcoming events please e-mail:
You May Like: Low Dose Naltrexone Ulcerative Colitis
Recommended Reading: How To Treat A Bleeding Ulcer
What Causes Ulcerative Colitis
The cause of ulcerative colitis is unknown but it is believed to be caused by a combination of several factors including an overactive immune system, genetics, and the environment.
- Overactive immune system: It is believed that in ulcerative colitis, the immune system is triggered to mistakenly attack the inner lining of the large intestine, causing inflammation and symptoms of ulcerative colitis.
- Genetics: Ulcerative colitis can run in families. The genetic link is not entirely clear but studies show that up to 20% of people with ulcerative colitis have a close family member with the disease.
- Environment: Certain environmental factors including taking certain medications , and eating a high-fat diet may slightly increase the risk of developing ulcerative colitis.
Physical or emotional stress and certain foods do not cause ulcerative colitis, however, they may trigger symptoms in a person who has ulcerative colitis.
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Read Also: Total Contact Casting For Diabetic Foot Ulcers