Clinical Evidence For Total Contact Casting
The use of TCC as the most effective off-loading method is strongly supported by clinical evidence. Randomized clinical trials provide strong evidence of reduced healing time and greater numbers of healed DFUs for TCC when compared to other methods.
Lavery et al. showed that TCC had a wound closure rate of 88.9%, compared to 50% for healing sandal and 40% for shear-reducing walking boot. They also showed that median time to healing for TCC was 5.4 weeks, compared to 8.9 weeks for a healing sandal and 6.7 weeks for sheer reducing walking boot.
Armstrong et al. determined that TCC had a healing rate of 88.9%, compared to 65% for a removable cast walker and 58.3% for a half-shoe, and time to healing was least for TCC at 4.8 weeks, compared to 7.2 weeks for the removable cast walker and 8.7 weeks for the half-shoe. This data was reiterated by Lavery almost 14 years later in a newer study .
How Long Must The Tcc Stay On
TCCs are typically changed every week, or alternating weeks, depending on several factors, such as the amount of edema, the rate of healing, practitioner preference and patient tolerance. Use of TCC is continued until healing has occurred and the foot is ready for footwear or an orthotic.
Did you enjoy this article? If so, you can find many more like it here. If you are interested in learning more about how Wound Educators can assist you in achieving wound care certification, visit our site.
Foot Ulcers and the Total Contact Cast. American Orthopaedic Foot and Ankle Society.
Total Contact Casting. Wound Care Centers.org.
Myers, B. . Appendix D: Total contact casting procedure and patient instructions. Wound Management: Principles and Practice . Pearson Prentice Hall. Upper Saddle River, New Jersey. pg. 464-465.
Experimental Protocol And Data Analysis
The participants walked at a comfortable self-selected walking speed along a 9m walkway. Trials, whereby the participants walked at a velocity outside a 10 % individual tolerance, were excluded from the study. Both pedar® and pliance® collected data simultaneously at a sampling rate of 50Hz synchronised to the temporal event of heel strike. Each trial started with the participant standing with two feet together. Each participant was instructed to commence walking after the various data collection systems had commenced recording. In this way, the heel strike of the first step of each trial could be used for synchronisation purposes. This synchronisation was completed manually by combining video, plantar and TCC wall data. Each participant walked a minimum of two successful trials.
Descriptive statistics and normality of data distribution were computed in SPSS v22.0 . The magnitude of TCC wall load as a proportion of plantar load was calculated. Following removal of the cast walls, the difference in plantar loading between the TCC and the shoe-cast for the whole foot and three clinically relevant regions of the foot, including rearfoot, midfoot and forefoot , were calculated using the Novel software . Paired sample t-tests were undertaken to assess significance between TCC and shoe-cast conditions. The alpha value was set at 0.05.
Recommended Reading: How To Treat An Eye Ulcer
Length Of Time For Treatment
Patients will need to come in weekly for a total contact cast change as well as if the other options are being used, along with weekly debridement of callous and soft tissue.
In general, once the wound bed is covered with epithelialized cells, the patient needs to continue to come in for treatment for two more weeks after this point, Wollheim said.
The overall target for healing a wound is to see greater than a 50% reduction in its size within one month, according to Wollheim. This indicates the wound will likely heal within three months.
If a wound has reduced its size by less than 50% in one month, there is only a 10% chance it will heal in three months, he said.
Who Needs A Total Contact Cast
Total contact casts are commonly used by people who have diabetes with foot ulcers that are not healing. Diabetes can cause problems with the feet. A complication called neuropathy can cause a loss of feeling in the feet. This can make it hard to tell if you have a blister or sore on your foot. Small sores can turn into big sores fast. If small sores arent taken care of, they can get worse and turn into ulcers.
Read Also: Things To Eat When You Have An Ulcer
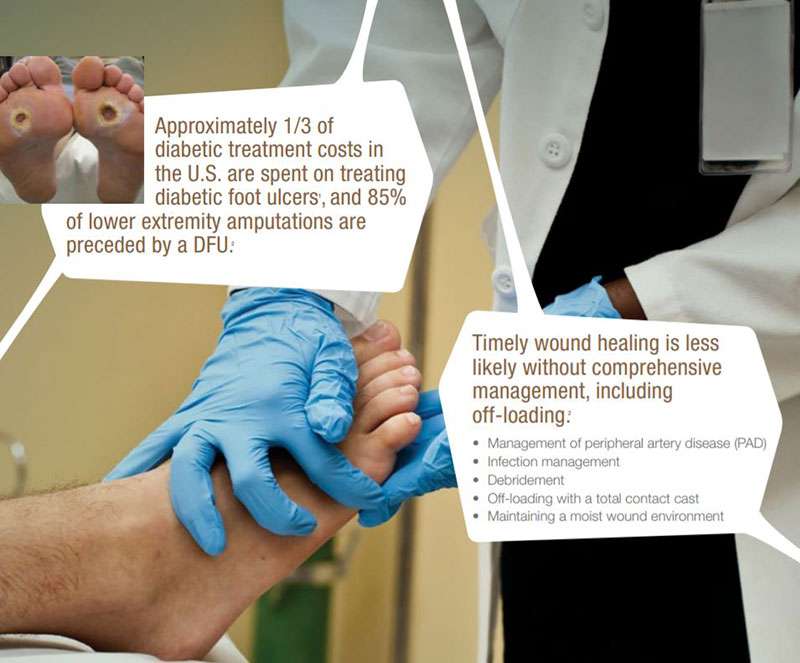
Diabetic Foot Ulcer Overview
Neuropathic DFUs are chronic wounds that result from a combination of factors. Some of the main factors that result in DFUs include :
These factors rarely cause problems in healthy people but the accompanying neuropathy means that the “pain feedback loop” that induces humans to limp or keep their weight off an injury no longer functions properly in diabetic patients. The result is that pressure and abrasion injuries, such as bruising and blisters caused by poor footwear, are not noticed and often ignored, and the continual use of the limb disrupts and damages the healing process.
The healing of DFUs requires many weeks, and patients need to be effectively off loaded during this time. A recent publication on the treatment of DFUs identified that the largest potential improvement in DFU care would come about through adoption of effective off-loading techniques.
Looking At The Gold Standard Of Treatment
Offloading the neuropathic foot is the cornerstone of diabetic wound management, and the total contact cast has been recognized as the gold standard for treatment for decades.2-7 The success of the TCC has been attributed to its ability to unload the plantar foot and maintain immobilization by the non-removable cast. Reducing plantar pressures allows for unimpeded wound healing and achieves complete closure in most wounds by 12 weeks. A high recurrence rate plagues these wounds, and failure to transition patients to their final footwear often has them back in the clinic in a short period of time. The use of an appropriate shoe-foot interface to achieve a redistribution of forces from areas prone to ulceration to the remainder of the foot has not been adequately studied, except for the total contact molded innersole, and countless devices, techniques, and modifications have been tried with varying success.8-14 These have included total contact insoles, pixelated offloading insoles, segmented diabetic healing shoes and insoles, and innovative sole designs for depth footwear for everyday use. TCC “kit” systems have been developed by several companies to streamline the application of the modality and increase its use by practitioners who have been slow to embrace the TCC despite convincing research to validate its use.
You May Like: Foods To Eat If You Have A Stomach Ulcer
Proper Care Following The Removal Of The Restrictive Offloading Device
About the AuthorDr. James McGuire is the director of the Leonard S. Abrams Center for Advanced Wound Healing and an associate professor of the Department of Podiatric Medicine and Orthopedics at the Temple University School of Podiatric Medicine in Philadelphia. Dr. McGuire has over 30 years of experience in wound management and lectures both nationally and internationally in the areas of wound healing, diabetic foot management, off-loading, and biomechanics of the at-risk foot.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, Kestrel Health Information, Inc., its affiliates, or subsidiary companies.
What Do I Need To Know About My Cast
Depending on the type of cast you have, the cast will take either 30 minutes or 24 hours to dry after it is first fitted. Your doctor will tell you what kind of cast you have. It is important that you dont put any weight on the cast while its drying.
You should do as little walking as possible after the cast dries, for these reasons:
- The ulcer will heal faster if you put less pressure on it.
- Your leg with the cast is longer than your other leg. This can cause pain in your hip or back if you walk too much.
- Youre less stable when youre wearing a cast. Your chances of falling and hurting yourself are increased. The less you walk, the less likely you are to fall. Be very careful on slippery or uneven ground. Use a cane for added stability, even if you usually dont use a cane. If you were already unsteady before wearing the cast, it is a good idea to use a walker.
Read Also: Remicade Infusion For Ulcerative Colitis
Is There Anything Else I Should Know
Here are a few other tips that may help you.
- You may have some itching under the cast. Dont slide anything down the cast to scratch the itch. You could easily damage the skin underneath.
- When youre sitting down, put your leg up on a chair or pillow whenever possible.
- While youre sleeping, you might kick or rub your other leg with the cast. This could cause skin damage on your other leg. It is a good idea to put a thick, soft, knee-high sock over your other leg before you go to bed. Or put a pillow between your legs.
If you would like more information on how diabetes affects your feet, ask your doctor.
The Total Contact Casting Procedure
Total contact casting is done by molding a cast over the entire surface of the foot and part of the leg. A soft layer of foam is placed on the ulcer, and the whole foot is wrapped in bandages prior to the application of the cast. The cast, which follows the contours of the foot, is designed to distribute the weight evenly over the entire weight-bearing surface of the foot. This results in offloading of pressure from the ulcer and the bony prominences of the foot.
Healing of ulcers using total contact casts takes approximately six to eight weeks, during which the cast is replaced on a weekly basis. The cast is removed when complete healing is achieved, after which it is recommended that the diabetic patient wear specially designed shoes.
Also Check: How Dangerous Is Ulcerative Colitis
How Is The Tcc Applied
The following depicts the usual steps when applying a total contact cast:
- Have the patient lie on his/her stomach with the affected leg pointing straight up
- Ensure that the ankle is bent in a neutral position
- Apply a thin dressing over the ulcer
- Apply a thin layer of stockinette
- Apply protective cast padding between the toes
- Apply cast padding in a thin layer up the limb
- Apply secondary foam padding over vulnerable areas
- Apply the plaster undercoat smoothly to the foot and leg, covering the toes and going up the leg
- The sole of the cast is applied so that it very closely molds the contours of the sole of the foot any valleys in the sole are filled in with plaster of Paris so that the sole is flat
- The cast may be reinforced with fiberglass and a rocker bottom sole or specially curved sole is applied for patients that are to be permitted to weight bear
What Is Total Contact Casting

Total contact casting is a special casting technique designed to heal diabetic foot ulcers by relieving pressure on the prominent areas of the foot that are prone to skin breakdown and ulceration. The cast is applied so that the patient can remain ambulatory for the duration of the casting and is composed of fiberglass or plaster. Its purpose is to protect the ulcer, allowing for wound healing.
Also Check: What Does An Ulcerative Colitis Flare Up Feel Like
What Causes A Foot Ulcer
Patients with diabetes are prone tomajor foot problems. This is because the foot expresses many of the underlying effects of diabetes, including neuropathy, vascular disease, and diminished response to infection.
As a result of the neuropathy, the foot can develop an ulcer. This happens for two reasons. The first is that the neuropathy causes paralysis of small muscles in the foot, which results in clawing of the toes. Clawing of the toes causes prominence of the metatarsal heads on the bottom of the foot as well as the knuckles on the dorsum of the foot.
Neuropathy also causes diminished sensation. As the prominent metatarsal heads on the plantar of the foot are subjected to increased pressure, the skin will begin to enlarge and become callused. The callused skin can be subjected to shear forces that cause a separation between the layers of the skin. The layers can fill with fluid, which can then become contaminated and infected. The pressure also can cause primary breakdown of the skin in these areas, causing a foot ulcer. Once the initial breakdown and contamination occurs, the foot may develop more significant problems because of infection.
Advantages Over Other Treatments
Medical or surgical treatment may not be adequate for diabetic foot ulcers. Even if the best care is given, healing may be delayed if the ulcer is subjected to constant pressure while walking. Total contact casting provides optimal wound healing conditions by ensuring that the ulcer is not further traumatized and also prevents the development of new ulcers in the bony prominences of the foot.
Precautions
A patient scheduled to receive a total contact cast should be properly informed of the procedure, since this treatment will impose limitations on freedom of movement. Walking should be done with the aid of a cane or crutch in order to avoid exerting any pressure on the affected foot and to prevent any fall-related injuries. Any development of hip or back pain should be reported to a doctor, as this may signal musculoskeletal strain due to the cast. The cast should remain dry, so the patient is advised to take sponge baths instead of showers.
RELATED ARTICLES
Don’t Miss: What’s The Signs Of An Ulcer
History Of Clinical Use
The use of TCC for foot ulcers resulting from leprosy was reported by Joseph Khan in India in the 1930s. Research conducted by Paul W. Brand, MD, in the 1940s and 50s, also in India, demonstrated that the wounds in the feet were caused by nerve damage rather than infection, as previously thought. In his use of TCC to eliminate weight and pressure on the ulcers, he observed the healing of ulcers that had been present for a long time. These seminal observations resulted in the development of treatments to manage neuropathic foot ulcers, which are useful for patients with diabetes.
In 1965, TCC was introduced to the United States by Dr. Brand, then at the National Hansen’s Disease Center in Carville, Louisiana. The goal of TCC was to distribute weight over the entire foot and lower leg. Over time, the staff at Carver Hospital refined the method to reduce the development of other wounds that occur in part because of the initial problem with the foot .
In 2003, the first TCC casting system that contained all the materials in one package was developed. This innovation helped standardize the application of TCC. Other advancements have been made to make casting easier to learn, easier to apply and less time-consuming.
What Is A Total Contact Cast
The total contact cast is a specific casting technique that is used to heal diabetic foot ulcers and to protect the foot during the early vulnerable phases of Charcot fracture dislocations. The cast is used to heal diabetic foot ulcers by distributing weight along the entire plantar aspect of the foot. It is applied in such a way to intimately contact the exact contour of the foot hence the name, “total contact cast.”
The cast relieves the pressure on the prominent areas of the foot, permitting the ulcers to heal. The cast should applied in such a way that the patient can remain mobile during the treatment of the ulcer. The cast is molded to the contours of the foot from the back of the heel through the arch region, in the region of the metatarsals, around the metatarsals, and even to the toes. The pressure, which has been concentrated on the bony prominence, is now distributed over the entire sole of the foot.
For the Charcot foot, the total contact cast is used in two ways. In the initial treatment of the Charcot foot when the breakdown is occurring and the foot is quite swollen and reactive, the cast is applied to control the movement of the foot and support its contours. In this instance the patient is often asked not to bear weight on the foot. In the second instance when the foot has already become deformed and ulceration has occurred, the principle using the cast is the same as described for the foot that has become deformed due to paralysis of the small muscles.
You May Like: Good Things To Eat With Ulcerative Colitis
Treat Diabetic Ulcers With Total Contact Casting
Foot ulcers are a common complication of diabetes and require professional management and off-loading. Chiropodists are professionals trained in diabetic foot care who understand the complexities of ulcers.
Lets review several methods used to off-load diabetic ulcers:
- Specialized removable footwear
- Removable Air Cast
- Total Contact Casting
Often, methods that allow a patient to remove their off-loading device are ineffective at resolving wounds. This ineffectiveness is due to patients not wearing their devices at all times when on their feet. Total Contact Casting eliminates this challenge. It is a specially designed, off-loading cast that ensures treatment compliance.
Important Total Contact Cast Facts
The total contact cast is the gold standard of treatment and the standard of care for diabetic foot ulcers that are neuropathic, Wollheim said.
However, there are some alternatives to the total contact cast for off-loading .
One is the use of a product called TCCEZ, which some clinicians feel more comfortable using because it is easier to apply.
The healing rates of the TCC-EZ is about the same as with the use of a traditional total contact cast, Wollheim said.
Another option is the use of a removable cast walker that is a clamshell type of structure with Velcro.
With a removable cast walker, we typically see a 65% healing rate not as good as a total contact cast, Wollheim said. However, some clinicians are more comfortable using it.
A clinician can create an instant total contact cast, according to Wollheim, by using a removable cast walker and securing it with duct tape or rolled plaster.
This can force compliance as the patient will not be able to take it off, he said. We call this an instant total contact cast and the healing rates are the same as with a total contact cast 75% to 100%.
The topical antimicrobial products used in wound care and the use of systemic antibiotics will vary, Wollheim said.
Don’t Miss: Diet Plan For Ulcerative Colitis Flare Up