Which Nutrients Are Important In Crohn’s And Colitis
Vitamins and minerals
Your body needs vitamins and minerals to work and stay healthy. Your Crohns or Colitis may stop you absorbing enough vitamins and minerals from your food. Vitamins and minerals that you may not absorb properly include iron, vitamin B12, vitamin D and calcium.Eating a healthy, balanced diet may help improve the level of vitamins and minerals in your body. If blood tests show you have low levels of vitamins and minerals, your doctor or specialist nurse may recommend you take supplements to restore your vitamin and mineral levels.Speak to your doctor, specialist nurse or dietitian if you think you may have low levels of any of these nutrients.
Iron
Having low levels of iron is common in people with Crohns or Colitis. Possible causes include a lack of iron in the diet, blood loss and problems absorbing iron from food. Lack of iron can lead to anaemia, where there are fewer red blood cells to carry oxygen around the body.Common symptoms of anaemia include:
Vitamin B12
Vitamin D
Calcium
Fibre
Its important to speak to a dietitian before cutting down on fibre so you dont miss out on the health benefits. For example, they may suggest that some people cut down on fibre for a short time during a flare-up, before slowly adding it back in to the diet.Fibre-rich foods include:
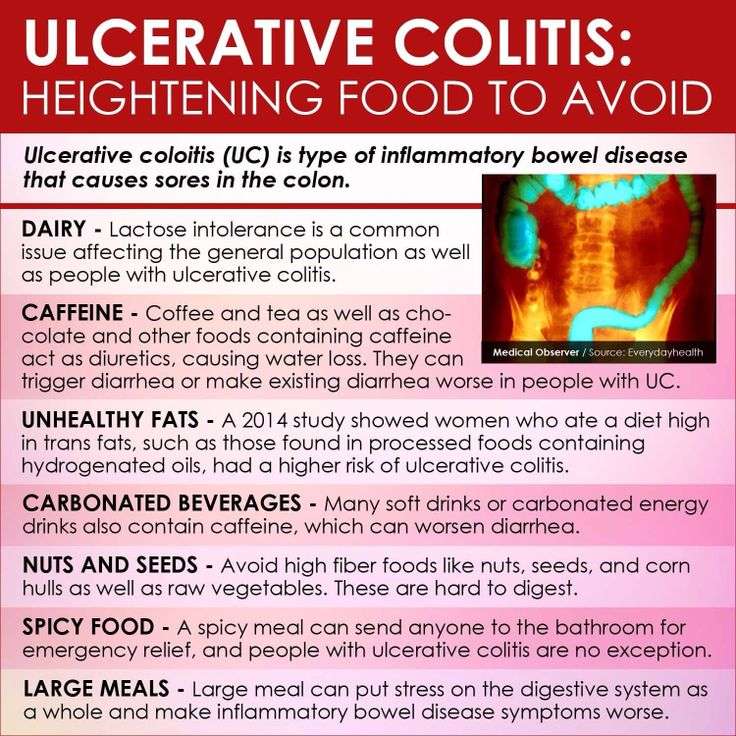
Foods To Avoid With Ulcerative Colitis
- Added sugars and hyper-processed foods
Our North American love affair with low fibre, high sugar and high fat hyper-processed food is associated with our risk of ulcerative colitis. It is this type of eating that is thought to drive gut dysbiosis or the overgrowth of more pro-inflammatory gut bacteria that can harm gut barrier integrity leading to leaky gut and inflammation. In laboratory studies, this type of diet can decrease the number or acetate and butyrate producing bacteria and increase the risk of colitis.
Another issue with hyper-processed foods is that they contain emulsifiers like xanthan gum and carrageenan which may alter gut barrier integrity. While their true impact on gut health is still hotly debated, in one double-blinded trial, people with ulcerative colitis on a carrageenan free diet had lower relapse rates than those given two capsules of carrageenan. For me, this would not be the first place I look when adjusting someones diet instead, it would be a refinement only after taking more global steps towards a more whole foods, plant-based approach.
- Meat, particularly red meat
If you arent a huge fan of red meat, ditch it entirely. If you truly love red meat, try to limit yourself to one 3-4 ounce portion every week or two, no more.
Dairy could be impacting symptoms for a few reasons:
- Omega 6-rich cooking oils like soy, corn and safflower oils
What To Do During A Flare
Medications are used to manage flares and induce remission as quickly as possible.
Doctors may prescribe a corticosteroid , antibiotic, 5-aminosalicylate, immunomodulator or biologic.
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day .
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 2530 grams.
- Drink plenty of fluids to avoid dehydration.
You May Like: What Vegetables Are Good For Ulcerative Colitis
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohns Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohns disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Dont Miss: Stomach Ulcer Over The Counter
Ulcerative Colitis Diet: Food Preparation And Meal Planning
While the idea of an elimination diet or restricting your intake of fiber, fat or other trigger foods may seem daunting, meal planning and preparing your food ahead of time can take some of the stress out of eating in a flare up. If your appetite is impacted as well, you can batch cook and eat what you want of a larger pre-prepared meal when you feel like eating, rather than preparing yourself a whole new meal from scratch.
The Crohns and Colitis Foundation indicates that rates of depression and anxiety are higher in those with IBD, so anything that can reduce stress for those with ulcerative colitis might be helpful for managing mental health. As such, pre-planned meals based around particular dietary needs can make the day-to-day experience of ulcerative colitis slightly less stressful, and may make the experience of a flare up more bearable.
This article is for informational purposes only and is not meant to offer medical advice.
Read Also: How To Cure Ulcer Naturally At Home In Tamil
Would You Like More Information On How To Start A Low Fodmap Diet For Ulcerative Colitis
Tap the blue button below to download our Eat This, Not That list as well as additional resources for IBS and colitis
SEND ME THE LIST
About Kimberly Yawitz
Kim Yawitz is a registered dietitian and nutritionist in St. Louis, Missouri.
She currently works with sports nutrition and weight management clients for a private practice. Prior to that Kim worked as an inpatient clinical dietitian, developing nutrition care plans for patients with health concerns ranging from autoimmune disease to critical illness.
Learn more about her on the About page.
Joe Leech, Dietitian
Recent Posts
Bottom Line: Is The Carnivore Diet Good For Ulcerative Colitis
There is no cure for UC so when we read social media posts or headlines that try to say the opposite, we must be wary. It has been well established that fiber from carbohydrates and plant foods are health promoting, particularly for Ulcerative Colitis and the IBD community. For more on what to eat for IBD, we have plenty of free resources and blog posts.
If you are confused about what to eat and are ready for a higher level of support from a specialist, schedule a free discovery call to explore ways we can help you. We have many different levels and ways to support your IBD journey!
Don’t Miss: How To Get Rid Of Ulcers In My Mouth
What You Should Know:
- Inflammatory Bowel Disease is a term for two specific and separate diseases: Crohns Disease and Ulcerative Colitis. Crohns disease is a disease of unknown cause that can involve any portion of the digestive tract. Ulcerative colitis is an inflammatory disease of the colon or large intestine, which is often accompanied by bloody diarrhea.
- Sometimes surgery and/or medications are needed to treat these diseases.
- Inflammation in the colon can cause the colon to empty frequently, causing diarrhea.
- Stress or certain foods can exacerbate symptoms.
- There is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet.
- Many people with IBD are at increased risk for nutrient deficiencies and may require a vitamin/mineral supplement.
Replace Red Meat With Salmon
Next time you’re thinking steak, make it salmon, or another meaty fish rich in omega-3 fatty acids like tuna, mackerel, or herring, recommends Rogers. Consumption of red and processed meats are tied to a worsening of UC symptoms, per the IOIBD’s most recent guidelines, while omega-3 fatty acids from seafood seem to help support lower levels of inflammation. Try a roasted salmon filet with a baked potato and sauteed spinach grilled, flaked tuna as a taco filling or use either fish to make burgers in lieu of the usual hamburger.
Don’t Miss: Spices To Avoid With Ulcerative Colitis
Track The Good And The Bad
There’s no single diet that will help everyone with UC. The condition can also change over time, so your plan will need to be flexible, too. The key is to find what works for you.
To stay organized, keep a food diary. Use your smartphone or a small notebook to record what you eat and drink and how they make you feel, both good and bad. It takes a bit of time and patience, but it will help you track your condition and fine-tune your diet plan.
When you prepare your meals, don’t forget that a well-balanced diet gives you enough protein, whole grains, and fresh fruits and vegetables.
You might not be able to eat everything in the grocery store or on the menus at the restaurants you like. But try to focus on the ones that you can enjoy without triggering your symptoms. Some simple tweaks in your meal prep can make it easier to eat some foods, like steaming veggies or switching to low-fat dairy.
Some people follow a low-residue diet or low-fiber diet every so often, getting about 10-15 grams of fiber a day. That can help you go to the bathroom less often.
Watch out for items that can be troublemakers if you have UC, including:
Faq: Dietary Management Of Ibd
Information regarding dietary treatments for IBD is often confusing. Many people receive information telling them to avoid entire food groups or specific foods. However, there is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet. This is important for maintaining the function of your digestive tract and your overall health.
You May Like: Is Xeljanz Used For Ulcerative Colitis
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, the symptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
Reintroducing Your Usual Diet

Your IBD team and dietitian will give you information about returning to your usual diet after youve finished enteral nutrition. They may suggest reintroducing foods slowly so you can see if any foods affect your symptoms and to help you feel more confident about eating again. There are three ways of doing this:
- the elimination diet – after excluding all foods, they are reintroduced one by one every few days, to see if they cause problems
- the Royal Free method – this is similar to the elimination diet but foods are reintroduced more quickly, over a period of days rather than weeks
- the LOFFLEX diet – this excludes foods high in fat and fibre.
There isnt much evidence to show how well these diets work, or whether one works better than another. Your dietitian will explain the benefits and risks of all your options.
Ive found that you have to be very careful on the internet as there are many websites claiming to cure IBD through untested diets and supplements – which are not properly regulated and could be harmful and also expensive.
Zaineb
This is an extreme form of low carbohydrate diet that limits:
Read Also: Over The Counter For Ulcer Pain
Can Surgery Affect Nutritional Status
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
The Best Foods To Eat And Avoid For Inflammatory Bowel Disease
Inflammatory bowel disease is a treatable, yet chronic and lifelong condition. IBD is a broad term that refers to the inflammation of the gastrointestinal tract and includes specific conditions such as ulcerative colitis and Crohns disease.
No plan has been proven to prevent or control IBD. But managing your diet can help manage your disease during flares and periods of remission. Be sure to talk to your physician or a registered dietitian about your nutrition needs and managing IBD.
Here are diet recommendations for managing IBD flares and remissions from UH Outpatient Nutrition Services.
Don’t Miss: List Of Foods To Eat When You Have An Ulcer
Eating When You Are In Remission
While theres no cure for UC, you may experience periods of remission. During this time, youll be symptom-free and your UC wont interfere with your daily life.
Theres no definitive way to avoid flare-ups forever, but you can prolong your remission periods by maintaining a diverse and nutrient-rich diet that does not include trigger foods.
To stay symptom-free, it may be helpful to follow one of the diets that other individuals with UC find successful, as well as introduce new foods slowly and stay hydrated.
However, its important to consult with your doctor or dietician before making any changes to your diet.
Some foods that may help keep you feeling good and hydrated during remission
One Pan Chicken And Butternut Squash
A one pan chicken and butternut squash recipe contain two, simple main ingredients. White poultry is a source of lean protein. Meanwhile, butternut squash is a type of winter squash. Squash contains potassium, an important nutrient for people with UC.
People may also substitute the chicken for a meatless option, such as tofu or tempeh.
Read on for good meat alternatives.
Read Also: Tnf Alpha Inhibitors For Ulcerative Colitis
Is There Any Evidence For The Carnivore Diet
Many Carnivore Diet advocates will claim the diet helps with weight loss, inflammation, and mental clarity however there is little to no scientific evidence to support these claims.
One such study looked at self-reported social media data on nutritional practices and health status of a large group of Carnivore dieters. Participants reported a high level of satisfaction due to the high protein intake and improvements in overall health with little negative effects .
Even so, its important to realize that self-reported data with little to no controls makes for a weak study. These participants were simply self-identifying and answering a few questions. The only other Carnivore Diet specific study I could find was an opinion piece on whether the diet could provide all essential nutrients .
In fact, the overwhelming majority of the literature suggests the exact opposite of the Carnivore Diet is best- a diet rich in plant sources and low in animal proteins.
It has been well established that a diet high in animal proteins increases risk of intestinal diseases by producing toxic metabolites like amines and hydrogen sulfide in the colon, thereby changing the integrity of the gut microbiome . Additionally, a diet high in red and processed meat has long been linked to colorectal cancer .
Pros Of The Carnivore Diet In Ibd
So, are there any pros to the Carnivore Diet in IBD?
Potential pros include:
- Increased satiety due to protein intake
- Abundance of iron-rich foods
- Reduction in IBD symptoms initially?
While yes, the Carnivore Diet does provide ample amounts of protein and iron it does so at the detriment of health promoting compounds like fiber and polyphenols found in carbohydrates and plants.
It may reduce or eliminate processed foods and sugars, however that fact does not outweigh the elimination of fiber and pigmented plant sources.
In IBD, the patient already has an altered microbiome. The goal with nutrition therapy for IBD is to restore some sort of normal for that person. It would not be in the best interest of the patient to continue promoting high animal proteins and creating toxic by-products in the process, further degrading the gut lining.
One could argue that the Carnivore Diet reduces symptoms of IBD initially due to the lack of fiber. There could be less irritation or discomfort related to the fiber intake, however symptom irritation is NOT the same thing as inflammation. Read more about that here.
Don’t Miss: Symptoms Of A Bleeding Ulcer In Your Stomach
Energy And General Health
If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.