Can Collagen Help With Treatment For Colitis
Weve all experienced that terrible scenario of being out and about and suddenly needing the loo, right? Well, what if that were to happen to you several times during the day? And what if the urge was so desperate, you had to find one immediately? Waiting patiently for someone else to finish just wasnt negotiable you need it now.
For Barney, its a permanent way of life, although these days its a little easier to manage. Now on the cusp of turning 40, Barney realises the signs were there since his childhood days. It was not uncommon for stomach cramps to be so severe that he would find himself on all fours or doubled over in pain. A farm boy who was forever outside mucking about, the family was never overly concerned.
Stop biting your dirty nails, his mum would reprimand him.
Only, it wasnt his nails at all. And the pain was eventually going to snowball into something so much worse.
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
To Eat: Easier To Digest Fruits
silkegb / Getty Images
Fruits with a lot of seeds might be difficult during a flare-up and should be avoided in most cases, which includes a lot of berries. Melons, however, are going tao be a good choice for a fruit that is easy to digest. Some of the fruits that are going to be more friendly for people in an IBD flare-up include bananas, watermelon, cantaloupe, papayas, and honeydew. Eat these fruits when they’re quite ripe and with all the seeds removed.
Also Check: What Is The Best Pain Medication For Ulcerative Colitis
What Foods Should I Eat During An Ulcerative Colitis Flare
When you are experiencing an ulcerative colitis flare-up, experts suggest you stick to foods that are less likely to aggravate your gut. Some of these include:
- White rice, bread, and pasta
- Crackers and cereals made with refined white flour
- Cooked veggies without the skin
- Tender, soft meats and fish
- Olive and coconut oil
- Lots and lots of fluids, since an ulcerative colitis flare-up can lead to diarrhea and thus dehydration
These foods have been found to be easily digestible in some ulcerative colitis patients, but be cautious when adding them to your diet since they can be triggers in other patients:
- Plain instant oatmeal
When you are experiencing an ulcerative colitis flare-up, experts suggest you stick to foods that are less likely to aggravate your gut.
Also Check: What Is The Medication For Ulcerative Colitis
Choose Fruit Without Seeds
Berries such as strawberries, raspberries, and blackberries are high in antioxidants, which may help ease inflammation. But theyre also possible UC triggers, because they contain seeds that are tiny and difficult to strain out, Craggs-Dino says.
Blueberries, which also contain antioxidants, dont have this type of seed, but they do have skin that can be difficult to break down during more severe flares. To work them into your diet, try tossing them in a smoothie, says Cavagnaro.
Smoothies break down that insoluble fiber that our belly struggles with, she says. Still, she cautions, If youre in a flare, avoid them. Instead, swap berries for applesauce, canned peaches or pears, and bananas.
Read Also: How Long Does An Ulcerative Colitis Flare Up Last
Probiotics For Ulcerative Colitis
The balance of “good and bad bacteria within the gut likely plays a role in the development of Ulcerative Colitis. The beneficial bacteria within your gut help with digestion and maintaining colon health. The detrimental bacteria trigger the bodys immune system to send immune cells to the intestine. The constant presence of these immune cells in the intestine leads to chronic inflammation, which is associated with Ulcerative Colitis symptoms. This is where probiotics come in.
Probiotics may help relieve Ulcerative Colitis symptoms by restoring a healthy balance of bacteria within your intestine. When beneficial bacteria are added to the gut and balance is achieved, the immune system no longer needs to send cells to the area and the inflammation resolves along with your Ulcerative Colitis symptoms.
If you do begin taking a probiotic supplement, it may not have an immediate effect on your Ulcerative Colitis symptoms. You will need to take a probiotic supplement for at least seven to ten days to begin to build up the good bacteria in your gut. Additionally, to continue to see their benefits, you will need to continue to take the probiotics. Stopping the supplement may even shift the balance of bacteria in a negative way and trigger a flare.
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
Also Check: Does Stress Cause Ulcerative Colitis
Diet Progression Following Flares For Ulcerative Colitis And Crohns Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
Butter Made With Nuts
Nut butter is an excellent source of protein and good fats, such as peanuts, almonds, cashew, and other varieties. If you want to avoid having to chew up challenging nut chunks, choose creamy peanut butter instead of chunky, which could aggravate your stomach during a flare-up.
Consider consuming peanut butter on bread or in a tortilla. Nut butter on saltines or other low-fiber crackers is another excellent option.
Also Check: Sand Beds For Pressure Ulcers
List Of Foods To Eat To Keep Colitis From Flaring Up
Colitis is an inflammatory bowel disease. There are several types of colitis, depending on the location of the inflammation. Symptoms vary but commonly include abdominal cramps, bloating, constipation and diarrhea. Theres really no nutritional therapy for colitis, nor is there a cure. But learning to strike a balance between getting the nutrients you need and avoiding the foods that seem to trigger your symptoms can help you manage the condition.
Video of the Day
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Recommended Reading: What Does A Venous Leg Ulcer Look Like
What Foods Can I Eat When I Am Having An Ulcerative Colitis Flare
Certain foods are less likely to make your UC symptoms worse and can also help to reduce inflammation. These foods help settle your stomach and ensure you receive enough vitamins and minerals during an UC flare and include:
- Low-fiber fruits such as bananas, cantaloupe, honeydew melon, and cooked or canned fruits
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Refined grains, found in sourdough, potato or gluten-free bread, white pasta, white rice, mashed potatoes, and oatmeal
- Fully cooked, de-seeded, skinless, non-cruciferous vegetables such as asparagus tips, cucumbers, potatoes, and squash
- Homemade protein shakes or oral supplements
- Use olive oil instead of other oils or fats
Youre Not Drinking Enough Fluids
If youre experiencing bouts of diarrhea, you run the risk of becoming dehydrated, because your body is losing more fluids than its taking in. This can be harmful to your overall well-being and interfere with your bodys ability to heal.
Drink as much water as you can during a UC flare. Just keep in mind that there are some liquids you should think twice about if you have diarrhea, including pear, peach, or prune juice, according to the Crohns & Colitis Foundation all of them contain nonabsorbable sugars that can be rough on your gut. Try, too, to avoid alcohol, caffeinated drinks, and carbonated beverages.
Don’t Miss: Best Supplement For Horses With Ulcers
Green Banana & Applesauce
Both green bananas and cooked and cooled apples are high in soluble fibers and resistant starches which help to slow down transit and soak up excess moisture which can be helpful if diarrhea is a concern. According to theUniversity of Wisconsin Health, applesauce is helpful for ulcerative colitis and are a rich source of vitamins and minerals like potassium.
Diet Recommendations For Ulcerative Colitis Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages.
- Try incorporating more omega-3 fatty acids in your diet. These fats may have an anti-inflammatory effect. They are found in fish, including salmon, mackerel, herring and sardines.
- Patients often find that smaller, more frequent meals are better tolerated. This eating pattern can help increase the amount of nutrition you receive in a day.
- Consider taking nutritional supplements if appetite is poor and solid foods are not tolerated well .
You May Like: Causes Of Ulcers In Horses
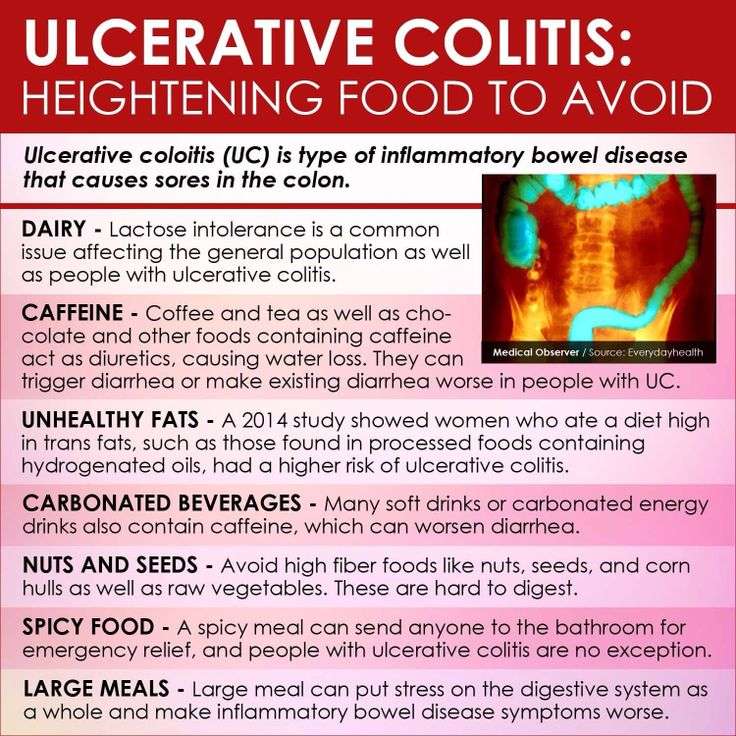
Foods To Avoid With Ulcerative Colitis
Although there are foods that are common triggers during both Ulcerative Colitis flares and remission, the list expands when youre experiencing active Ulcerative Colitis symptoms. Keep in mind that Ulcerative Colitis triggers differ from person to person, so the real key to long-term Ulcerative Colitis management is identifying what works for you. Easier said than done, right?
If youve ever searched on your own to figure out how to manage your Ulcerative Colitis, youve probably found a ton of information. The challenge is that the information on the internet can be contradicting and confusing. If youre struggling with Ulcerative Colitis, we recommend enlisting the help of a registered dietitian. They will be able to help you better understand your UC and determine what foods and behaviors most trigger your symptoms.
Remember to limit fiber when you are experiencing an Ulcerative Colitis flare. High fiber foods are part of a healthy, well-rounded diet. However, when UC symptoms are active, you may need to temporarily limit fiber intake to reduce inflammation and allow your gut to heal. High fiber foods are harder to digest and can trigger UC symptoms. High fiber foods include whole grains, fruits with skin and seeds, vegetables with skin and seeds, raw vegetables, cruciferous vegetables, nuts, seeds, beans and legumes.
Ulcerative Colitis Crohns Disease Or Something Else
The colon, also known as the large intestine, has three parts or section: ascending colon , transverse , descending colon , and the sigmoid colon just before the rectum.
Ulcerative colitis symptoms in each person will be different depending on where inflammation occurs and how bad it is. The most common symptoms include:
There are common complications that tend to come with UC, even though they are not actually a direct result of this chronic health condition. Fever, fatigue, and anemia are perhaps the most common additional symptoms. Additionally, inflammation beyond the colon often shows up as skin sores, skin rashes, mouth sores, joint pain, red and painful eyes, and sometimes even liver disease.
While both are referred to as inflammatory bowel disease or IBD, and Ulcerative colitis is related to Crohns disease, they are still different. Crohns disease, unlike ulcerative colitis, is not limited to the colon and is a chronic inflammatory disease of the intestines or the entire GI tract. Crohns often affects the small intestine and colon although occasionally it, too, is limited to the colon.
Also Check: Venous Stasis Ulcer Right Lower Leg Icd 10
Don’t Miss: How Do You Test For An Ulcer In The Stomach
How Can I Live With Chronic Ulcerative Colitis
If you are struggling with colitis or another type of irritable bowel disease, help is available at Gastroenterology Associates of Southwest Florida, PA. Our team provides compassionate, expert care to help patients suffering from these types of chronic conditions. Find out how we can help you live with chronic ulcerative colitis
You May Like: Cbd Oil For Stomach Ulcers
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Don’t Miss: Stomach Ulcer Over The Counter
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Recommended Reading: Hind Gut Ulcers In Horses Symptoms
What Foods Should I Avoid

Certain foods can exacerbate UC flares, but everyone has different trigger foods. For some, it might be a juicy burger and for others, it could be their morning latte.
In general, inflammatory foods, like fast food, processed food, alcohol, and sugary drinks contribute to the development of flares, says Dr. Singh. Freuman adds that saturated fat, specifically, can be an issue for certain people. Foods that contain significant amounts of saturated fat include:
- Whole-milk dairy, such as cheese, cream, butter, and full-fat yogurt
Lactose is the sugar present in milk and dairy products, and lactase is the enzyme people need to break down those sugars during digestion. If someone is lactose-intolerant, it means they dont produce enough lactase to break down the sugars, which can cause cramps, bloating, diarrhea, and gas.
To complicate matters, UC is sometimes coupled with lactose intolerance. But lactose intolerant dairy lovers, take heart: Its often possible to still consume dairy with lower lactose content, like cottage cheese and yogurt. Because these products contain live cultures that produce their own lactase, your body doesnt have to do all the work to break down lactose5.
Thats a win-win, since dairy foods provide important nutrients, like calcium and vitamin D, to your diet. In fact, avoiding them completely is not recommended unless 100% necessary.
Read Also: Surgical Management Of Ulcerative Colitis Ppt
Do Any Medications Have Nutritional Side Effects
Moderate to severe flares of IBD are often treated with corticosteroids , cholestyramine and 5-ASA compounds . These medications have nutritional side effects that should be addressed. If you use any of these medications, talk to your doctor or registered dietitian for treatment advice.
- Prednisone causes decreased absorption of calcium and phosphorus from the small intestine. It also causes increased losses of calcium, zinc, potassium and vitamin C. With continual use of high doses of prednisone, the result may be bone loss and development of bone disease. People on prednisone may need up to 1200 milligrams a day. Protein needs also are increased for people taking prednisone because it increases protein breakdown in the body.
- Cholestyramine decreases absorption of fat-soluble vitamins , as well as folate, vitamin B-12, calcium and iron.
- Sulfasalazine interferes with folate absorption. People taking this drug also should take a 1 milligram folate supplement each day.