The Formation Of Exudate
The normal wound healing response of inflammation leads to the development of local oedema. Histamine, released from damaged cells as a result of injury, causes plasma leakage from blood vessels and, as a consequence, oedema forms in adjacent tissues. This exudate seeps from the wound surface, initially taking the form of a clear, serous liquid. Later, it becomes more viscous and opaque, as it contains leucocytes and other constituents such as albumin, macrophages and cellular debris .
Although there is limited understanding of exudate formation, Thomas lists some of the factors that may influence its production .
When a wound deteriorates, it may exhibit an increase in exudate production, accompanied by soiling of clothes or bedclothes, a change in odour, and possibly leakage from dressings.
The optimal level of exudate for a wound The optimal level of exudate required to facilitate healing has not yet been determined. In addition, it varies with different types of wound. Increased levels of wound exudate may promote bacterial wound colonisation , particularly in wounds that are not appropriately managed. However, despite the possibility of dressings becoming soaked and strike-through providing potential access for bacteria, there is little evidence to support the theory that this increases the risk of infection.
What Is Zinc Oxide
Zinc is a trace element very abundant in the body. While it is known that zinc deficiency can cause delayed wound healing, the actual role of zinc in wound healing was not known. A number of experimental studies and clinical trials have been conducted using zinc. Results showed that topical zinc oxide had increased wound healing, increased reepithelialization, decreased rates of infection and decreased rates of deterioration of ulcers. Topical zinc oxide has shown to improve the rate of wound healing in patients, regardless of their zinc status. Oral zinc supplementation in zinc deficient patients did not have the same effect.
The animal studies reviewed showed that zinc sulfate did not enhance wound healing, but delayed it. One of the major roles for zinc in wound healing was found that zinc oxide enhances the ability of matrix metalloproteinases to enzymatically break down collagen fragments. There are few clinical studies, but they have all shown a positive benefit for topical zinc oxide, and of interest, especially when used for debridement in burns.
Further research on the topic of zinc in wound management has been recommended, but for now, I would say use zinc oxide whenever possible. I certainly will continue using it in my wound care practice, especially now I know it is actively helping the wound.
Reference:Kogan S, Sood A, Granick M. Zinc and Wound Healing: A Review of Zinc Physiology and Clinical Applications.Wounds. 2017 29: 102-106.
What Kind Of Dressing Do You Use On A Stage 4 Pressure Ulcer
If a pressure ulcer is at-risk of infection or has become infected, an antimicrobial silver foam dressing may be helpful. Alternatively, a silver alginate dressing in combination with a foam dressing may be used. It is important to select a debridement method most appropriate to the person’s condition.
Recommended Reading: How To Use Aloe Vera Gel For Ulcerative Colitis
What Are The Causes Of Stage 2 Pressure Ulcers
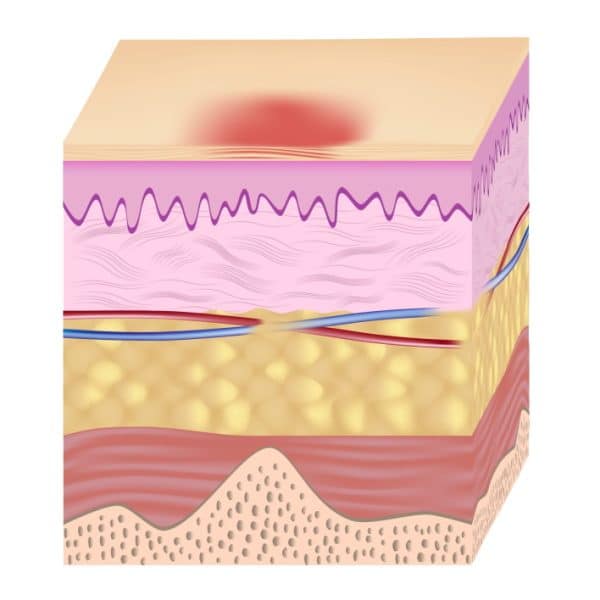
Pressure ulcers can occur mainly due to three different forces:
-
Prolonged Pressurev – When a person applies constant pressure against the bony surface for a long time, it can result in a pressure ulcer. When this pressure goes beyond the tissue capillary pressure, the surrounding tissues deprive oxygen, leading to tissue necrosis.
-
Shearv – Shear happens when the deep fascia slides over the skeletal muscle, which can compress the blood vessels leading to ischemia and tissue necrosis.
-
Frictionv – Friction is the opposite of shear force. Friction causes microscopic and macroscopic tissue trauma when the patient moves through the support surface.
Related TopicsCommon Penile Disorders – Causes, Diagnosis, Prevention, and Treatment
Further, moisture from incontinence, wetness, or exudate increases the friction between the surface and the skin. It weakens the epithelial bonds making the skin more liable to pressure, shear, and friction damage.
Stage 1 pressure ulcers do not cause skin breaks, but disposing of the same area to any forces after an ulcer is formed can tear the skin, developing stage 2 pressure ulcers.
Appendix 11 Time To Event Data: Direct Evidence
The duration of followup ranged from 3 to 26 weeks, but the distribution was insufficient to allow modelling of time dependence in the network.
Seven studies reported timetoevent data. We calculated the hazard ratio using the method and spreadsheet from Tierney 2007 one study reported the hazard ratio directly, adjusted for exudate level. The timetohealing data are shown in Analysis 3.1 and summary statistics for the timetohealing and the proportion healed are compared in Table 22 for the studies that report both healing outcomes.
In the individual network, two studies in 95 participants suggested that the time to healing may have been quicker for hydrocolloid versus saline gauze there was no heterogeneity . One study in 24 participants suggested healing may have been quicker for collagenase ointment compared with hydrocolloid . In the other studies, the CI showed much uncertainty.
There was some suggestion of a time dependent effect because there were qualitative and quantitative differences between the HR and the RR: for shorter studies , the HR gave a smaller effect than the RR, but for the medium and longer term studies the HR gave a larger effect than the RR, suggesting that wounds that heal do so relatively quickly.
Analysis
Comparison 4 Direct evidence: group interventions, timetohealing data, Outcome 1 Timetohealing .
Recommended Reading: How To Manage Ulcerative Colitis Pain
Quality Of The Evidence
We have explored the application of a new approach to GRADE analysis, alongside NMA in STATA . We applied the GRADE approach separately to effect estimates for different contrasts and to the ranking of interventions, but the two aspects are closely interrelated and, in this review, are a consequence of the sparse network and the high risk of bias through much of the network. The effect estimates were exemplified by contrasts of interventions versus saline gauze.
Across the network as a whole, the evidence was of very low certainty. There was overall high risk of bias and overlap of the ranking probability distributions, and no clearcut results. The evidence was of such poor quality that we consider it inappropriate to focus on which treatments had the highest probabilities of healing .
Improve Skin Resistanceexpand: More
Linovera® is a product range made of hyperoxygenated fatty acids . Indicated for prevention and treatment of stage 1 pressure ulcers as well as lower limb ulcers and diabetic foot ulcers .
The products promote blood microcirculation, reducing the risk of ischemia and facilitating the renewal of epidermal cells. They protect against friction, reduce skin fragility and help to prevent dehydration of the skin.
Read Also: Are Mouth Ulcers A Sign Of Hiv
Severity Of Pressure Ulcers
Healthcare professionals use several grading systems to describe the severity of pressure ulcers most common is the EPUAP grading system. Pressure sores are categorised into four stages corresponding to the depth of damage. It must however be emphasised that when an eschar is present, accurate staging is not possible.
Donât Miss: What Causes A Bleeding Ulcer In Stomach
How Can Pressure Ulcers Be Treated
It is important to watch out for early signs of pressure ulcers and to contact your doctor if you notice any changes to the skin. Ulcers are best managed early on, and your doctor will assess whether your pressure ulcer can be managed at home, if you need a referral to a wound specialist or if you require treatment at hospital.
Use healthdirects Service Finder tool to locate your nearest GP or nurse clinic.
Wound dressings can enhance healing. Your healthcare team will select the most appropriate treatment and dressing, depending on your specific pressure ulcer. There are 6 classes of dressings:
- alginate absorbent fibre dressings
Depending on the type of pressure ulcer, a bandage may also be applied to keep the dressing in place or support the injured area.
To promote healing and recovery, it is important to eat a balanced diet that includes protein, carbohydrates, fats and sufficient fluids.
Other treatments may include antibiotics if the ulcer becomes infected, or debridement a procedure used to clean the wound and remove any damaged tissue.
Don’t Miss: How To Treat Severe Ulcerative Colitis
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
- the Cochrane Wounds Specialised Register
- the Cochrane Central Register of Controlled Trials
- Ovid MEDILINE
- EBSCO CINAHL Plus .
We also searched the following clinical trials registries:
- ClinicalTrials.gov
- WHO International Clinical Trials Registry Platform
- EU Clinical Trials Register .
Searching other resources
Ease Pressure Reduce Frictionexpand: More
Askina® Heel is a non adhesive hydrocellular heel dressing that protects the heel area from shear stresses and reduces pressure from external forces.
Description
Partial-thickness skin loss with exposed dermis superficial
- Manage bacterial load and odor
- Manage exudate and promote moist healing
- Protect the periwound skin
Also Check: Early Warning Signs Of Ulcerative Colitis
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
What Types Of Wound Dressing Can Be Used On Bed Sores

By Nursing Home Law Center
In order for bed sores to heal, attention must be paid to the removing dead tissue and protecting the wound from infection causing bacteria. Dressings are usually applied to help the body heal itself. The type of dressing and the frequency with which it is to be changed is ordered by a physician with the application and changes carried out by nurses.
Many patients with bed sores suffer additional harm when the staff responsible for caring for them fails to follow medical orders with respect to the frequency with which dressings are to be changed. If dressings are not changed according to orders set forth by a physician, the healing of the bed sores may be delayed and perhaps become infected.
The most commonly used dressings used to treat bed sores include:
Absorptive Dressings: These dressings are either applied directly to the wound or on top of other primary dressings. Absorptive dressings are intended to remove the drainage from the bed sore that may impede healing. Most absorptive dressings are changed on a daily basis. However, excessive drainage from a bed sore may require more frequent dressing changes.
Common types of Absorptive dressings include: Medipore, Silon Dual Dress, Aquacel Hyrofiber Combiderm, Absorbtive Border, Multipad Soforb, Iodoflex, Tielle, Telefamax, Tendersorb, Mepore and Exu-dry.
Related Information
Also Check: Does Colectomy Cure Ulcerative Colitis
Prevalence Incidence And Health
In the USA, approximately 13 million people develop pressure ulcers each year, and more than 2.5 million patients in the United States acute care services suffer from pressure ulcers, and 60,000 each year die from the complications of such ulcers. In the United States between 1990 and 2000, the NPUAP reported a prevalence rate of pressure ulcer ranging from 10% to 18% in general acute care, 2.3% to 28% in long-term care and up to 29% in home care, and 0% to 6% in rehabilitative care. Pressure ulcers can diminish global life quality because of pain, management procedures, and increased length of hospital stay. Furthermore, they contribute to rapid mortality in some patients. Therefore, any intervention that may assist to avoid pressure ulcers or to treat them may be important to decrease the cost of pressure ulcer care and increase life quality of affected individuals. Pressure ulcer management costs are a major problem to healthcare organizations. In the UK, the cost is estimated at £1.4£2.1 billion annually and in the US is estimated at $1.6 billion. In Australia, budgets spent per each patient admitted to Intensive Care Units have been around $18,964. In the UK, the reported cost of care for pressure ulcers has been 4% of total healthcare costs.
Appendix 1 Pressure Ulcer Grading
One of the most widely recognised systems for categorising pressure ulcers is that of the National Pressure Ulcer Advisory Panel . Their international classification recognises four categories or stages of pressure ulcer and two categories of unclassifiable pressure injury, in which wound depth and/or extent, or both, cannot be accurately determined unclassifiable pressure ulcers are generally severe and would be grouped clinically with Stage 3 or Stage 4 ulcers :
The two additional categories of unclassifiable wounds are:
- Unstageable/unclassified Obscured fullthickness skin and tissue loss: Fullthickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
You May Like: How To Cure Ulcerative Colitis With Diet
Nursing Home Abuse & Neglect Resources
Common Cases:
Client Reviews
Nursing Home Law Center, LLC is not a law firm. It is an organization that concentrates solely on helping provide nursing home patients and their families the legal help they need. NHLC LLC has a network of recognized attorneys located across the country who have experience representing clients in all types of nursing home injury cases. References to NHLC attorneys or our attorneys are references to attorneys within NHLCs network, and not employees, agents, or partners of NHLC. Please consult the disclaimer page for further information concerning NHLC. All information on this site shall be considered attorney advertising and not construed as legal advice. Prior case results should not be relied on when retaining a lawyer.
Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in Appendix 2.
You May Like: Stage 1 Vs Stage 2 Pressure Ulcer
Agreements And Disagreements With Other Studies Or Reviews
We have been unable to identify any network metaanalyses directed at healing pressure ulcers and incorporating both dressings and topical agents. The AHRQ guideline reviewed the evidence for dressings in a series of pairwise comparisons and stated that overall, they did not find substantial evidence to support certain local wound applications over others . The most recent NICE guideline on the prevention and management of pressure ulcers considered all RCT evidence on dressings and separately all RCT evidence on topical agents. NICE recommendations are to not use saline gauze dressings and for the health professional and adult to discuss the type of dressing to use, taking into account pain and tolerance, position of the ulcer, amount of exudate and frequency of dressing change. These recommendations rely heavily on consensus decisions, weakly supported by the evidence, and as such, agree with the findings of this review.
Spotlight On Aging: Pressure Sores
|
Aging itself does not cause pressure sores. But it causes changes in tissues that make pressure sores more likely to develop. As people age, the outer layers of the skin thin. Many older people have less fat and muscle, which help absorb pressure. The number of blood vessels decreases, and blood vessels rupture more easily. All wounds, including pressure sores, heal more slowly. Certain risk factors make pressure sores more likely to develop in older people: |
Causes that contribute to the development of pressure sores include
Pressure on skin, especially when over or between bony areas, reduces or cuts off blood flow to the skin. If blood flow is cut off for more than a few hours, the skin dies, beginning with its outer layer . The dead skin breaks down and an open sore develops. Most people do not develop pressure sores because they constantly shift position without thinking, even when they are asleep. However, some people cannot move normally and are therefore at greater risk of developing pressure sores. They include people who are paralyzed, comatose, very weak, sedated, or restrained. Paralyzed and comatose people are at particular risk because they also may be unable to move or feel pain .
Friction can lead to or worsen pressure sores. Repeated friction may wear away the top layers of skin. Such skin friction may occur, for example, if people are pulled repeatedly across a bed.
-
Assessment of nutrition status
-
Sometimes blood tests and magnetic resonance imaging
Read Also: How To Manage Ulcer Pain