Active Uc Of Any Extent Not Responding To Aminosalicylates
In mild-to-moderate UC of any extent, aminosalicylates such as mesalamine are the preferred initial treatment . In patients with disease activity limited to the rectum, topical therapy alone might suffice, but combination therapy is more effective and is also recommended for left-sided and extensive UC . Table 2 gives an overview on current treatment options.
Table 2.
Medical therapy for UC
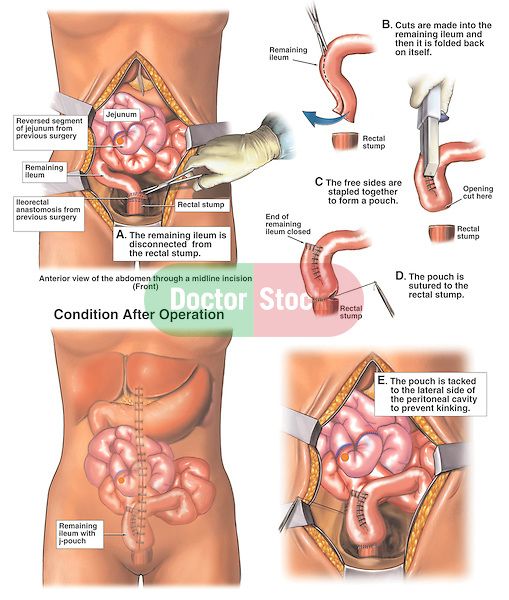
Fig. 1.
Active ulcerative colitis of any extent not responding to 5-aminosalicylates . MMX, multimatrix AZA, azathioprine 6-MP, 6-mercaptopurine.
Except in case of isolated proctitis, where topical corticosteroids alone may be considered, treatment with oral corticosteroids should be initiated in patients who do not respond adequately to 5-ASA . In case of isolated proctitis, topical corticosteroids alone might be considered. The introduction of corticosteroids should be a shared decision-making process that includes patients preference of therapy and tolerance to 5-ASA. It is, however, recommended to start corticosteroids in patients with sustained rectal bleeding for 2 weeks, persistent abdominal symptoms after 6 weeks of adequate therapy with 5-ASA or if symptoms deteriorate . In selected cases, a prolonged therapy with up to 16 weeks might still be able to achieve remission.
You May Like: What Is An Ulcer Diet
Are Food Triggers The Only Cause Of An Ulcerative Colitis Flare
Regardless of your diet, there may be times when your ulcerative colitis symptoms seem to disappear completely for months at a time before making a dramatic reappearance. When this happens, its .
But the foods youre eating arent the only possible culprit. Emotional stress, not taking medications as prescribed, and use of certain medications, like steroids and antibiotics, can also trigger ulcerative colitis flares, according to the Cleveland Clinic.
Flares take different forms for different people, and theres no formula that predicts what will bring them on. Different people will claim a medicine or anxiety will set their symptoms off. But some people just seem to have had flares when they have flares, and you can drive yourself crazy trying to find the cause, Dr. Schwimmer says.
Surgery For Inflammatory Bowel Disease
NYU Langone gastroenterologists work closely with colorectal surgeons and other specialists to provide comprehensive, advanced care for individuals who have been diagnosed with inflammatory bowel disease, or IBD. If medication is not effective in achieving remission and alleviating symptoms, or if the results of endoscopic or imaging studies suggest that chronic inflammation has led to serious damage in the lining of the digestive tract, your doctor may recommend surgery.
Colorectal surgeons at NYU Langone’s Inflammatory Bowel Disease Center specialize in procedures to remove diseased areas of the large or small intestine while leaving as much of the bowel intact as possible. Our surgeons use robotic-assisted techniques designed to minimize the size of abdominal incisions and protect the surrounding muscle and soft tissue.
Also Check: Stage 2 Pressure Ulcer Characteristics
Perforation Of The Colon
Chronic inflammation caused by ulcerative colitis can weaken the wall of the colon until a hole, or perforation, develops. Once the colon has been perforated, the contents of the intestine can spill into the abdomen and cause a serious infection called peritonitis.
This is a potentially life-threatening condition that needs immediate medical treatment.
Purpose Of Ileostomy Or J

Surgery is used to treat ulcerative colitis for a few different reasons.
The first reason to have a colectomy for ulcerative colitis is that the condition is no longer treatable with medications. There are many different drugs that are used to treat the condition. However,the available drugs may not significantly reduce inflammation.
Some of the medications used to treat ulcerative colitis may need time to work to get the disease under control. It can also occur that the disease becomes severe enough that theres not enough time for the drugs to work.
While not common, ulcerative colitis is also associated with colon cancer. The risk of colon cancer increases after having the disease for about eight to 10 years. If there are changes in the colon that might lead to colon cancer, surgery to remove the colon might be the best option.
Surgery might also be done to treat complications. Two of those include toxic megacolon and a perforation in the intestine. These are rare emergencies, but they would be a reason for a colectomy surgery.
Another reason to have surgery for ulcerative colitis is to improve quality of life. A patient might decide that the symptoms of the disease are keeping them from living a full, happy life, and surgery offers an opportunity for improvement.
Read Also: What Is Good For Ulcer Pain
What You Should Know About Proctocolectomy
-
The ileum will be brought through a hole in your abdominal wall called a stoma, which allows waste to drain out of your body.
-
The stoma will be about the size of a quarter and protrude slightly from your abdomen. A healthy stoma is pinkish in color, and appears moist and shiny.
-
An external ostomy pouching system will attach to the stoma and be worn at all times to collect waste.
-
The typical site for an ileostomy is the lower abdomen to the right of the navel, just below the belt line.
-
Some patients may still feel as if they need to have a bowel movement after their surgery, just as people who have lost a limb sometimes still feel as if the limb is still there. This called phantom rectum and it is completely normal. It does not require any treatment and often subsides over time.
Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
Also Check: Snack Foods For Ulcerative Colitis
Signs Of Possible Colitis
General signs of colitis can include:
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.
Also Check: Ulcers In Small Bowel Crohnâs
Choice Of Ileal Pouch Size And Type
Although most surgeons do not use the S pouch as the first option , the spout created in its construction provides an additional 3-5 cm in length to the entire ileal reservoir, as compared with the length of a J pouch.
Some still advocate straight ileoanal pull-through anastomosis without reservoir construction. Straight endorectal pull-through causes dilatation and compensation over time so that the pouch develops a reservoir function. In addition, length is generally not a problem with a straight pull-through. Thus, many pediatric surgeons perform this as their primary procedure. Good long-term outcomes and patient satisfaction are reported.
However, others have noted a need for revision of the straight pull-through configuration in 70% of cases. Construction of the ileal J pouchanal anastomosis is described below. One should keep in mind that the straight ileoanal pull-through is performed in essentially the same manner and uses less total length of small bowel.
In summary, the choice of pouch size and type involves a balance between increasing reservoir function to decrease stool frequency and the risk of developing pouchitis. All reservoirs have a tendency to enlarge over time. Consequently, most surgeons have opted for a smaller initial reservoir that depends on reservoir enlargement to gradually decrease stooling frequency while avoiding pouchitis.
Recommended Reading: Best Foods To Heal Stomach Ulcer
Early Recognition Close Monitoring And Timely Re
Any patient meeting the criteria for severe disease should be recognized promptly and admitted in the hospital. Stool cultures for enteric pathogens and Clostridium difficile should be taken at the earliest possibility but results should not be awaited before rapid IV corticosteroid therapy. Flexible unprepared sigmoidoscopy with minimal air insufflation should be performed within 24 hours of admission to confirm diagnosis and exclude a superimposed infection with the cytomegalovirus .3,8
Following initiation of corticosteroid therapy patients should be closely monitored with daily blood works, clinical examination and serial abdominal films as clinically indicated. Positive stool cultures should prompt treatment with antibiotics, presence of a significant amount CMV inclusions on colonic biopsy are an indication for ganciclovir treatment. Formal re-assessment is performed between days 3 and 5.3,8 As discussed above, current evidence does not allow for a singular recommendation. Failure of corticosteroid therapy is therefore based on a clinical, biochemical and radiological assessment. Several indices such as stool frequency, CRP and albumin levels and colonic dilatation on plain radiography can be used as described above.
Open Vs Laparoscopic Colectomy
The terms open and laparoscopic refer to how the colectomy surgery is performed. During an open colectomy, a surgeon makes a large incision in the abdomen to remove the colon tissue. In laparoscopic surgery, the surgeon makes very small cuts and uses flexible tools and cameras to see inside the body and remove the intestine.
You May Like: Carnivore Diet For Ulcerative Colitis
Elective Colorectal Cancer Surgery
Patients with Crohns disease and ulcerative colitis have a higher risk for colorectal cancer than the general population, so elective surgery may be recommended to eliminate that risk.
Colorectal cancer risk factors
-
The risk of CRC increases after living with IBD for 8 to 10 years
-
The risk increases the longer a person lives with IBD
-
The greatest risk is for people with IBD affecting their colon
-
Patients who have a family history of primary sclerosing cholangitis are also at higher risk of developing colorectal cancer
In most cases, colorectal cancer starts as a polyp, or a small lump growing from the wall of the intestine. Polyps typically start out benign but become cancerous over time. But in patients with IBD, abnormal and potentially precancerous tissue, called dysplasia, may lay flat against the wall of the intestine and can even be found in areas of the intestinal wall that appear normal during a colonoscopy.
Read Also: What Causes Mouth Ulcers On Gums
Ial Or Total Colon Resection
In a total resection, the entire large intestine is removed. While this is the only true cure for UC, it can reduce quality of life.
In a partial resection, colorectal surgeons remove the diseased region of the colon with a margin of healthy tissue on either side. When possible, the two remaining ends of the large intestine are surgically united, reconnecting the digestive system.
When this cant be done, the bowel is routed to the abdominal wall and waste exits the body in an ileostomy or colostomy bag.
Read Also: Ulcerative Colitis And Hip Pain
Quality Of Life And Satisfaction With Colectomy
The majority of respondents reported that they were somewhat satisfied, satisfied, or very satisfied with colectomy. Most also reported an improvement in their quality of life post-surgery, with 46 % stating that their current quality of life was very improved.
The results of the various survey tools applied are shown in Table . The median IBDQ score was 172 , with clinical remission generally scoring above 170. The mean EQ-5D index score was 0.79 and the mean EQ-5D VAS score was 77.0 .
Recommended Reading: Over The Counter Medication For Ulcerative Colitis
Questions To Ask Your Doctor
- Am I a candidate for surgery?
- How will this surgery affect my UC symptoms?
- What are the risks of this surgery?
- What are the possible short- and long-term complications?
- Which type of surgery is best for me?
- Have you worked with a surgeon who has performed this procedure before?
- What will recovery be like?
- Will I need to make any lifestyle changes?
- How will this surgery affect my day-to-day life?
For most people with UC, surgery is the last option after other treatment options have either failed or not provided the necessary relief.
Surgery options fall into two main categories. The key difference is where the waste pouch is placed following surgery.
Both types of surgery are intensive and require a lengthy recovery period. Before you make a decision, consult a variety of healthcare professionals, including your doctor, a surgeon, and an enterostomal therapist.
UC doesnt have a cure at the moment, but removing your colon and rectum does help treat the symptoms.
You may still live with many of the side effects of these surgeries long after the incisions have healed, though. Thats why its important that you feel prepared and informed about your options before going into the hospital.
You May Like: Do Ulcers Give You Diarrhea
When Is A Colectomy Necessary
Modern medical treatments for UC have improved significantly.
According to estimates, 15 in 100 people with UC may require a colectomy 10 years after receiving a diagnosis. However, this number is reducing, as scientists are continually developing better treatments.
The need for surgery varies depending on the severity of the disease and which area of the bowel it affects.
In general, though, 10 years after diagnosis:
- About 19% of people who have extensive colitis may require a colectomy.
- Close to 8% of those with left-sided colitis may need a colectomy.
- Approximately 5% of people with proctitis, which is inflammation of the lining of the rectum, may need a colectomy.
A person may need a colectomy for a number of reasons. These include:
There are two forms of proctocolectomy that surgeons typically perform for people with UC.
Actions For This Page
- Crohns disease and ulcerative colitis are collectively known as inflammatory bowel disease .
- Ulcerative colitis is located only in a persons large bowel .
- Diet and food allergies do not cause IBD.
- Medications help manage the symptoms of IBD.
- People with IBD can lead useful and productive lives.
- Some dietary changes can help you manage symptoms of IBD and allow medications to work better.
- Always talk with your doctor, healthcare specialist or dietitian before changing your diet. Arrange an emergency plan of action with your doctor, including after-hours phone numbers.
Recommended Reading: Can Ulcerative Colitis Cause Blood In Urine
You May Like: What Are The Signs And Symptoms Of Ulcerative Colitis
Inducing And Maintaining Remission In Uc: Do The Guidelines Agree
Despite the many similarities, there are a number of inconsistencies in the recommendations regarding the management of moderate-to-severe UC between the ACG and AGA guidelines .11,16 Whereas the ACG recommends the use of prednisone or oral budesonide MMX for induction of remission,16 the AGA does not address these therapies given its focus on immunosuppressives, biologics, and small-molecule therapies. However, despite being the drugs that everyone loves to hate, Dr Feagan commented that steroids are excellent induction drugs and good therapies to add on to biologics to get rapid symptomatic remission. He continued, It is imperative to get patients to symptomatic remission, and if you have to use steroids to get thereusing cessation of bleeding as a markeryou should use them.
Surgical Treatment Of Ulcerative Colitis
Restorative proctocolectomy with IPAA is the operation of choice for patients with UC it represents the only technique by which the substrate of the disease is completely removed and gastrointestinal continuity is reestablished. It is important to include the rectal mucosa down to the dentate line since residual tissue in this location may give rise to intractable pouchitis later on. Patients after IPAA can discontinue colitis-related medications, particularly immunosuppressants and immunomodulators, thereby avoiding associated adverse effects. In addition, the procedure substantially reduces the risk for dysplasia or cancer to the pouch itself in the rare cases where severe chronic pouchitis cannot be controlled.
Regular pouchography before closure of ileostomy.
In recent years, there has been a trend towards performing a three-step procedure . The reason for this seems to be an intensified conservative therapy with increasing use of biologics. This entails the risk of surgical complications due to an often significantly reduced general condition of the patient. The three-stage procedure offers a better control in these cases. In contrast, a one-stage operation should be reserved only for young patients with good sphincter function, low activity of inflammation, good general condition, low-dose immunosuppressive therapy, and a totally tension-free IPAA. In our series this ideal condition is met in less than 10% of all patients.
Don’t Miss: Best Vitamins For Ulcerative Colitis
Predictors Of Response To Steroids
Response to steroids is indicated by improvement in patients symptoms and improved laboratory parameters .
At day 3 of admission, response to steroids should be measured by assessing stool frequency and CRP levels .1). In the landmark study by Travis et al, which included patients with 51 episodes of severe UC, presence of more than 8 stools/d or 3-8 stools/d plus a CRP > 45 mg/L at day 3 predicted a colectomy rate of 85%. In another prospective study by Lindgren et al which included 97 episodes of severe UC, the following mathematical model was devised to predict colectomy: number of stoolsd + 0.14 Ã CRP 8 predicted a colectomy rate of 72%.
Algorithm for treatment decisions for patients with acute severe ulcerative colitis on intensive steroid therapy. AZA: Azathioprine.
Therefore regular assessment of response to steroids is of paramount importance in treating patients with acute severe UC. In a group of 80 patients who underwent emergency colectomy for severe UC between 1994 and 2000 in Oxford, patients with signicantly longer duration of preoperative medical therapy were more likely to have major post-operative complications.
Read Also: Is Okra Good For Ulcerative Colitis