Stages Of Pressure Ulcers And Treatment
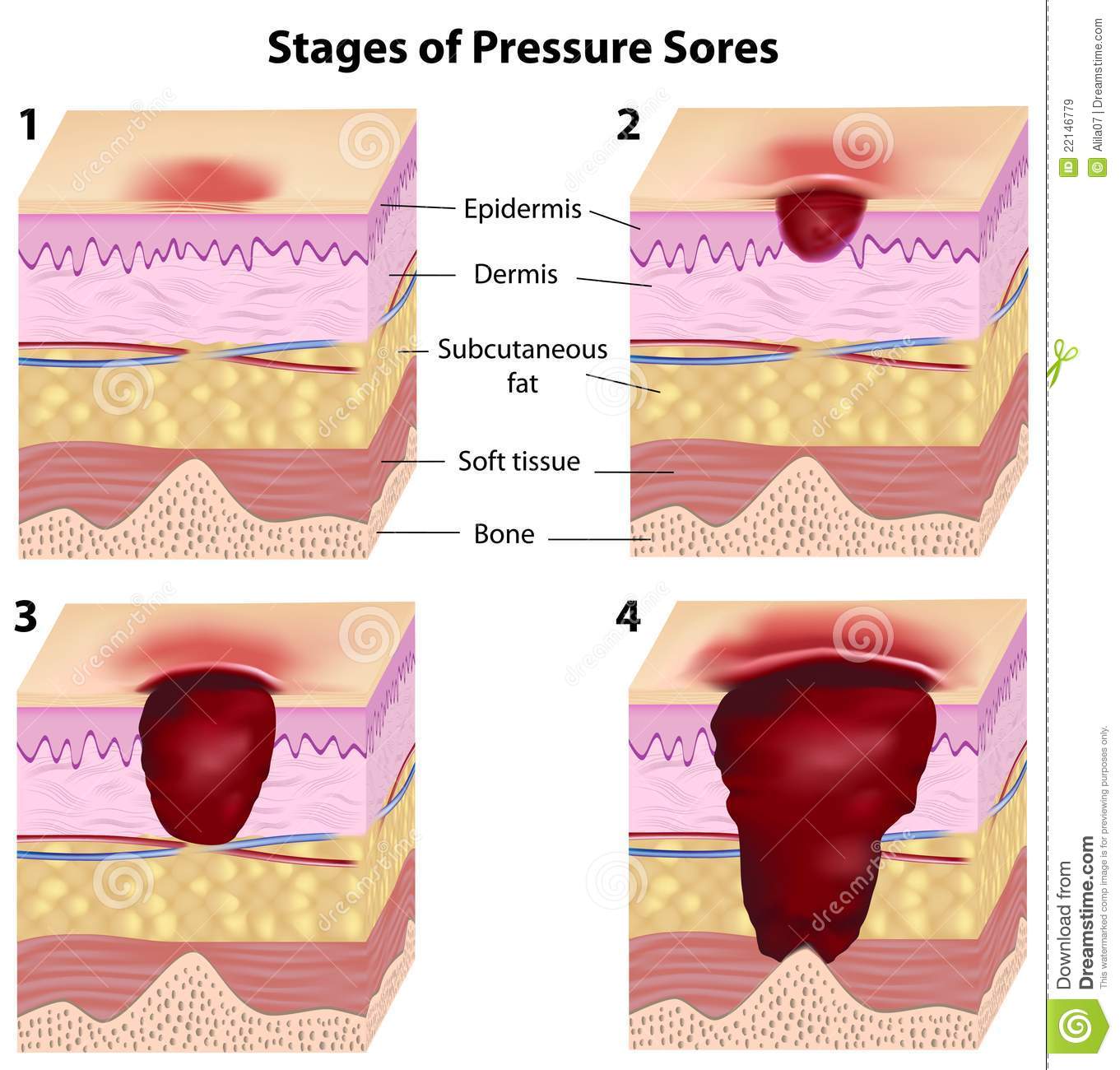
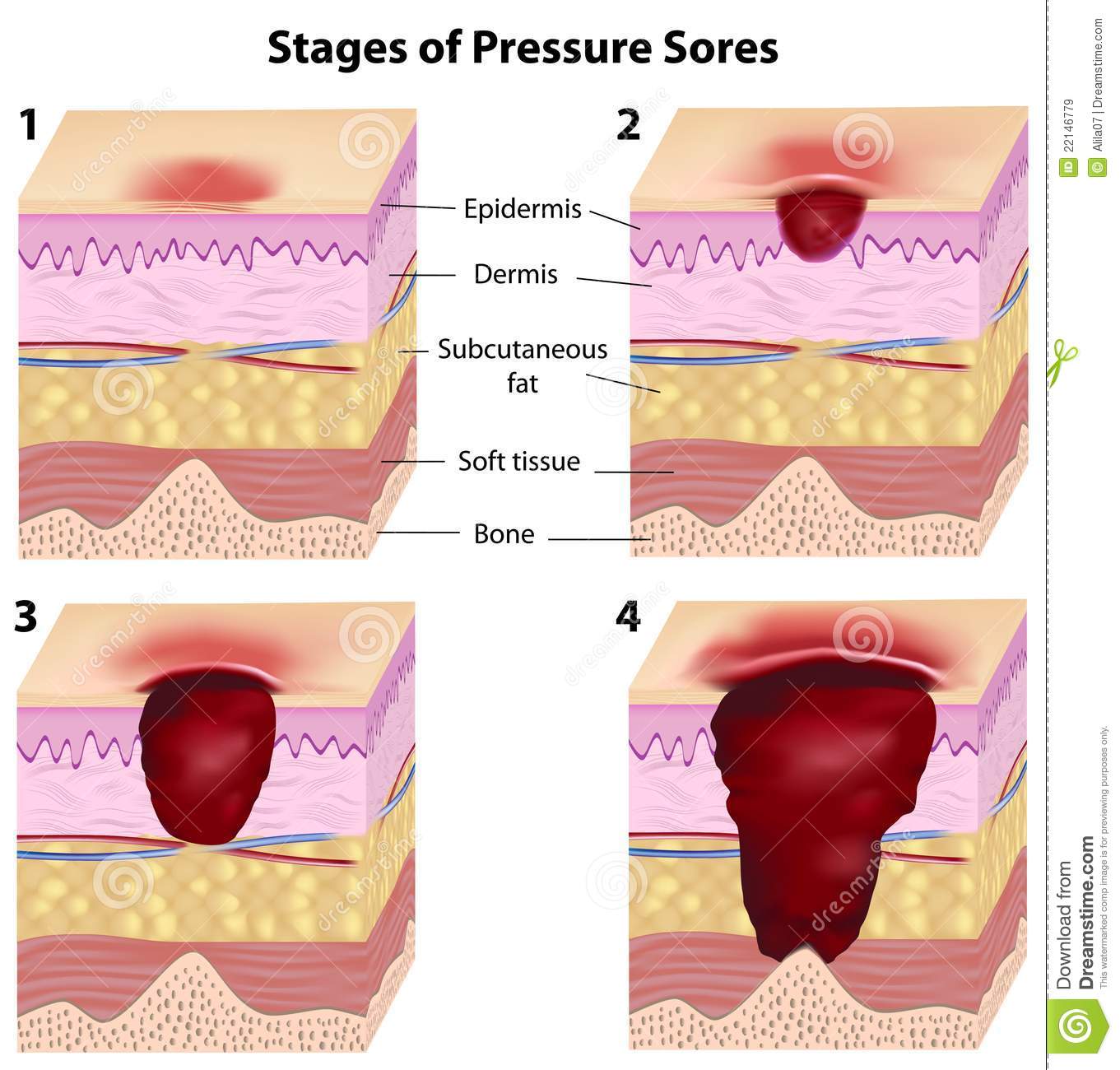
Pressure ulcers can progress in four stages based on the level of tissue damage. These stages help doctors determine the best course of treatment for a speedy recovery.
If caught very early and treated properly, these sores can heal in a matter of days. If left untreated, severe bedsores may require years to heal.
What Is The Icd Code For A Tailbone Pressure Ulcer
Pressure ulcer of coccyx Pressure ulcer of tailbone ICD-10-CM Alphabetical Index References for L89.15 Pressure ulcer of sacral region The ICD-10-CM Alphabetical Index links the below-listed medical terms to the ICD code L89.15.
What is the ICD 9 cm diagnosis code for 2012?
Free, official information about 2012 ICD-9-CM diagnosis code 707.03, including coding notes, detailed descriptions, index cross-references and ICD-10-CM conversion.
Recommended Reading: What To Eat To Help Ulcers
Pressure Ulcer Of Other Site Stage 4
- 20162017201820192020202120222023Billable/Specific Code
- L89.894 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2023 edition of ICD-10-CM L89.894 became effective on October 1, 2022.
- This is the American ICD-10-CM version of L89.894 – other international versions of ICD-10 L89.894 may differ.
- Healing pressure ulcer of other site, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, other site
- Applicable To annotations, or
Read Also: Does Stress Affect Ulcerative Colitis
Sacral Decubitus Ulcers Are A Certain Type Of Wound Located On The Lower Back At The Bottom Of The Spine
How to measure a sacral wound. Clock terms can also be used to describe the location of undermining. Use the body as a clock when documenting the length, width, and depth of a wound using the linear method. The braden risk assessment scale can be utilized to assess a patientâs risk of developing a pressure ulcer.
Get the wound depth using a cotton pledget or applicator dipped in a normal saline solution to measure the deepest part of the wound bed. Look closely at the wound and its edges, and then draw the wounds shape. Measure the wound how to measure wound size consistency is key.
Any adult who scores lower than 18 on the braden scale is high risk. For example, you might use words like jagged, red, puffy, or oozing to describe the wound.step 2, use a ruler to measure the length. Remove the applicator and hold it against the ruler to measure the depth of the wound margin based on.
This is particularly important when The total amount of tissue debrided should be listed separately from the wound measurements The six approaches for measuring wound area were simple ruler method , mathematical models , manual planimetry , digital planimetry , stereophotogrammetry and digital imaging method .
Step 1, draw the shape of the wound and write a brief description. Assessing and measuring wounds you completed a skin assessment and found a wound. In all instances of the linear method, the head is at 12:00 and the feet are at 6:00.
Archives Of Plastic Surgery
Can Bedsores Lead To Sepsis
What is the ICD-10 code for bed sores?
ICD-10-CM category L89 codes classify pressure ulcers, also known as bed sores, pressure sores or decubitus ulcers. Pressure ulcers are wounds caused by unrelieved pressure on the skin.
When do you code sepsis first?
When sepsis is present on admission and due to a localized infection , the sepsis code is sequenced first followed by the code for the localized infection.
What is the ICD code for a debridement sacral wound?
Read Also: Does Ulcerative Colitis Cause Headaches
Management Of Sacral Ulcers Varies By Ulcer Stage
It is important to properly stage pressure ulcers for several reasons, but two of the most important are for prognosis and management planning. Stage 1 and stage 2 pressure ulcers heal by regenerating tissue in the wound. Stage 3 and stage 4 pressure ulcers, on the other hand, heal through scar formation, which means the borders of the wound contract as it heals.
For Stage 1 sacral ulcers, the primary goal of therapy is to ensure adequate tissue perfusion and to protect the wound from further damage.2 This means preventing the sacrum from chronically squeezing the skin and preventing blood flow to the area. The goal of therapy for Stage 2 ulcers is to encourage tissue regeneration and protect the wound surface. For stage 3 or 4 ulcers, management efforts are focused on promoting tissue granulation and epithelialization.
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
- Use positioning devices to prevent prolonged pressure bony prominences.
- Keep the head of the bed as low as possible to reduce risk of shearing.
- Keep sheets dry and wrinkle free.
Also Check: Can Ulcers In The Esophagus Cause Cancer
Pressure Ulcer Of Sacral Region Stage 3
- 20162017201820192020202120222023Billable/Specific Code
- L89.153 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2023 edition of ICD-10-CM L89.153 became effective on October 1, 2022.
- This is the American ICD-10-CM version of L89.153 – other international versions of ICD-10 L89.153 may differ.
- Healing pressure ulcer of sacral region, stage 3
- Pressure ulcer with full thickness skin loss involving damage or necrosis of subcutaneous tissue, sacral region
- Applicable To annotations, or
Info For Medical Coders On How To Properly Use This Icd
- Inclusion Terms:
Inclusion Terms
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
- Healing pressure ulcer of sacral region, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, sacral region
Also Check: Natural Remedies For Mouth Ulcers
Whos At Risk Of Stage 4 Bedsores
Anyone with a lower-stage bedsore is at risk of a stage 4 sore. However, some patients may be more prone to this type of injury.
At particularly high risk are those:
- With Limited MobilityMovement is the key to preventing bedsores of any stage. If an older person cannot move on their own, they may sit or lie in the same position for hours. This can cut off blood flow to their skin and cause a bedsore.
- Who Are In Understaffed Nursing HomesNursing home residents with mobility issues must rely on staff members to prevent bedsores. Sadly, some care facilities may fail to prevent bedsores due to issues like understaffing and poor training.
- Who Have Alzheimers or DementiaIf residents with mental impairments develop a bedsore, they might not be able to tell anyone due to their condition. Theyll need to have someone else find it and help them get the proper care. Residents with these conditions may also have trouble sensing pain.
- Other FactorsResidents are at higher risk of bedsores if they have blood flow or circulation problems, diabetes, or poor nutrition or if they wear a cast.
Our trusted advocates can help you and your loved one take legal action. Call us today at .
Enhancing Healthcare Team Outcomes
The main goal is to prevent a decubitus ulcer by decreasing the pressure acting on the affected site. This goal requires an interprofessional team, including primary care providers, wound care specialists, surgeons, specialty-trained wound nurses, physical therapists, and nurses aides. Nurses provide care, monitor patients, and notify the team of issues. Nurses aides are often responsible for turning and repositioning patients. Air-fluidized or foam mattresses should be used, frequent postural changes, provision of adequate nutrition, and treatment of any underlying systemic illnesses. Debridement should take place to remove dead tissue that serves as the optimum medium for the growth of bacteria. Hydrogels or hydrocolloid dressing should be used, which aid in wound healing. Tissue cultures are necessary, so the most directed antibiotic can be administered, which can involve the pharmacist and the latest antibiogram data. The patient should be kept pain-free by giving analgesics. They should try to increase physical activity if possible, which a nurseâs aide, medical assistant, or rehab nurse can facilitate. Frequent follow-ups are an absolute necessity and a team approach to patient education and management involving the wound care nurse and wound care clinician will lead to the best results. These interprofessional activities can help drive better outcomes for patients with decubitus ulcers.
Donât Miss: How To Get Rid Of Stomach Ulcer Pain
Also Check: Natural Herbs To Treat Stomach Ulcers
Pressure Ulcer Icd 10 Symptoms
Early symptoms of a pressure ulcer ICD 10 include discoloration of skin. People with pale skin tend to have red spots and people with darker skin tend to have purple or blue spots.
Category 1 Pressure Ulcer ICD 10: Discolored stains may or may not turn white when pressed. The skin can feel warm and spongy. Pain or itching may occur in the affected area. Doctors and nurses refer to pressure ulcer ICD 10 at this stage as category 1 pressure ulcer ICD 10.
Category 2 Pressure Ulcer ICD 10: If the skin does not collapse, but the ulcer worsens, it may form an open wound or blister.
Category 3 Pressure Ulcer ICD 10: When the deep wound reaches deep into the skin layers.
Category 4 Pressure Ulcer ICD 10: When it reaches the muscles and bones.
Also Check: Blood Clots In Stool With Ulcerative Colitis
When To Use L89153 For Pressure Ulcer Of Sacral Region
Pressure ulcer of sacral region, stage 3 Billable Code. L89.153 is a valid billable ICD-10 diagnosis code for Pressure ulcer of sacral region, stage 3 . It is found in the 2021 version of the ICD-10 Clinical Modification and can be used in all HIPAA-covered transactions from Oct 01, 2020 Sep 30, 2021 .
Also Check: How To Cure A Bleeding Ulcer
The Dilemma Of Coding And Reporting Deep
Confusion and apprehension surround new guidelines for deep-tissue pressure injury.
The release of the 2020 Official Guidelines for Coding and Reporting has resulted in confusion and apprehension surrounding the intent of the new guideline related to the new ICD-10-CM codes for pressure-induced deep-tissue damage, or deep-tissue pressure injury .
The ambiguity stems from what appears to be conflicting advice found within the coding guidelines regarding pressure ulcer stage codes.
To provide history on the introduction of the new ICD-10-CM codes, we can reference the September 2018 Coordination and Maintenance Committee meeting. During this meeting, the following three points were discussed, based upon the request by the Centers for Medicare & Medicaid Services for Healthcare Research and Quality for new codes in order to identify and track deep-tissue injuries for surveillance and quality improvement purposes. The National Pressure Ulcer Advisory Panel serves as the authoritative voice for improved patient outcomes in pressure ulcer prevention and treatment through public policy, education, and research. In 2016, the NPUAP adopted several changes to pressure ulcer staging, based on recent clinical literature and expert consensus, which introduced minor inconsistencies with ICD-10-CM.
The guidelines referenced in this article are as follows:
Patient admitted with pressure ulcer evolving into another stage during the admission:
Pressure Ulcer Of Sacral Region Stage 4l89154
Chapter 12 – Diseases of the skin and subcutaneous tissue » Other disorders of the skin and subcutaneous tissue » Pressure ulcer of sacral region, stage 4
Hierarchy Tree View
YOU AGREE THAT THE INFORMATION PROVIDED ON THIS WEBSITE IS PROVIDED AS IS, WITHOUT ANY WARRANTY OF ANY KIND, EXPRESSED OR IMPLIED, INCLUDING WITHOUT LIMITATION WARRANTIES OF MERCHANTABILITY OR FITNESS FOR ANY PARTICULAR PURPOSE, OR NON-INFRINGEMENT OF ANY THIRD-PARTY PATENT, COPYRIGHT, OR ANY OTHER THIRD-PARTY RIGHT. IN NO EVENT SHALL THE CREATORS OF THE WEBSITE OR WASHINGTON UNIVERSITY BE LIABLE FOR ANY DIRECT, INDIRECT, SPECIAL, OR CONSEQUENTIAL DAMAGES ARISING OUT OF OR IN ANY WAY CONNECTED WITH THE WEBSITE, THE USE OF THE WEBSITE, OR THIS AGREEMENT, WHETHER IN BREACH OF CONTRACT, TORT OR OTHERWISE, EVEN IF SUCH PARTY IS ADVISED OF THE POSSIBILITY OF SUCH DAMAGES.
You May Like: How To Cure Ulcerative Colitis With Diet
Q& A: Clarifying New Guidance For Pressure Ulcers Deep
Q: Our coding department was told there were changes made for fiscal year 2020 when it comes to reporting healed/healing pressure ulcers and pressure-induced deep tissue damage. Can you explain any recent updates?
A: You are right, there have been updates to guidance surrounding these diagnoses.
First, the FY 2020 ICD-10-CM Official Guidelines for Coding and Reporting have additional clarity on patients admitted with pressure ulcers documented as healed. The guidelines added the phrase at the time of admission. The guidelines now state that there is currently no code assignment for pressure ulcers that are completely healed at the time of admission.
In contrast, if the pressure ulcer is documented as healing but not yet healed, the coder is to code the pressure ulcer to the appropriate pressure ulcer stage at the time of admission. Meaning, if the pressure ulcer was to the bone but improves during the stay to only include the depth of the subcutaneous tissue , the pressure ulcer is to be reported as a stage 4 pressure ulcer, not a stage 3.
If a pressure ulcer was present on admission and is healed at the time of discharge, the site and stage of the pressure ulcer at the time of admission should be reported. Remember, healed at the time of admission is the only time a pressure ulcer would not be reported, because it no longer exists.
- L89.126, pressure-induced deep tissue damage of left upper back
- L89.156, pressure-induced deep tissue damage of sacral region
Pressure Ulcer Of Unspecified Site Stage 4
- 2016201720182019202020212022Billable/Specific Code
- L89.94 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM L89.94 became effective on October 1, 2021.
- This is the American ICD-10-CM version of L89.94 other international versions of ICD-10 L89.94 may differ.
- Healing pressure ulcer of unspecified site, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, unspecified site
- Applicable To annotations, or
Read Also: How To Use Aloe Vera Gel For Ulcerative Colitis
You May Like: What Foods Not To Eat When You Have An Ulcer
Pressure Ulcer Icd 10 Diagnosis
When admitted to an acute or chronic hospital, patients must undergo a thorough skin examination to determine whether they have developed a pressure ulcer ICD 10 and whether they have symptoms of previous pressure ulcer ICD 10 . The assessment of the skin can be done with various tools, but the most common is the use of the Braden scale. This assessment includes the presence of previous ulcers and an assessment of the risk of developing pressure ulcer ICD 10.
The scale checks the following sensory parameters:
- sensation of the skin
- assessment of friction forces
- shear forces on the affected skin
The Braden scale is rated by a factor of 1 to 4, with the exception of frictional shear, which has three points on its scale. Points are added up to get a score.
The highest possible Braden score is 23. A patient with a score of 18 or less is considered at risk for pressure ulcer ICD 10. The general health and nutritional status of the patients are also assessed. Particular care is required to prevent pressure-related skin changes and risks. If the patient has a pressure ulcer ICD 10, it should be an ulcer that can be documented with photographic evidence.
Read Also: What Does Ulcerative Colitis Affect
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
What is a Pressure Ulcer?
There are many contributing factors.
Also Check: What Does An Ulcerative Colitis Flare Up Feel Like
Recommended Reading: What Foods Should I Avoid With Ulcerative Colitis