Neonates Infants Children And Young People: Risk Assessment
-
Carry out and document an assessment of pressure ulcer risk for neonates, infants, children and young people:
-
being admitted to secondary care or tertiary care or
-
receiving NHS care in other settings if they have a risk factor, for example:
-
significantly limited mobility
-
the inability to reposition themselves
-
significant cognitive impairment.
All Ages: Care Planning
-
Develop and document an individualised care plan for neonates, infants, children, young people and adults who have been assessed as being at high risk of developing a pressure ulcer, taking into account:
-
the outcome of risk and skin assessment
-
the need for additional pressure relief at specific at-risk sites
-
their mobility and ability to reposition themselves
-
other comorbidities
What Bundle Of Best Practices Do We Use
Given the complexity of pressure ulcer prevention, with many different items that need to be completed, thinking about how to implement best practices may be daunting. One approach that has been successfully used is thinking about a care bundle. A care bundle incorporates those best practices that if done in combination are likely to lead to better outcomes. It is a way of taking best practices and tying them together in a systematic way. These specific care practices are among the ones considered most important in achieving the desired outcomes.
The pressure ulcer bundle outlined in this section incorporates three critical components in preventing pressure ulcers:
- Comprehensive skin assessment.
- Standardized pressure ulcer risk assessment.
- Care planning and implementation to address areas of risk.
Because these aspects of care are so important, we describe them in more detail in the subsequent subsections along with helpful clinical hints. While these three components of a bundle are extremely important, your bundle may stress other aspects of care. It should build on existing practices and may need to be tailored to your specific setting. Whatever bundle of recommended practices you select, you will need to take additional steps. We describe strategies to ensure their successful implementation as described in Chapter 4.
The challenge to improving care is how to get these key practices completed on a regular basis.
Resources
Additional Information
Tools
Practice Insights
Recommended Reading: How To Cure Colon Ulcers
What Are The Stages Of A Pressure Injury
There are four stages that describe the severity of the wound. These stages include:
- Stage 1: This stage is discolored skin. The skin appears red in those with lighter skin tones and blue/purple in those with darker skin tones. The skin does not blanch when pressed with a finger.
- Stage 2: This stage involves superficial damage of the skin. The top layer of skin is lost. It may also look like a blister. At this stage, the top layer of skin can repair itself.
- Stage 3: This stage is a deeper wound. The wound is open, extending to the fatty layer of the skin, though muscles and bone are not showing.
- Stage 4: This stage is the most severe. The wound extends down to the bone. The muscles and bone are prone to infection, which can be life-threatening.
Description Of The Intervention
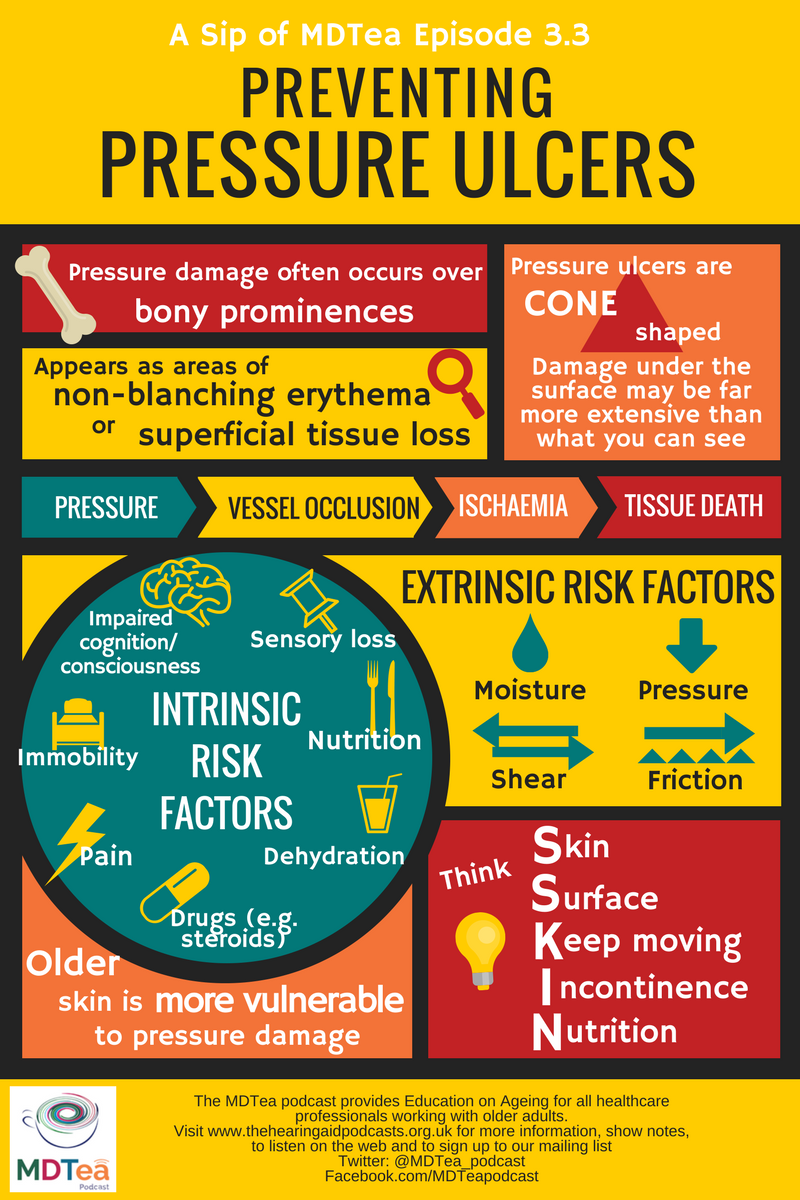
Use of pressure ulcer risk assessment tools or scales is a component of the assessment process to identify individuals at risk of developing a pressure ulcer . Risk assessments generally use checklists that alert practitioners to the most common risk factors that predispose individuals to pressure ulcer development. These checklists are often developed into risk assessment tools, for example the Norton Scale , the Waterlow tool and the Braden tool . It is argued that there is a lack of consensus regarding which variables are the most important indicators of risk . Therefore, it is not surprising that there are currently almost 40 risk assessment scales in use, most of which are based on the seminal work of Norton 1975, or have been designed in response to a review of the literature . It is clear, however, that the risk factors that predispose an individual to developing a pressure ulcer will vary among patients in different clinical settings , and it may not be possible to design one risk assessment tool that will meet the needs of all patients in all clinical settings.
Don’t Miss: What Not To Eat With Bleeding Ulcers
What Is A Pressure Injury
A pressure injury is an area of injured skin. A pressure injury happens when force is applied on the surface of the skin. This force can be a constant pressure on an area of skin or a dragging force between the skin and another surface. These injuries usually happen over bony parts of the body . A pressure injury can become life-threatening if it advances to a deep wound or becomes infected.
Comparison : Alternating Pressure Mattress Versus Standard Care
Characteristics of Included Studies
Two studies compared the Micropulse System alternating pressure mattress with standard care. The study characteristics are reported in Table 32. Both studies included patients having surgery for 2 or more hours. The follow-up study period was 7 days for both studies. Both studies used the National Pressure Ulcer Advisory Panel pressure ulcer classification system .
Recommended Reading: What Causes A Bleeding Ulcer In Stomach
How Often Is Repositioning Necessary
Even though it’s often recommended that people be repositioned every two hours, there’s no single recommendation that works for everyone. Some people can lie in the same position for quite a long time without getting ulcers, while others need to switch much more often. Research has not yet found out how often someone should change position to get the best preventive effect.
Unnecessarily moving someone too much for no good reason can also have disadvantages. For instance, repositioning every two hours at night may wake the person each time and keep them from getting a good nights sleep. Changing position can also be very painful for people who have wounds or joint conditions. Frequent repositioning is physically demanding for caregivers or family members too. It’s therefore important to observe how often someones position really needs to be shifted. It can then help to make a note every time they are repositioned.
Comparison : Alternating Pressure Mattress Or Overlay Versus Standard Foam Mattress
Characteristics of Included Studies
In the systematic review by Cullum et al., only the study by Andersen et al. was reported comparing an alternating pressure mattress with a standard foam mattress. We found 1 additional RCT to add to this body of evidence, that completed by Sanada et al. Therefore, 2 studies comprise the body of evidence comparing an alternating pressure mattress or overlay with a standard foam mattress. The study characteristics are reported in Table 19. All studies included patients admitted to an acute care setting. The follow-up study period was 10 days in the Andersen et al. study. Sanada et al. reported that follow-up was continued until a pressure ulcer developed. Both studies used an explicit but different pressure ulcer grading system .
You May Like: What Is The Medicine For Ulcer
What Are The Elements Of A Comprehensive Care Plan For Effective Prevention Or Pressure Injuries
Effective prevention of pressure injuries depends on a comprehensive care plan that includes strategies and practices aimed at reducing or eliminating the risk of these injuries. Elements of such a plan may include the following:
References
National Pressure Ulcer Advisory Panel announces a change in terminology from pressure ulcer to pressure injury and updates the stages of pressure injury. National Pressure Ulcer Advisory Panel. Available at . April 13, 2016 Accessed: June 10, 2018.
NPUAP pressure injury stages. National Pressure Injury Advisory Panel. Available at . April 2016 Accessed: March 26, 2020.
Woolsey RM, McGarry JD. The cause, prevention, and treatment of pressure sores. Neurol Clin. 1991 Aug. 9:797-808. .
Abrussezze RS. Early assessment and prevention of pressure ulcers. Lee BY, ed. Chronic Ulcers of the Skin. New York: McGraw-Hill 1985. 1-9.
Schweinberger MH, Roukis TS. Effectiveness of instituting a specific bed protocol in reducing complications associated with bed rest. J Foot Ankle Surg. 2010 Jul-Aug. 49:340-7. .
Pieper B, ed. Pressure Ulcers: Prevalence, Incidence, and Implications for the Future. Washington, DC: National Pressure Ulcer Advisory Panel 2013.
Treatment For Pressure Ulcers
The ulcers are treated with methods that promote wound healing and prevent further damage, such as
-Preventing deep or prolonged contact with a hard surface. This is done by using a unique cushion called an air body or air mattress. This helps maintain position, prevent shearing and improve circulation to the wound site.
-Removing or repositioning any objects in contact with the ulcer, such as clothing or sheets.
-Lifting extremities for bedridden patients. A unique tool called the McRoberts maneuver can raise a leg while the patient is lying on their back. This will help prevent pressure from being placed on that area and allow it to heal.
-Turning/repositioning bed-bound patients every two hours if possible. If not, reposition as often as possible for the patient.
-Prompt treatment of any skin breakdown with a topical or local wound-care product that will protect the skin from further damage.
Posted byJoy Joan E. De Castro, RN, MSN on Jan 31, 2017
For the patient with and/or at risk for pressure ulcers, in addition to assessing M2250 Pressure Ulcer care and prevention on OASIS C home health care forms, also include these MyHomecareBiz Best Practice assessment strategies:
Read Also: How To Get Rid Of Peptic Ulcer
Adapt A Holistic Approach
There are different measures available to prevent pressure ulcers. For example, whenever a patient enters a ward, a pressure ulcer risk assessment should be used, followed by a regular skin assessment to check for any signs of sores.
Also, nutrition plays a huge role in the patients overall health status influencing the probability of developing pressure injuries. It is important to assess the nutritional needs and adapt the diet accordingly and ensure adequate hydration.
What Are The Causes Of Pressure Injuries
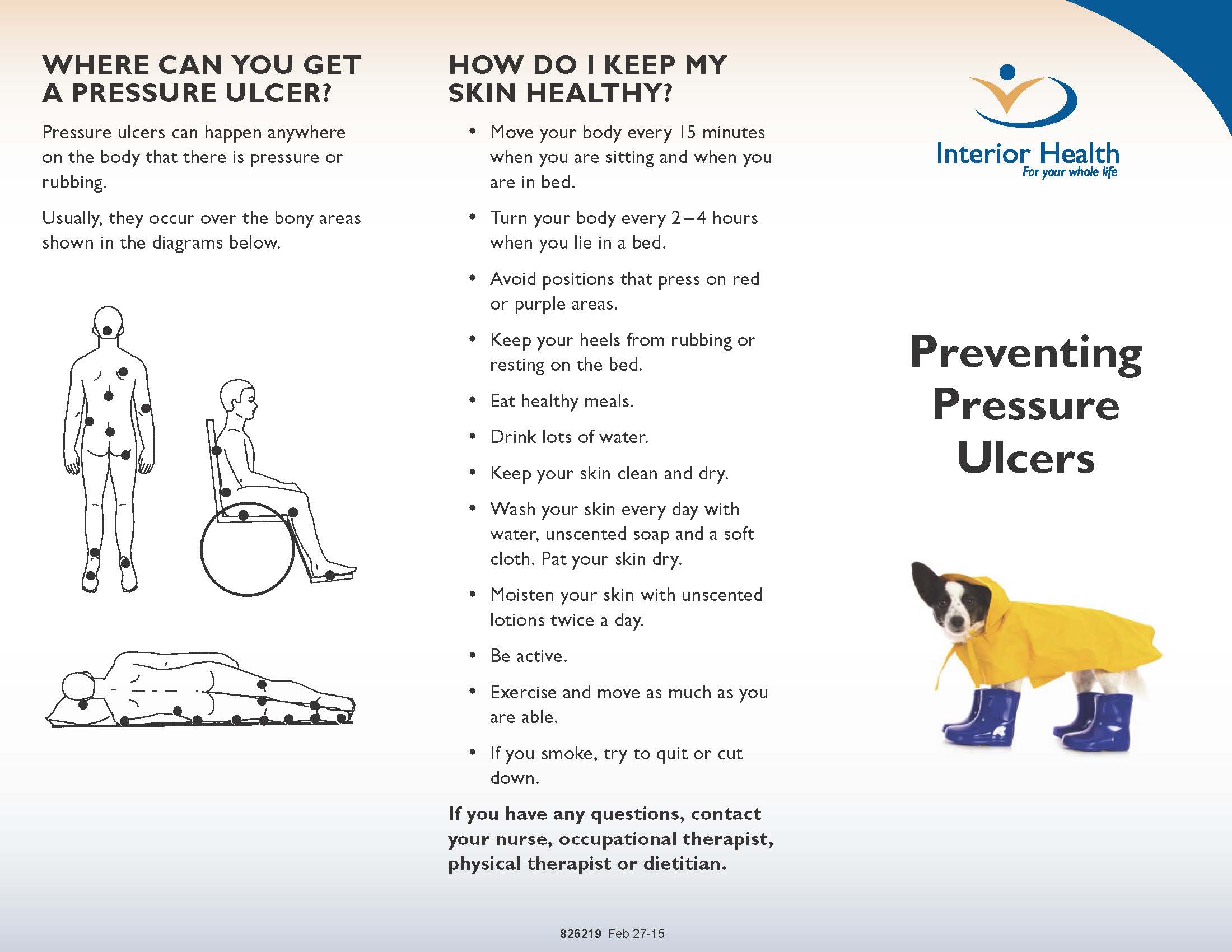
Pressure injuries are caused when a force is applied to the skin, causing damage to the tissue. Several types of force include:
- Pressure: Constant pressure on the skin results from remaining in the same position for a prolonged period of time.
- Shear: Shear damage or a dragging force can occur when the head of the bed is raised and the body slides down. The skin sticks to the sheets, but internal structures are damaged.
- Moisture: Fluids that remains on the skin can cause the skin to become overly wet, which increases the risk for pressure injury development.
Don’t Miss: Healing Ulcerative Colitis With Plant Based Diet
Which Interventions Are The Most Important
Pressure ulcers usually heal very slowly, and may come back. That’s why it’s so important to make sure they don’t develop in the first place. People who are confined to a wheelchair or have to stay in bed for a long time often say that they can feel parts of their body becoming sore. It’s important to pay attention to what they say, to quickly reduce pressure on their skin, and regularly change the position they sit or lie in.
Observing which parts of the body are most susceptible to pressure, as well as the positions that put the most pressure on them, can help you get an idea of what sort of relief might be helpful. For example, lying down puts much less pressure on your backside than sitting in a chair. If you use a wheelchair, you can find out what helps to reduce the pressure and then make that your routine.
It’s also important to try to move if possible even if you have to lie in bed or sit in a wheelchair. If you are able to sit up, leave the bed, or even walk a few steps with a bit of help, its a good idea to do that as often as possible.
How Should A Standardized Pressure Ulcer Risk Assessment Be Conducted
As discussed above, one purpose of comprehensive skin assessment is to identify visible changes in the skin that indicate increased risk for pressure ulcer development. However, factors other than skin changes must be assessed to identify patients at risk for pressure ulcers. This can best be accomplished through a standardized pressure ulcer risk assessment.
3.3.1 What is a standardized pressure ulcer risk assessment?
After a comprehensive skin examination, pressure ulcer risk assessment is the next step in pressure ulcer prevention. Pressure ulcer risk assessment is a standardized and ongoing process with the goal of identifying patients at risk for the development of a pressure ulcer so that plans for targeted preventive care to address the identified risk can be implemented. This process is multifaceted and includes many components, one of which is a validated risk assessment tool or scale.
Other risk factors not quantified in the assessment tools must be considered. Risk assessment does not identify who will develop a pressure ulcer. Instead, it determines which patients are more likely to develop a pressure ulcer, particularly if no special preventive interventions are introduced. In addition, risk assessment may be used to identify different levels of risk. More intensive interventions may be directed to patients at greater risk.
Action Steps
Ask yourself and your team:
3.3.2 Why is a pressure ulcer risk assessment necessary?
Action Steps
Ask yourself and your team:
Also Check: Is Omeprazole Good For Ulcers
Comparison : Alternating Pressure Mattress Versus Alternating Pressure Overlay
Characteristics of Included Studies
One study compared the use of an alternating pressure mattress with an alternating pressure overlay. The study characteristics are reported in Table 24. This comparison is not reported in the review by Cullum et al. The study by Nixon et al. included patients admitted to an acute care setting. The median follow-up time period was 9 days. An explicit pressure ulcer classification system was used to measure the outcome .
Implementation Of Pressure Ulcer Prevention Best Practice Recommendations In Acute Care: An Observational Study
Corresponding Author
Anna Lucia Barker
The University of Queensland, Brisbane, Australia, Centre of Research Excellence in Patient Safety, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
Correspondence to
AL Barker, PhD, Department of Epidemiology and Preventive Medicine, The Alfred Centre, 99 Commercial Road, Melbourne, Victoria 3004, Australia
Nicole Klopfer
Centre of Research Excellence in Patient Safety, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
Carolina Weller
Centre of Research Excellence in Patient Safety, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
Corresponding Author
Anna Lucia Barker
The University of Queensland, Brisbane, Australia, Centre of Research Excellence in Patient Safety, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
Correspondence to
AL Barker, PhD, Department of Epidemiology and Preventive Medicine, The Alfred Centre, 99 Commercial Road, Melbourne, Victoria 3004, Australia
Nicole Klopfer
Centre of Research Excellence in Patient Safety, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
Carolina Weller
Centre of Research Excellence in Patient Safety, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
Read Also: Hand Foot And Mouth Ulcers
What Other Kinds Of Aids Are Available
Another thing that can help prevent damage to the skin is sheepskin mattress covers. Some people find sheepskin unpleasant, though, because it can make your skin very warm after a while.
Pressure ulcers often occur on peoples heels. So heels are often elevated using pillows, or special heel protectors made out of animal skin or foam are used. But there is no proof that these actually prevent pressure ulcers. Some people find the heel protectors uncomfortable and choose not to wear them. There are also concerns that they could increase the risk of falling if people get up and walk around while wearing them.
There hasn’t been much research on aids such as special positioning cushions or special cushions for people to sit on either.
Grades Of Pressure Sores
If youve been bedridden for long enough, the areas of skin that are constantly in contact with the mattress or chair will start to discolour. This shows that the skin is in danger of ulcerating.
Pressure sores are graded to four levels, including:
- grade I skin discolouration, usually red, blue, purple or black
- grade II some skin loss or damage involving the top-most skin layers
- grade III necrosis or damage to the skin patch, limited to the skin layers
- grade IV necrosis or damage to the skin patch and underlying structures, such as tendon, joint or bone.
Also Check: Can Stomach Ulcers Cause Blood In Your Stool
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Causes And Prevention Of Pressure Sores
Pressure sores are wounds that develop when constant pressure or friction on one area of the body damages the skin. Constant pressure on an area of skin stops blood flowing normally, so the cells die and the skin breaks down.
Other names for pressure sores are bedsores, pressure ulcers and decubitus ulcers.
Don’t Miss: Natural Cure For Peptic Ulcer
Treatment For Pressure Sores
There are a variety of treatments available to manage pressure sores and promote healing, depending on the severity of the pressure sore. These include:
- regular position changes
- special mattresses and beds that reduce pressure
- being aware of the importance of maintaining healthy diet and nutrition
- dressings to keep the sore moist and the surrounding skin dry. There is no advantage of one type of dressing over another.
- saline gauze dressing may be used if ointments or other dressings are unavailable.
- light packing of any empty skin spaces with dressings to help prevent infection
- regular cleaning with appropriate solutions, depending on the stage of the sore
- there is no advantage of one particular type of antiseptic or antibiotic treatment over another
- specific drugs and chemicals applied to the area, if an infection persists
- surgery to remove the damaged tissue that involves thorough debridement of the wound, the removal of underlying or exposed bone, and filling the empty space
- operations to close the wound, using skin grafts if necessary
- continuing supportive lifestyle habits such as eating a healthy and nutritious diet, as suggested by the nutritional staff.