Cleaning And Dressing The Ulcer
The first step is to remove any debris or dead tissue from the ulcer and apply an appropriate dressing. This provides the best conditions for the ulcer to heal.
A simple, non-sticky dressing will be used to dress your ulcer. This usually needs to be changed once a week. Many people find they can manage cleaning and dressing their own ulcer under the supervision of a nurse.
What Causes Ankle Ulcers
Venous stasis ulcers are typically due to a condition called venous hypertension or chronic venous insufficiency. Your blood doesnt flow from your lower legs back to your heart as it should. This causes a buildup of pressure in your veins. The additional pressure can lead to an ulceration on your skin. These usually form on the inside of your legs, just above your ankle.
Its unknown exactly how this condition causes ulcers. Many doctors believe it also causes a decrease in blood flow to the capillaries of your legs. This produces a buildup of white blood cells. The accumulation of white blood cells restricts oxygen to your tissue. The lack of oxygen causes damage and forms the ulcer.
Another theory is that venous hypertension causes cells from elsewhere in the body to leak into your skin and influence cellular growth. This process interferes with the repair of damaged tissue.
You may have a higher risk of developing venous stasis ulcers if you have or had:
- previous leg swelling
- a history of inflammatory diseases
If you have a family history of ulcers, its possible youll develop them too. Smoking may also raise your risk of developing ankle ulcers because it interferes with the flow of oxygen through your bloodstream.
Symptoms Of Venous Leg Ulcers
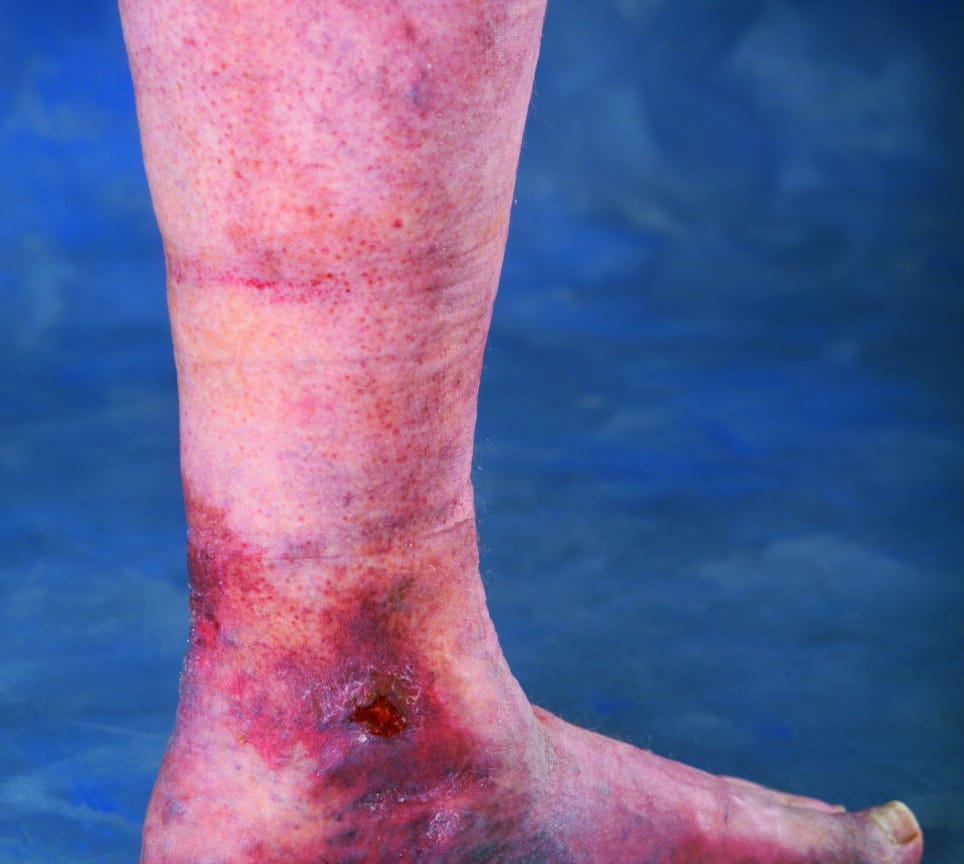
Venous leg ulcers are open, often painful, sores in the skin that take more than a month to heal. They usually develop on the inside of the leg, just above the ankle.
If you have a venous leg ulcer, you may also have:
- discolouration and darkening of the skin around the ulcer
- hardened skin around the ulcer, which may make your leg feel hard or even resemble the shape of an upside-down champagne bottle
- a heavy feeling in your legs
- aching or swelling in your legs
- red, flaky, scaly and itchy skin on your legs
- swollen and enlarged veins on your legs
- an unpleasant and foul-smelling discharge from the ulcer
Don’t Miss: What Are The Symptoms Of A Stomach Ulcer Uk
After The Ulcer Has Healed
Once you have had a venous leg ulcer, another ulcer could develop within months or years.
The most effective method of preventing this is to wear compression stockings at all times when you’re out of bed.
Your nurse will help you find a stocking that fits correctly and that you can manage yourself.
Various accessories are available to help you put them on and take them off.
Page last reviewed: 16 November 2022 Next review due: 16 November 2025
What Are My Treatment Options

Treatment will depend on many factors, including the reason for the condition and your health status and history. Other factors your doctor will consider are:
- Your specific symptoms.
- How severe your condition is.
- How well you can tolerate medications or procedures.
The most common treatment for venous insufficiency is prescription-wear compression stockings, she says. These special elastic stockings apply pressure at the ankle and lower leg. They help improve blood flow and can reduce leg swelling.
You also can improve blood flow by keeping your legs elevated whenever possible, which means keeping them uncrossed when you are seated and by exercising regularly.
If you need medication, the most commonly prescribed include:
- Diuretics. These medications draw extra fluid from your body through your kidneys.
- Anticoagulants. These medications thin the blood.
- Pentoxifylline . This medication helps improve blood flow.
Also Check: Liquid Diet For Ulcerative Colitis
Other Types Of Leg Ulcer
Other common types of leg ulcer include:
- arterial leg ulcers caused by poor blood circulation in the arteries
- diabetic leg ulcers caused by the high blood sugar associated with diabetes
- vasculitic leg ulcers associated with chronic inflammatory disorders such as rheumatoid arthritis and lupus
- traumatic leg ulcers caused by injury to the leg
- malignant leg ulcers caused by a tumour of the skin of the leg
Most ulcers caused by artery disease or diabetes occur on the foot rather than the leg.
Page last reviewed: 16 November 2022 Next review due: 16 November 2025
Getting A Specialist Vascular Referral
If you have venous hypertension, intervention to your veins from a vascular specialist might help with healing and stop your wound or sore from coming back. Sometimes varicose veins can be treated by laser therapy. If you have peripheral arterial disease, you may require further investigations and the vascular team will be able to assess the need to improve the blood supply to your leg or whether your ulcer can be managed in other ways such as reduced/modified compression. Ask your nurse or doctor for a referral to your local vascular team to talk about how their input might help you.
Also Check: Ulcerative Colitis Social Security Disability
Causes Of Venous Leg Ulcers
A venous leg ulcer is the most common type of leg ulcer. They are caused by diseases of the leg veins such as varicose veins or as a complication of a DVT .
Venous leg ulcers can develop after a minor injury. It can happen where persistently high pressure in the veins of the legs has damaged the skin.
How Are They Treated
Venous ulcers are usually treated with bandages or stockings that put pressure on your legs. Some of these are worn all of the time and need to be replaced by a doctor every few days. Others are worn only during the day, and you can put them on and take them off yourself. Your doctor may recommend gels or foams to put under the bandage to help the wound heal.
Sitting or lying down with your leg raised for 30 minutes, three or four times a day, can keep the swelling down. Your doctor may give you medicine to help the blood flow through your legs better.
Also Check: Best Supplement For Horses With Ulcers
Healthcare Advice For Leg Ulcers
There are some lifestyle changes you can make that will help boost healing:
- Maintain a healthy weight
- Eat a well-balanced diet that includes 5 portions of fruit and vegetables a day and protein rich foods such as eggs, fish, chicken or pulses
- Take light to moderate exercise such as cycling or walking for about thirty minutes at least three times a week
- Avoid standing or sitting for long periods of time
- Put your feet up elevate your legs above your heart.
- Every so often, move your feet around in circles, then up and down. This helps blood circulate and get back to your heart
Swelling In The Legs And Ankles
Venous leg ulcers are often accompanied by swelling of your feet and ankles , which is caused by fluid. This can be controlled by compression bandages.
Keeping your leg elevated whenever possible, ideally with your toes at the same level as your eyes, will also help ease swelling. You should put a suitcase, sofa cushion or foam wedge under the bottom of your mattress, to help keep your legs raised while you sleep.
You should also keep as active as possible and aim to continue with your normal activities. Regular exercise, such as a daily walk, will help reduce leg swelling. However, you should avoid standing or sitting still with your feet down. You should elevate your feet at least every hour.
Also Check: Evidence Based Practice Guidelines For Pressure Ulcer Prevention
Leg Ulcers In Older People: A Review Of Management
Adeyemi Adeyi, Sharon Muzerengi and Indrajit Gupta
Download PDF |
| Abstract
Leg ulcers are a common presentation in the elderly population associated with a negative impact in the quality of life. Several factors including venous and arterial insufficiency, immobility and obesity all contribute to an increased incidence in this age group. A thorough assessment including comprehensive history of ulcer development, examination of the ulcer site, size, shape, appearance and vascular assessment with Doppler ultrasound are all essential in deciding type of treatment. Various treatment modalities are available for the management of different types of leg ulcers although no clinical trials comparing the efficacy of one treatment over the other have been done. Some of them have not got strong evidence to show that they actually improve healing, still awaiting further research. |
Aetiology of ulcer
| Basal cell , squamaous cell carcinoma, melanoma | |
| Neuropathic | Common in diabetes, wet, deep, sharp borders on pressure points |
| Ulcer | SiteAppearanceSize-measureWound baseExudate levelSurrounding skin |
ANKLE CIRCUMFERENCE
| 1 wool padding1 high elastic bandage1 cohesive bandage | |
| Greater than 30cm | 1 wool padding1 light elastic bandage 1 high elastic bandage1 cohesive bandage |
- Patient fit for surgery
- Sufficient mobility to activate calf muscle pump
- Prepared to attend hospital for investigation and surgery
- Obesity controlled
- Superficial venous incompetence
References
What Does This Mean

This means that treating faulty veins under the skin in the superficial vein system by Endovenous Laser Ablation or Sclerotherapy speeds up the rate of healing of the commonest type of leg ulcer and doing so also reduces the risk of the ulcer coming back.
Lets cover what a leg ulcer is, what types of leg ulcer there are, what causes a venous leg ulcer and lets discuss this latest research.
Read Also: Alternative To Sulfasalazine For Ulcerative Colitis
What Is A Venous Leg Ulcer
A skin ulcer develops when an area of skin breaks down to reveal the underlying flesh. Venous leg ulcers are the most common type of skin ulcer. They mainly occur just above the ankle. They usually affect older people and are more common in women.
Venous leg ulcers are the most common type of leg ulcer, causing about 3 in 4 of all leg ulcers. They affect about 1 in 100 people in the UK at some stage in their lives. Venous leg ulcers become more common as you get older. Most are painless but some are painful. Without treatment, an ulcer may become larger and cause problems in the leg. Skin inflammation sometimes develops around a venous ulcer.
Non-venous skin ulcers are less common. For example, a skin ulcer may be caused by poor circulation due to narrowed arteries in the leg, problems with nerves that supply the skin, or other problems. The treatment for non-venous ulcers is different to that of venous ulcers.
The rest of this leaflet deals only with venous leg ulcers.
When Is Surgery Needed
Sometimes, more serious cases of venous insufficiency require surgery. Your doctor may suggest one of the following:
- Surgically repairing veins or valves.
- Removing the damaged vein.
- Minimally invasive endoscopic surgery .
- Laser surgery .
Surgical procedures include:
You May Like: What Can You Eat If You Have Ulcerative Colitis
Chronic Leg Ulcers: Epidemiology Aetiopathogenesis And Management
Shubhangi Vinayak Agale
1Department of Pathology, Grant Govt Medical College, Byculla, Mumbai 400008, India
Academic Editor:
Abstract
Chronic leg ulcer is defined as a defect in the skin below the level of knee persisting for more than six weeks and shows no tendency to heal after three or more months. Chronic ulceration of the lower legs is a relatively common condition amongst adults, one that causes pain and social distress. The condition affects 1% of the adult population and 3.6% of people older than 65 years. Leg ulcers are debilitating and greatly reduce patients quality of life. The common causes are venous disease, arterial disease, and neuropathy. Less common causes are metabolic disorders, hematological disorders, and infective diseases. As many factors lead to chronic lower leg ulceration, an interdisciplinary approach to the systematic assessment of the patient is required, in order to ascertain the pathogenesis, definitive diagnosis, and optimal treatment. A correct diagnosis is essential to avoid inappropriate treatment that may cause deterioration of the wound, delay wound healing, or harm the patient. The researchers are inventing newer modalities of treatments for patients with chronic leg ulceration, so that they can have better quality life and reduction in personal financial burden.
1. Introduction
4. Pathogenesis of Chronic Leg Ulcers
4.1. Venous Ulcers
4.3. Diabetic Foot Ulcer
What Does A Venous Leg Ulcer Look Like And What Causes Them
Venous leg ulcers are sores that develop between your knee and ankle, but they typically form inside the leg near or around the ankle. They are large, shallow ulcers with uneven edges that drain or weep a lot.
Youll likely see swelling in your leg, with red, itchy skin around the wound. You may also experience tightness in your calves, as well as aching, throbbing or a feeling of heaviness in your legs. Pooled and trapped blood often causes discolored splotches in the area.
The sores sometimes affect only the skin or they may sink deeper into the fat layer, muscle, tendon and bone, she says. Severe ulcers are more likely to become infected and take longer to heal.
Your veins carry blood back to your heart, and valves in the veins stop the blood from flowing backward. When your veins have trouble sending blood from your limbs to the heart, its known as venous insufficiency. In this condition, blood doesnt flow back properly to the heart, causing blood to pool in the veins in your legs.
Our veins are just like pipes, says Ehren. When theres persistently high blood pressure in the veins of the legs with a valve that doesnt work correctly, it causes damage to the skin, which eventually breaks down and forms an ulcer.
Other possible causes for venous leg ulcers include:
- Varicose veins.
Also Check: Can You Take Tylenol With Ulcerative Colitis
Also Check: Pressure Ulcer Care At Home
Preventing A Recurrence Of Venous Skin Ulcers
Venous leg ulcers commonly come back after they have healed. To prevent this, you should wear a support stocking during the daytime for at least five years after the ulcer has healed. This counteracts the raised pressure in the veins that causes venous leg ulcers. You should get a new stocking about every six months as the elastic tends to go after a while. Compression stockings can be prescribed or bought at pharmacies. They come in different sizes – your pharmacist will advise. Compression stockings for the prevention of venous leg ulcers are usually below knee in length rather than thigh length.
There are different strengths of compression stockings – class 1, 2 and 3. The higher the class the greater the compression. Ideally, wear class 3 stockings. However, some people find class 3 stockings too tight and uncomfortable but class 2 may be fine. It is still better to wear some sort of compression stocking than none at all.
Note: proper compression stockings used for medical purposes are different to the support stockings or tights sold in ordinary clothing shops.
A leg ulcer is much less likely to recur if you wear compression stockings regularly.
Sometimes surgery for varicose veins or other vein problems is advised after an ulcer has healed, in order to help prevent a recurrence.
Should Leg Ulcers Be Kept Dry
Low oxygen tension leads to high levels of oxygen at the capillaries and low levels of oxygen at the wound edges. This provides the ideal environment for wound healing because granulation and wound healing is stimulated. a wound, nurses should remember: If theres no blood supply keep it dry and seek expert advice.
Recommended Reading: Antibiotic For Mouth Ulcer Treatment
Treating An Infected Ulcer
An ulcer sometimes produces a large amount of discharge and becomes more painful. There may also be redness around the ulcer. However redness may be harder to see on black or brown skin.
These symptoms and feeling unwell are signs of infection. You should contact your GP or leg ulcer specialist as soon as possible.
If your ulcer becomes infected, it should be cleaned and dressed as usual.
You should also elevate your leg most of the time. You’ll be prescribed a 7-day course of antibiotics.
The aim of antibiotic treatment is to clear the infection. But antibiotics do not heal ulcers and should only be used in short courses to treat infected ulcers.
What To Expect After Treatment With Cvm
At CVM, we’re ready to help diagnose and treat your leg ulcers at our select wound care locations:
Our expert team will carefully consider all potential chronic pelvic pain causes, with a special emphasis of diagnosing any potential vascular disorders.
We provide complete chronic pelvic treatment for pain. Aside from implementing innovative techniques to treat your pain, including treatments for vascular issues, we’re committed to listening to your concerns and treating your pain seriously. Many of our patients go on to have significant improvement or resolution of their symptoms.
Recommended Reading: What Happens When You Have A Bleeding Ulcer
How Venous Leg Ulcers Are Treated
Most venous leg ulcers heal within 6 months if they’re treated by a healthcare professional trained in compression therapy for leg ulcers.
But some ulcers may take longer to heal, and a very small number never heal.
Treatment usually involves:
- cleaning and dressing the wound
- using compression, such as bandages or stockings, to improve the flow of blood in the legs
Antibiotics may also be used if the ulcer becomes infected, but they do not help ulcers heal.
But unless the underlying cause of the ulcer is addressed, there’s a high risk of a venous leg ulcer coming back after treatment.
Underlying causes could include immobility, obesity, previous DVT or varicose veins.