What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
Skin And Wound Care Practices Today
You will hear clinicians who would never dream of practicing medicine and nursing exactly the same way they did 30 years ago falling back on what they perceive as acceptable care for patients at risk for or presenting with a pressure ulcer. I STILL hear people promoting liquid antacids, povidone iodine, sugar, off the grocery shelf honeythe list seems endless. Yet they will swear their patient healed. My assertion is that some patients healed despite the awful things someone put on their wound. We need to apply evidenced-based practice in skin and wound care the same careful way we apply those principles to other aspects of health care.
About The AuthorPaula Erwin-Toth has over 30 years of experience in wound, ostomy and continence care. She is a well-known author, lecturer and patient advocate who is dedicated to improving the care of people with wounds, ostomies and incontinence in the US and abroad.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, Kestrel Health Information, Inc., its affiliates, or subsidiary companies.
Acp Clinical Practice Guidelines
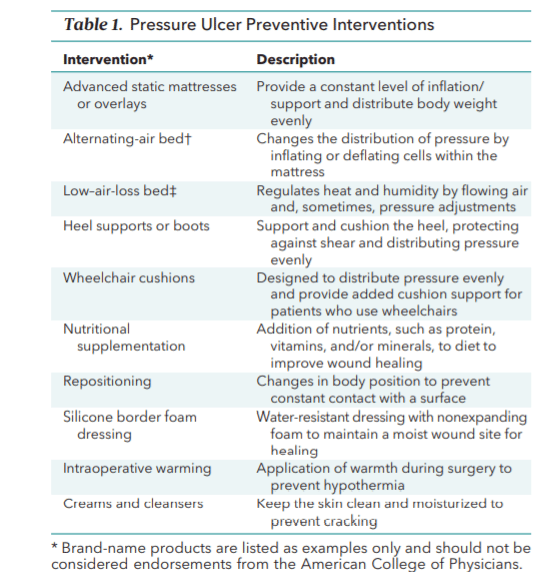
The 2015 American College of Physicians clinical practice guidelines for risk assessment, prevention, and treatment of pressure ulcers included the following recommendations and statements :
References
Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System. J Wound Ostomy Continence Nurs. 2016 Nov/Dec. 43 :585-597. . .
NPIAP pressure injury stages. National Pressure Injury Advisory Panel. Available at . Accessed: April 29, 2022.
Woolsey RM, McGarry JD. The cause, prevention, and treatment of pressure sores. Neurol Clin. 1991 Aug. 9:797-808. .
Abrussezze RS. Early assessment and prevention of pressure ulcers. Lee BY, ed. Chronic Ulcers of the Skin. New York: McGraw-Hill 1985. 1-9.
Schweinberger MH, Roukis TS. Effectiveness of instituting a specific bed protocol in reducing complications associated with bed rest. J Foot Ankle Surg. 2010 Jul-Aug. 49:340-7. .
Zhao G, Hiltabidel E, Liu Y, Chen L, Liao Y. A cross-sectional descriptive study of pressure ulcer prevalence in a teaching hospital in China. Ostomy Wound Manage. 2010 Feb 1. 56:38-42. .
Pham B, Stern A, Chen W, Sander B, John-Baptiste A, Thein HH, et al. Preventing pressure ulcers in long-term care: a cost-effectiveness analysis. Arch Intern Med. 2011 Nov 14. 171:1839-47. .
Don’t Miss: To Prevent Pressure Ulcers You Must
Pressure Injury Prevention & Management
Implementing an evidence-based best practice system for pressure injury prevention and management can reduce the potential for pressure injury development and promote healing of existing pressure injuries.
Each person should be assessed for pressure injury risk factors on admission and receive an in-depth assessment of any existing pressure injuries. The assessment process drives the development of person-centered goals and interventions to prevent or heal pressure injuries.
The care plan should reflect the persons preferences, values and needs and identify the interventions necessary to meet his/her goals for treatment. The care plan should also include guidelines for reassessment to evaluate the effectiveness of the care provided and to prompt changes in treatment as needed. The use of any particular intervention should be based on the strength of the evidence provided by existing clinical trials or literature reviews.
Evaluation and monitoring outcomes are vital components of any program for managing pressure injury risk and treating existing pressure injuries. An effective system includes reassessment of the persons risk for developing a pressure injury. The frequency of reassessment will depend on a variety of factors, with more frequent assessments for people with existing pressure injuries, those who are at high risk for developing pressure injuries, or those who have experienced a significant change of condition.
Turn Everyone And Move Study
The Turn Everyone And Move study13 was a 12-month paired facility 2-arm randomized intervention trial that tested the effectiveness of musical cues reminding LTC nursing and ancillary staff to help residents to move or reposition all residents, regardless of identified risk level, every 2 hours in 10 US LTC facilities. Staff and visiting family members received education on both PrU prevention and the intervention. Musical selections based on facility preferences were played over the facility public address system every 2 hours for the 12-hour daytime period. Intervention facility residents were 45% less likely than comparison facility residents to develop a new PrU. The researchers concluded that a broad approach involving customized musical cues that prompt multidisciplinary staff teams to encourage or enable all residents to move holds promise for reducing facility-acquired PrUs in LTC settings.13,26
Don’t Miss: How Can You Get Ulcers In Your Stomach
About The American College Of Physicians
The American College of Physicians is the largest medical specialty organization and the second-largest physician group in the United States. ACP members include 141,000 internal medicine physicians , related subspecialists, and medical students. Internal medicine physicians are specialists who apply scientific knowledge and clinical expertise to the diagnosis, treatment, and compassionate care of adults across the spectrum from health to complex illness. Follow ACP on and .
Infrastructure To Support Change
Sarasota Memorial Healthcare System, a magnet recognized not-for-profit organization, is committed to delivering safe, high-quality care that results in desired outcomes and is consistent with current professional knowledge . The organizational culture is reflected in the mission statement as well as the organizations participation with several agencies including The Joint Commission, the Agency for Healthcare Research and Quality Patient Safety Indicators, the American Nurses Credentialing Center Magnet Program , and many other health care accrediting agencies. Interdisciplinary collaboration is encouraged as evidenced by interdiscipli-nary meetings that focus on identifying the need for change and implementing evidence-based practice . Change that results in improved patient outcomes is encouraged by the executive team, risk management, nurse educators, several practice councils, and unit managers. Initiation of and participation in change is recognized by nurse of clinical excellence awards. At SMH, proposed changes are commonly presented to unit practice councils throughout the organization. Council members vote on the proposed change, and if the majority of the UPC members and council chair agree upon the proposal, the specified change in practice is implemented systematically.
Recommended Reading: Chicken Recipes For Ulcerative Colitis
Assessment And Management Of Pressure Injuries For The Interprofessional Team Third Edition
Purchase hardcopyAbout this Guideline
The third edition Assessment and Management of Pressure Injuries for Interprofessional Teams guideline provides evidence-based practice, education and policy recommendations for interprofesssional teams across all care settings who are assessing and providing care to people with existing pressure injuries in people 18 years of age and above.
This guideline provides best practice recommendations in three main areas:
- Practice recommendations are directed primarily to the front-line interprofessional teams who provide care for people with existing pressure injuries across all practice settings.
- Education recommendations are directed to those responsible for interprofessional team and staff education, such as educators, quality improvement teams, managers, administrators, and academic institutions.
- System, organization, and policy recommendations apply to a variety of audiences, depending on the recommendation. Audiences include managers, administrators, policy-makers, health-care professional regulatory bodies, and government bodies.
Related File
Assignment: Pressure Ulcer In Icu In Uk
1- Critique different types of evidence 2- Analyse what constitutes Best Evidence for practice in the UK3- Critically reflect on the BENEFITS and LIMITATIONS of evidence based practice within nursing practice. Using Randomised Controlled Trial Student will critique a qualitative and quantitative research paper and explore how research and EBP apply to nursing practice.Harvard Reference, CINAHL, NICE,
Introduction
Recommended Reading: Can Ulcerative Colitis Cause Blood In Urine
The Purpose Of The Guideline
The purpose of the guideline is to implement evidence-based guidelines for caregivers of palliative care patients on pressure ulcer prevention. This guideline aims to improve the knowledge and practice of caregivers and enables them to take measures to prevent pressure ulcer development among palliative care patients, thereby improving the quality of life of palliative care patients.
How Should A Standardized Pressure Ulcer Risk Assessment Be Conducted
As discussed above, one purpose of comprehensive skin assessment is to identify visible changes in the skin that indicate increased risk for pressure ulcer development. However, factors other than skin changes must be assessed to identify patients at risk for pressure ulcers. This can best be accomplished through a standardized pressure ulcer risk assessment.
3.3.1 What is a standardized pressure ulcer risk assessment?
After a comprehensive skin examination, pressure ulcer risk assessment is the next step in pressure ulcer prevention. Pressure ulcer risk assessment is a standardized and ongoing process with the goal of identifying patients at risk for the development of a pressure ulcer so that plans for targeted preventive care to address the identified risk can be implemented. This process is multifaceted and includes many components, one of which is a validated risk assessment tool or scale.
Other risk factors not quantified in the assessment tools must be considered. Risk assessment does not identify who will develop a pressure ulcer. Instead, it determines which patients are more likely to develop a pressure ulcer, particularly if no special preventive interventions are introduced. In addition, risk assessment may be used to identify different levels of risk. More intensive interventions may be directed to patients at greater risk.
Action Steps
Ask yourself and your team:
3.3.2 Why is a pressure ulcer risk assessment necessary?
Action Steps
Ask yourself and your team:
Also Check: What Foods To Eat When You Have A Stomach Ulcer
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Skin integrity .
Tools
Detailed instructions for assessing each of these areas are found in Tools and Resources .
Action Steps
American College Of Physicians Releases New Guidelines Forpreventing And Treating Bedsores
Evidence showed that nutritional supplementation with protein or amino acids reduced wound size
Read Prevention Guideline | Read Prevention Summary for Patients | Read Treatment Guideline | Read Treatment Summary for Patients | Read Editorial
Philadelphia, March 3, 2015 — The American College of Physicians today published two evidence-based clinical practice guidelines in Annals of Internal Medicine for the prevention and treatment of bedsores, also called pressure ulcers. Bedsores commonly occur in people with limited mobility, such as those in hospitals or long-term care settings.
Up to $11 billion is spent annually in the United States to treat bedsores and a growing industry has developed to market various products for pressure ulcer prevention, said Dr. David Fleming, president, ACP. ACP’s evidence-based recommendations can help physicians provide quality care to patients while avoiding wasteful practices.
Don’t Miss: What To Do For Ulcer Pain
Learn The Risk Factors And Tailor Prevention To Device Type
Takeaways:
- Medical devicerelated pressure injuries are a common but preventable patient care issue with simple interventions.
- Prevention guidelines and evidence-based practices can help reduce MDRPIs.
Editors note: The author has provided the attached PDF file of a clinical tips card for preventing medical device related pressure injuries. The card is 2 inches by 7 inches the spot at the top indicates where a hole could be punched to put a laminated version of the card on a lanyard. It could also be carried in the pocket and posted in the unit.
THE Joint Commissions Quick Safety issue on managing medical devicerelated pressure injuries points out that nearly all hospital patients require at least one medical device for care and treatment, putting them at risk for injury. The National Pressure Ulcer Advisory Panel defines MDRPI as localized damage to the skin and/or underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear.
Nurses can take the lead in preventing MDRPIs by understanding risk factors, tailoring prevention to the device type, collaborating with other team members to ensure continuity of care, and monitoring for change.
The Burden Of Pressure Ulcers
The burden of pressure ulcers on those living with them, on those engaged in efforts to prevent and treat them, and on healthcare resources, is enormous. Pressure ulcer prevention and reduction is a high priority for the NHS . Commissioning for Quality and Innovation suggests that, based on the NHS SafetyRefers to serious adverse effects, such as those that threaten life, require or prolong hospitalization, result in permanent disability, or cause birth defects. Thermometer Pilot, pressure ulcer incidenceThe number of new occurrences of something in a population over a particular period of time, e.g. the number of cases of a disease in a country over one year. can be halved in one year, and the tools they cite for achieving this include high quality evidence . The NICE guideline on Pressure ulcers: prevention and management draws on the best available evidence but in relation to many core elements of care this is not high quality. Decisions about care need to be informed by reliable evidence of effectivenessThe ability of an intervention to produce a desired effect, such as reduce symptoms. and safety, but primary research is lagging behind.
Read Also: How Ulcerative Colitis Is Diagnosed
Pressure Ulcers Are Common
A prevalenceThe proportion of a population who have a particular condition or characteristic. For example, the percentage of people in a city with a particular disease, or who smoke. survey conducted in the city of Leeds as part of an NIHR-funded five year programme of work, the Wounds Research for Patient Benefit , demonstrated that complex wounds are common, with an estimated point prevalence of 1.47 per 1000 people , and that pressure ulcers were the most frequent type of complex wound .
The survey also found that most people were receiving wound care from community nurses, with a median of two visits per week, lasting just under half an hour. The standard of care was generally high almost 95% of all pressure ulcers had a documented European Pressure Ulcer Advisory Panel ulcer severity classification in line with NICE guidelines and 73% of people with pressure ulcers had a pressure-relieving mattress.
Clearly nurses are working hard on pressure ulcer management. The cornerstones of care revolve around low technology interventions such as repositioning essentially nothing new. But is, what is considered to be best practice, actually evidence-based practice and does this matter?
Understanding The Extent Of The Local Problem
A 12 hour prevalence survey was done on all inpatient units to establish risk of pressure sore development and the proportion of patients with skin breakdown. Volunteer clinical nurses collected the data after instruction about evidence-based practice, clinical practice guidelines, and how to assess prevalence. After a 2 week follow up period, all new occurrences of pressure ulcers were documented and the accuracy of a risk assessment scale was evaluated.
Recommended Reading: Is Ulcerative Colitis Worse Than Crohn Disease
Don’t Miss: What Are The Signs Of An Ulcerative Colitis Flare Up
Use Of Cueing Innovations To Ensure Consistent Care Delivery
Three recent PrU prevention interventions in LTC13,14,19 have addressed the issue of consistent care delivery in LTC by using innovative methods of cueing to ensure timely and consistent turning/repositioning of residents. Cueing supports storage of the regularly scheduled task of repositioning in staff memory that is required by the protocol and reinforces timely recall and performance of this task, even in the presence of distracting intrusive events. The result is improved consistency in meeting standards of care and reduction in undesired variation in the occurrence and timing of care delivery. The 3 interventions are: On-Time Quality Improvement for Long-Term Care,19â21 the Turning for Ulcer ReductioN study,14 and the Turn Everyone And Move study.13 The unique cueing innovations featured in each PrU prevention intervention were developed in collaboration with the LTC facility communities responsible for its implementation.13,14,19 Descriptions of cueing components associated with each intervention, staff responses to each cue, focus of care facilitation, and the frequency of cue use are provided in Supplemental Digital Content, Table 1.