Speak With Your Doctor
Without treatment, people with UC tend to relapse.
For many people with mild or moderate symptoms, things improve somewhat after diagnosis. This is thanks to medication, along with identifying and avoiding triggers.
More aggressive cases are less common, and only a small number of severe cases will require hospitalization.
Repeated flare-ups can indicate problems with your current treatment, so speak with your doctor and discuss adjusting your medication.
Several classes of medication now exist that can help you get into and stay in remission. Your doctor may need to add another type or increase your dosage.
The only way to prevent UC flare-ups is to have surgery. The most common type of UC surgery is the proctocolectomy, which involves the removal of the rectum and colon.
Candidates for UC surgery include people who:
- have sudden or severe disease
- have a perforated colon
- are at risk for colorectal cancer
- are unable to tolerate their UC medications due to side effects
- have stopped responding to their UC medications
In addition to knowing how to manage flare-ups, its also helpful to recognize factors that can trigger your flare-ups.
Tags: IBD
Please note:This article outlines 11 tips to help you prevent an ulcerative colitis flare, and is based on one patients experience. Nothing in this article is meant to replace any advice you have received from your doctor.This article was contributed by Ms. Wanni Z. Below is her story.
Mild Hypoxic Stress Was More Frequent In Patients With Flare
Mild hypoxic stress was defined as aircraft travel and/or journeys to regions lying at an altitude of > 2000 m above the sea level. Details regarding the occurrence of mild hypoxic stress in the two groups during the observation period between September 1st, 2010 and August 31st, 2011 are presented in . Twenty one patients in the group experiencing flare-up episodes traveled by aircraft and/or journeyed to regions lying at an altitude of > 2000 m above the sea level within 4 weeks of occurrence of the flare-up when compared to 8 patients in the IBD group that were in clinical remission . These findings are illustrated in . When a comparison between subgroups of IBD patients was made, 8/21 CD patients who experienced flare-up episode had travelled by airplane or to high altitude regions when compared to 2/22 CD patients in clinical remission . In UC patients experiencing flare-up episodes, a trend for more frequent aircraft travel and journeys to higher regions was observed .
A detailed analysis of the frequency, duration, and destination of the flights is provided in . IBD patients experiencing flare-up episodes more frequently travelled by aircraft when compared to IBD patients in remission . On average, IBD patients experiencing flare-up episodes traveled 6.2 ± 4.2 h when compared to 4 ± 4.1 h in the IBD group in remission .
Foods To Eat With Ulcerative Colitis
My long-term nutrition goal for my clients with ulcerative colitis is always to move towards an anti-inflammatory diet where they eat as many whole plant foods as possible. It is thought that a more Mediterranean or anti-inflammatory diet pattern contributes to an healthier community of gut bacteria, a stronger gut barrier and a better immune balance between tolerance and inflammation. In one clinical trial, a plant-based diet improved relapse rates in ulcerative colitis. Other lab research suggests that a Mediterranean-style diet decreases risk of colitis. However, because of the nature of inflammation and irritation, it can often take very slow and sustained change over time to increase intake of plant-based foods comfortably.
- Fruits and Vegetables
Fruits and vegetables have been associated with a decreased risk of ulcerative colitis. They are high in anti-inflammatory phytochemicals and fibre, which is critical for production of short chain fatty acids by our gut bacteria that help to ease inflammation and support gut barrier function.
- Omega 3 rich seeds
We all need omega 3 rich foods in our daily diet ulcerative colitis is no exception. Data suggests that increased intake of omega 3 rich foods decreases risk of ulcerative colitis but clinical trials on fish oils have not offered conclusive benefits to disease outcomes.
- Calcium- and magnesium-rich foods
Recommended Reading: Stomach Ulcer Treatment In Homeopathy
How Much Vitamin D Should I Take For Crohns
Replenishing low vitamin D helps heal active mucosal inflammation in the intestines, and oral supplementation is well-absorbed and tolerated. This was confirmed by a study published in June 2015 in the United European Gastroenterology Journal, which found a dose of 2000 international units per day to be
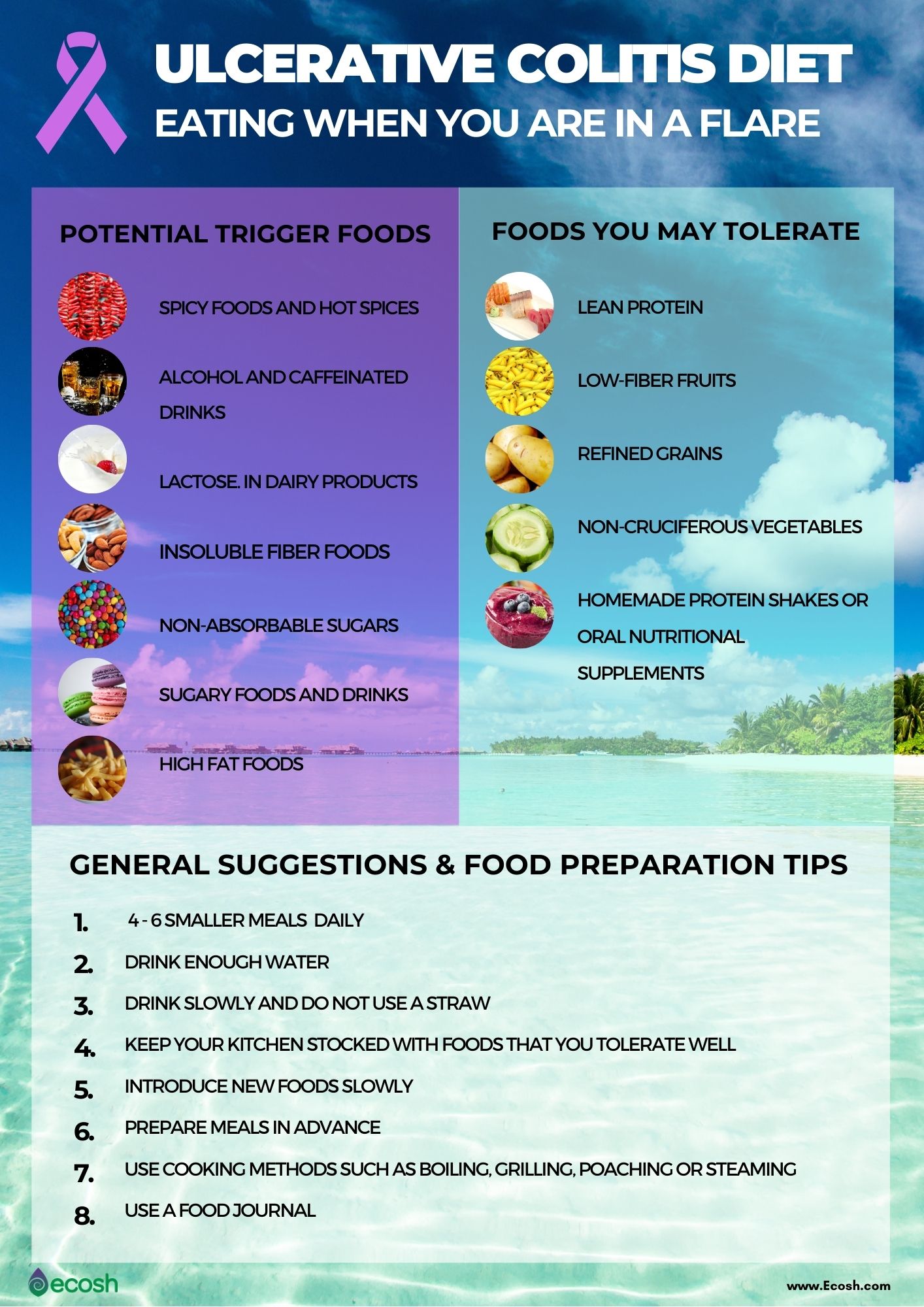
Diet Tips During A Flare
A modified diet may help you manage and reduce your UC symptoms. Depending on the person, specific foods may trigger flare-ups or worsen symptoms. As a result, its important to identify and limit these foods.
Your doctor and a dietitian can work with you to find a diet that best manages your symptoms while providing the nutrition you need.
Don’t Miss: What Causes Stomach Ulcers In Humans
Can I Drink Alcohol With An Ulcerative Colitis Flare
Alcohol has a significant impact on the gut microbiome, leading to changes that can promote inflammation. While a small amount may be well tolerated, for some, alcohol even when consumed in small amounts, can lead to an increase in symptoms such as diarrhoea and pain.
The changes in the gut microbiome are noted in Ulcerative colitis patients who consume alcohol. Specifically, an increased number of bacteria that promote inflammation in the gut. This may then lead to increased permeability along the gut lining and the overactivation of the immune response which then leads to the tissue damage seen in this condition.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Don’t Miss: Why Do I Keep Getting Mouth Ulcers
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
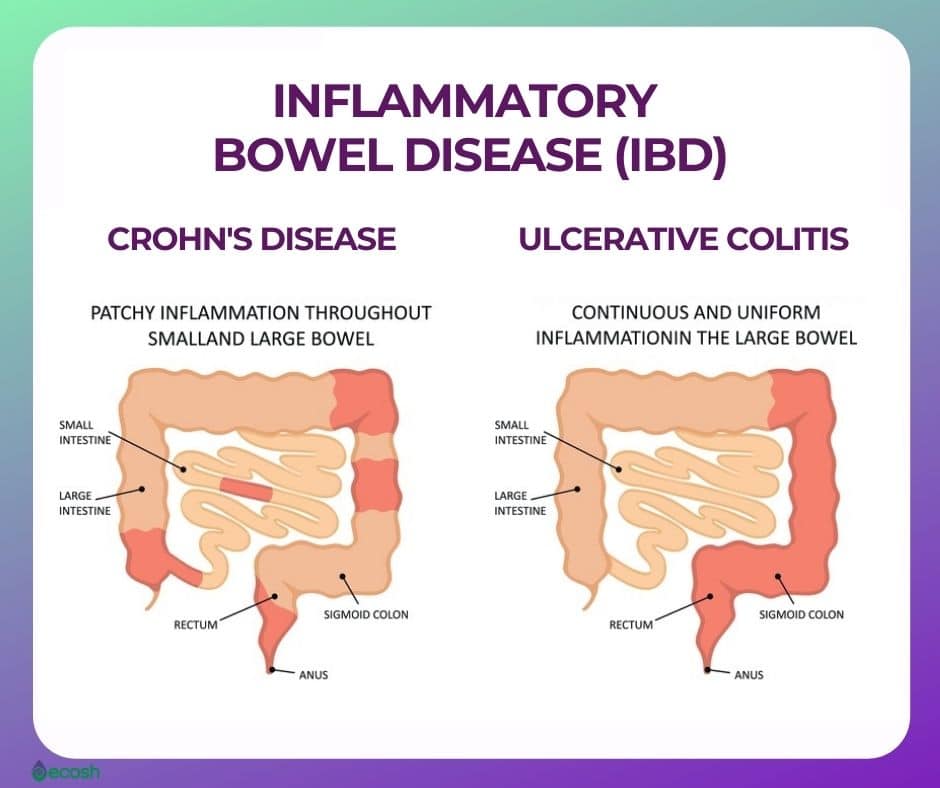
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Gut Bacteria And Ulcerative Colitis
Imbalances in the gut microbiome have been linked with the onset of IBD. This is likely due to an inappropriate immune response to the gut bacteria leading to inflammation.
Its also been noted that in those with IBD, there are imbalances in the gut bacteria. This bacterial imbalance is referred to as dysbiosis and is seen as a reduction in the diversity of the gut bacteria. This also results in a reduced number of specific beneficial bacteria that have anti-inflammatory properties.
Don’t Miss: Ulcer Signs Symptoms And Treatment
What Meals Are Protected For Folks With Ulcerative Colitis
Foods which can be normally tolerated properly by folks with UC embody:
- Breads, noodles and pastas produced from refined white flour
- Boiled white rice
- Crackers and cereals produced from white flour
- Fruits with out peels and seeds
- Cooked greens with out skins and seeds
- Pureed greens and vegetable soups
- Soft, tender meats with out pores and skin
You May Like: Causes Of Bleeding Ulcers In Stomach
Symptoms Of Ulcerative Colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience fatigue , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is. For some people, the condition has a significant impact on their everyday lives.
Recommended Reading: How To Tell Stomach Ulcer
Recommended Reading: Is Ulcerative Colitis Worse Than Crohn Disease
What Makes It Worse
The reasons why aren’t totally clear. Doctors don’t know why it affects only a small section in one person, but spreads through the entire colon in another. But certain triggers sometimes play a role. These include:
Food. It’s different for everyone, but certain foods can irritate your symptoms. For example:
- Caffeine can make severe diarrhea worse
- Dairy may lead to more diarrhea, gas, and pain
- Fizzy drinks can be a problem if you have gas
- Greasy and fried foods often lead to gas and diarrhea
- High-fiber foods, such as fresh fruits and veggies, whole grains, corn, nuts, and seeds, can be hard on you
- Spicy foods can be tough to handle
Stress. It can trigger flare-ups and make your symptoms much harder to deal with. It’s especially challenging because just having ulcerative colitis can bring on more of it.
Skipping meds. Even when you’re in remission, it’s very important to take your meds. In the best case, they prevent flare-ups. And even if not, they can help keep things under control.
Follow these 5 tips to help control your ulcerative colitis flare-ups.
How Long Do Flares Last
Flares occur at different times and may last for days or weeks. They can happen anywhere from weeks to years apart, depending on the person and the effectiveness of treatment.
Your doctor will work with you to treat your flare and help return your UC to a more manageable state.
The Crohns & Colitis Foundation recommends waiting to become pregnant until UC has been in remission for at least 3 months.
If you conceive during a flare-up, you may have more symptoms during pregnancy.
Youre likely to have a healthy pregnancy if you have UC, but youll still have a higher chance of complications than someone without the condition. Particularly if your UC is active, you may have a greater risk for:
In general, UC medications can be taken during pregnancy.
Talk with your doctor about any possible changes to your medications while pregnant.
Ideally, having a conversation with your doctor prior to getting pregnant can allow them to prepare a UC treatment plan in advance that can be revised, if and as needed, during your pregnancy.
You May Like: Coconut Milk Good For Ulcerative Colitis
Ulcerative Colitis Treatment Medications
Treatments for ulcerative colitis includes both medications and surgery however, there is no medication that can cure ulcerative colitis. Medicationsthat treat ulcerative colitis are
- anti-inflammatory agents, for example, 5-ASA compounds like sulfasalazine , and olsalazine , and topical and systemic corticosteroids), and
- immunomodulators, for example, 6-mercaptopurine , azathioprine , methotrexate , cyclosporine .
Treatment of ulcerative colitis with medications is similar, though not always identical, to treatment of Crohns disease.
Also Check: Pepto Bismol And Ulcerative Colitis
Assessment Of Sleep Duration And Shift Work
Participants in NHS I were asked about total hours of actual sleep in 24-hour period. The response categories were < 5, 6, 7, 8, 9, 10, or 11 hours or more. Participants in NHS II were asked the same question in 2001 with similar response categories. Self-reported sleep duration has been validated previously in these cohorts. In 2002, among women who completed the question on sleep duration in 2000, 480 were mailed a supplemental questionnaire and invited to keep a sleep diary for 1 week. There was strong correlation between self-reported sleep duration and the sleep diary . Furthermore, there was good reproducibility for sleep duration reported in 2000 and 2002 within a one hour deviation 50. Self-reported sleep duration also demonstrates moderate to strong correlation with sleep duration measured by polysomnography or actigraphy51–53. Women who completed the sleep duration question were similar in age, body mass index, physical activity, alcohol consumption, and dietary factors to those who did not complete this question. Sleep duration was classified as 6 hours, 7-8 hours, and 9 hours consistent with prior analyses26,30,50.
Recommended Reading: H Pylori And Stomach Ulcers
Shift Work And Risk Of Uc And Cd
We explored the association between duration of rotating night shift work and risk of UC or CD . Compared to women who reported no shift work, women with 1-5 years and 6 years of shift work reported similar risk of UC . We also observed no association between number of years of night shift work and incidence of CD.
The Big Problem With The Current Conventional Treatment For Ulcerative Colitis
Current conventional treatment does not focus on any of the causes and only targets symptoms.
Doctors do not believe that chronic stress and emotional imbalances could be a factor in triggering the disease. They also do not believe diet or lifestyle choices could be a cause. This is changing slowly however as more research proves otherwise. Most of the current medications for ulcerative colitis lead to negative side effects, especially the use of steroids long term. Surgery still does not solve the problem because if the causes are still present, disease will manifest in other areas of the body.
You May Like: How Do Stomach Ulcers Heal
You May Like: Ulcerative Colitis And Blood In Urine
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
Natural Ways To Heal Ulcerative Colitis
Herbs are plants valued for their specific strengthening/ tonifying properties.
Use a combination of the following herbs for ulcerative colitis in capsule, powder or tincture for maximum benefit, and adjust as your condition improves. Therapeutic dose is equal to one capsule of each herb 3 times a day or 1 liquid dropper full of an herbal tincture 3 times a day.
Calendula herb for ulcerative colitis is bacteriostatic and tissue healing.
Licorice soothes and heals the mucus membranes and acts like a steroid to calm the tissues without side effects.
herb for ulcerative colitis is tissue soothing, cooling and healing.
Plantain is a tissue wound healer and also treats leaky gut syndrome.
White oak bark is an astringent to pull the tissues tight and promotes healing.
Wild yam is anti-inflammatory and promotes digestion, releases gas and is anti-spasmodic.
Don’t Miss: What To Take For Ulcerative Colitis
Continuous Signs And Symptoms
Ulcerative colitis can cause signs and symptoms such as diarrhea, blood in the stool, nausea, fatigue, and abdominal pain. One of the goals of treatment is to stay on top of the inflammation that may contribute to these symptoms.
The symptoms of ulcerative colitis can lower a persons quality of life significantly, as well as affect personal relationships and the ability to have a rewarding and successful career. While it does take time and effort to develop a treatment plan, the result can be the cessation of the symptoms and an improvement in quality of life.
Understanding Ulcerative Colitis Flare
A flare-up is the reappearance of disease symptoms. And for people living with ulcerative colitis , an inflammatory bowel disease , flare-ups can be unpredictable, lasting hours, days, or weeks.
- Frequent and/or urgent bowel movements
- Lack of appetite
- Joint and body aches
Because these symptoms may also be caused by something other than UC, it can sometimes be difficult to tell whether you’re experiencing a flare-up. Below, we look at factors that might affect a UC flare-up, and what can help if you are experiencing a UC flare-up.
You May Like: Ulcerative Colitis Left Side Pain