Colitis Patients Diagnosed Later In Life Tend To Have Better Disease Outcomes
- Date:
- Washington University School of Medicine
- Summary:
- Adults diagnosed with ulcerative colitis after age 50 are more likely to achieve remission from their symptoms than patients diagnosed at younger ages, even when those patients receive similar treatments, according to new research. The study is the first to look at patients whose colitis was treated with modern medications. Nearly 1 million US adults have ulcerative colitis.
Adults diagnosed with ulcerative colitis after age 50 are more likely to achieve remission from their symptoms than patients diagnosed at younger ages, even when those patients receive similar treatments, according to research at Washington University School of Medicine in St. Louis.
The study, published in the August issue of Clinical Gastroenterology and Hepatology, is the first to look at patients whose colitis was treated with modern medications, from the relatively mild, maintenance drugs known as 5-aminosalicylates to immunosuppressive therapies such as steroids and the drug infliximab, which targets specific proteins in the body’s immune system to help control inflammation.
Nearly 1 million U.S. adults have ulcerative colitis. The related Crohn’s disease can affect any part of the gastrointestinal tract, but ulcerative colitis patients have inflammation only in the lining of the large intestine or colon. The condition often causes diarrhea, bloody stool, weight loss and fever. In severe cases, some patients need surgery to remove the colon.
How To Stay Healthy
Keep up with treatment even when you’re in remission. That means you need to take your medicine even if you feel good. See your doctor at least once a year so they can see how things are going. And like everyone else, it’s important to stay active and follow a healthy diet.
Get regular screenings for colon cancer. Your doctor will let you know how often you should get checked. You may need a colonoscopy every 1-3 years. That’s a procedure that helps your doctor look for cancer or cells that might become dangerous. Your chances of recovery go way up when you find and treat colon cancer early.
Show Sources
Sudden Severe Ulcerative Colitis
This complication is the main cause of emergency surgery in patients with ulcerative colitis. With sudden, severe ulcerative colitis, medications and intravenous steroids, are unable to control the symptoms.
-
Uncontrolled bleeding can occur from deep ulcerations in the colon, though that is rare.
-
Severe, sudden ulcerative colitis can lead to toxic megacolon, a potentially life-threatening complication caused by severe inflammation.
-
Toxic megacolon leads to rapid enlargement of the colon. Symptoms include pain, distension or swelling of the abdomen, fever, rapid heart rate, constipation, and dehydration.
-
Toxic megacolon requires immediate treatment and surgery.
Also Check: Foods Not To Eat With Ulcerative Colitis
Ial Or Total Colon Resection
In a total resection, the entire large intestine is removed. While this is the only true cure for UC, it can reduce quality of life.
In a partial resection, colorectal surgeons remove the diseased region of the colon with a margin of healthy tissue on either side. When possible, the two remaining ends of the large intestine are surgically united, reconnecting the digestive system.
When this cant be done, the bowel is routed to the abdominal wall and waste exits the body in an ileostomy or colostomy bag.
With modern surgical techniques, its potentially possible to reconnect the remaining bowel to the anus, either during the initial resection surgery or after a healing period.
What Kinds Of Surgeries Are Done
Two surgeries are commonly done.
- Ileoanal anastomosis. This surgery is the most common. It removes the large intestine and the lining of the rectum, but you can still have nearly normal bowel movements after the surgery. This surgery is usually successful. About 7 or 8 out of 10 people have no problems after surgery. And most people say their quality of life is better.footnote 2
- Proctocolectomy and ileostomy. People who can’t be under anesthesia for long periods of time because of illness or age are more likely to have this surgery. It removes the large intestine and the rectum. After this surgery, you will wear an ostomy bag that is attached to an opening in your belly to collect body waste. This surgery has a lower risk of problems after surgery compared to ileoanal anastomosis.
You doctor may recommend surgery if:
- Medicines and nutritional therapy have failed to manage severe symptoms.
- Holes develop in the large intestine .
- You have colon cancer, a significantly increased risk of cancer , or a narrowing in the intestine that cannot be distinguished from cancer, even if you do not have symptoms of active disease.
- Severe bleeding requires ongoing blood transfusions.
- Slow growth or other serious complications occur in a child.
You may choose to have surgery to improve your quality of life, cure ulcerative colitis, or prevent the possibility of colon cancer.
Recommended Reading: What Foods Should Be Avoided With Stomach Ulcers
Symptoms Of Ulcerative Colitis
Usually the first sign of ulcerative colitis is loose stools that are often bloody. This may be accompanied by abdominal cramping and an urgency to move your bowels. A decreased appetite, weight loss and fatigue are common symptoms as well. Some patients with ulcerative colitis will have skin lesions, joint pain, eye inflammation and liver disorders. Approximately half of all patients with ulcerative colitis have very mild symptoms. Symptoms can also come and go, with long periods between flare-ups.
Enhancing Healthcare Team Outcomes
Ulcerative colitis is a systemic disorder with no cure. The disorder has numerous extraintestinal involvement in addition to the colon. Thus, it is best managed by an interprofessional team. All patients with the disorder need lifelong monitoring. Because of the risk of colorectal cancer, surveillance colonoscopy should occur every 1-2 years. Further, since patients are often treated with biological agents, they need to undergo screening for melanoma and nonmelanoma skin cancer.
The pharmacists should assist the team by educating the patient on the importance of medication compliance to avoid relapse. The nurse should encourage regular vaccinations, hand washing, and cancer screening. A dietary consult should be obtained to educate the patient on foods to eat and what not to eat, especially if they have a stoma. In addition, a stoma nurse should be involved in the teaching of stoma care.
An infectious disease nurse should monitor the patient in the outpatient setting to ensure that they are not immunocompromised. Social workers should be involved to ensure that the patient has ample support and finances so that the treatments are not missed. Patients with risk factors for osteoporosis need screening for bone mineral density periodically. Patients should be encouraged to undergo annual vaccination against influenza and pneumococcus. Finally, many patients with ulcerative colitis develop depression and anxiety and should be referred to a mental health counselor.
Outcomes
Also Check: How Do You Treat An Ulcer Naturally
Personal Stories About Surgery To Cure Ulcerative Colitis
These stories are based on information gathered from health professionals and consumers. They may be helpful as you make important health decisions.
I have suffered from some really bad symptoms from ulcerative colitis. The diarrhea and pain interrupt my life. I can’t go anywhere without checking out where all the washrooms are. I don’t dare go on long hikes or go skiing, things I used to do all the time. It makes me depressed. I like the idea of having surgery so I don’t have to deal with this illness anymore.
Toni, age 33
The symptoms of ulcerative colitis can be painful and embarrassing, but I only get them a few times a year. My medicines control them really well. I don’t think my condition is bad enough for me to have surgery, and I don’t like the thought of having to use an ostomy bag. I think I will wait and see if my condition gets worse.
Carolyn, age 40
I want to have surgery, because I’m scared of getting colon cancer. I had an uncle who had colon cancer. My risk is already higher than average because I have ulcerative colitis. Besides, I’ve had this disease for 7 years. In another year, I have to start having an annual colonoscopy to check for cancer. If I have surgery, I won’t have to deal with symptoms or be tested every year and worry about colon cancer.
Bill, age 27
Juan, age 30
Complications Of Ulcerative Colitis
UC increases your risk of developing colon cancer. The longer you have the disease, the higher your risk of this cancer.
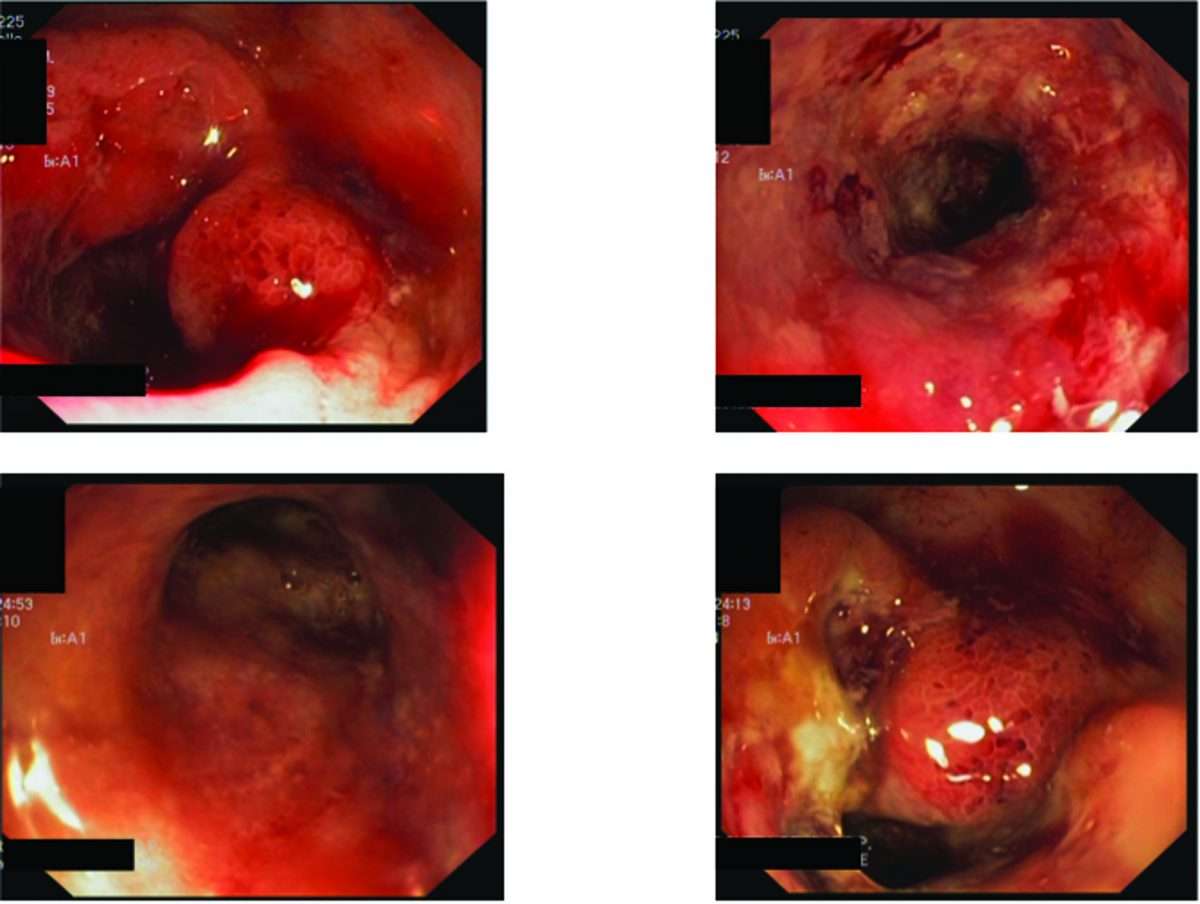
Because of this increased risk, your doctor will perform a colonoscopy and check for cancer when you receive your diagnosis.
Repeat screenings are recommended thereafter, according to the American Cancer Society. Regular screenings help lower your risk of colon cancer. Follow-up screenings can detect precancerous cells early.
Other complications of UC include:
- thickening of the intestinal wall
- intestinal bleeding
You May Like: How Do They Test For Ulcerative Colitis
What About Network Meta
Principles of network meta-analysis.9
After the quality of the evidence is assessed, recommendations are developed and graded to differentiate those based on strong evidence from those based on weak evidence.5 This information is intended to provide the user with an estimate of the groups confidence that following the recommendation will produce the desired health outcome.7 As with levels of evidence, many classification schemes have been developed for grading recommendations. The GRADE approach is commonly used to grade the strength of recommendations and has been adopted as the standard by many guideline developers and organizations, including the AGA and the ACG.4,11,12 The GRADE approach typically scores the strength of recommendations as either strong or weak, also known as conditional or discretionary.2,6 While the GRADE approach acknowledges that expertise is required to interpret any form of evidence, it considers that opinion is an interpretation ofrather than a form ofevidence.6
Once recommendations are developed and graded, the guidelines are then made available for public policy evaluation. This step is critical, Dr Feagan pointed out, because there is no point in having guidelines if they cant be implemented. Lastly, the guidelines are submitted for peer review and published.
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Read Also: Pressure Ulcer Prevention Care Plan
Ulcerative Colitis During Pregnancy: What To Do
Pregnancy is quite possible when you have ulcerative colitis, as long as the disease is in remission.reassures the general practitioner, before alerting. Fertility is normal except in the event of an acute attack and there is a pronounced risk of prematureMost treatments for recto colitis are compatible during pregnancy.Biotherapies can be continued during pregnancy with, however, a stop in the 3rd trimester..
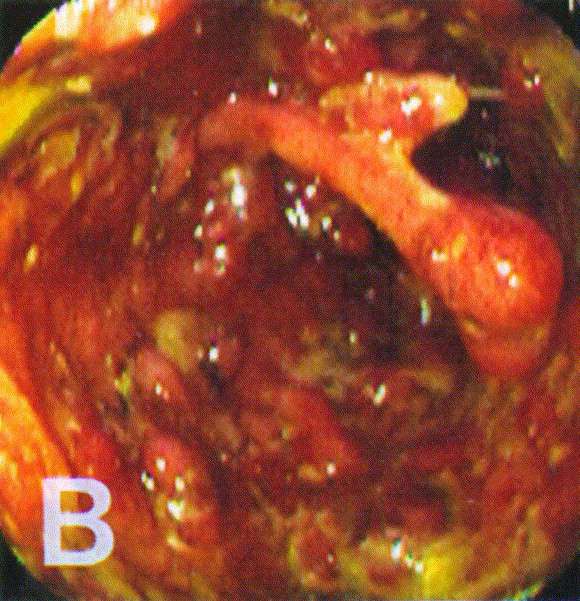
The diagnosis of ulcerative colitis is made on the basis of clinical and paraclinical arguments . We will thus examine the wall of the patients rectum and colon during a endoscopic colonoscopy . At the same time, a biopsy and an anatomo-pathological examination will be practiced, continues the doctor. According to the ARS, at the time of the diagnosis of RCH, in approximately 50% of the cases, the attack concerns only the rectum .There may be a Increased risk of colon cancer in patients with pancolic UClinked to the persistence of inflammation, confides the deputy director of Afa. But this excess risk is controlled when regular monitoring is established by colonoscopy after ten years of disease progression.
Consult when you have digestive symptoms or when a family member is affected ulcerative colitis for screening
Uc Therapy And Immunology In The Modern Medical Era
Following World War II, the era of randomized clinical trials began, ushering in the modern age of evidence-based medicine. A landmark UC study from this time was Sloan’s exhaustive series of the clinical features of 2000 UC patients published in 1950. Subsequent clinical trials began to establish the efficacy of pharmacologic interventions. In 1955, Truelove published the first blinded, controlled trial in UC patients in the British Medical Journal, demonstrating improvement and decreased mortality for patients taking corticosteroids when compared to control subjects.
A major conceptual shift followed the report of Swedish physician Nanna Svartz , who serendipitously discovered impressive UC symptom resolution after treatment with sulfasalazine. In an attempt to cure the arthritis of his King, Gustas V, Svartz had synthesized this new drug by chemically bonding sulfapyridine, a known antibiotic, with 5-aminosalicylic acid , an anti-inflammatory. When reviewing his trial data, Svartz noticed that those arthritis patients who also had UC experienced symptom relief. Years later, another RCT would demonstrate that the 5-ASA component of sulfasalazine was also effective for UC, thus providing another anti-inflammatory drug for treating UC with a better adverse effect profile than sulfasalazine.
Don’t Miss: Best Thing To Take For Stomach Ulcer Pain
Elective Colorectal Cancer Surgery
Patients with Crohns disease and ulcerative colitis have a higher risk for colorectal cancer than the general population, so elective surgery may be recommended to eliminate that risk.
Colorectal cancer risk factors
-
The risk of CRC increases after living with IBD for 8 to 10 years
-
The risk increases the longer a person lives with IBD
-
The greatest risk is for people with IBD affecting their colon
-
Patients who have a family history of primary sclerosing cholangitis are also at higher risk of developing colorectal cancer
In most cases, colorectal cancer starts as a polyp, or a small lump growing from the wall of the intestine. Polyps typically start out benign but become cancerous over time. But in patients with IBD, abnormal and potentially precancerous tissue, called dysplasia, may lay flat against the wall of the intestine and can even be found in areas of the intestinal wall that appear normal during a colonoscopy.
Diagnosis Of Ulcerative Colitis
A diagnosis of ulcerative colitis can be suspected based on the presenting symptoms. Your doctor initially may order blood work and stool tests. Your doctor will also want to perform a colonoscopy to directly visualize the lining of the colon. This is an out-patient procedure to examine your colon using a flexible fiber-optic scope. The exam is done under sedation and is quite painless. The doctor will take biopsies of your colon for a pathologist to evaluate.
Also Check: What Not To Eat With Bleeding Ulcers
Don’t Miss: How Do You Get A Peptic Ulcer
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
During surgery, your small intestine will either be diverted out of an opening in your abdomen or be used to create an internal pouch thats connected to your anus called an ileoanal pouch.
Also Check: Icd 10 Venous Stasis Ulcer Left Leg
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
The Crohn’s Colitis Cure
Progress is made by trial and failure the failures are generally a hundred times more numerous than the successes yet they are usually left unchronicled. This book brings together the successes throughout history regarding Colitis and Crohns into one place, Combined they produce a profound strategy to reverse the condition.
Inflammatory Bowel Disease costs an estimated $44 Billion per year world-wide. It is a condition on the increase. There seems to be little incentive to change this condition from “incurable”. Here is a book that blows the lid off the treatment of this autoimmune disease and the industry built up around it. Its time to take control of your health, and learn how to free yourself from this diagnosis.
This is not a pill it is a road map that will guide you on a journey towards a cure. Outlining a protocol for reversing Ulcerative Colitis and Crohns Disease, a result of 30 years research by the author a protocol your doctor is unlikely to mention.
We would accomplish many more things if we did not think of them as impossible. Vince Lombardi
Also Check: Nanda Nursing Diagnosis For Ulcerative Colitis