Soothe Skin Irritation And Pain
Bouts of diarrhea often can bother your skin. Use moist towelettes for wiping. Follow up with a petroleum jelly ointment. Need more relief? Soak in a saltwater bath, which may ease soreness. Try acetaminophen for pain, but avoid NSAIDs, such as ibuprofen and naproxen. They can trigger flares and cause other problems.
Be Consistent With Treatment Drugs
Take your medications consistently. Dont miss or skip a dose even when in remission. Dont try to wean yourself off of a treatment drug as these changes can all lead to flares.
Contact Digestive Health Services at if you have any changes to your flares, or if you think you might have ulcerative colitis.
What Are Ulcerative Colitis Flare
Ulcerative colitis is a condition which affects thousands of people across the UK. Luckily, many people with ulcerative colitis flare-ups receive advice and treatment, meaning the condition has minimal impact on their quality of life.
This doesnt mean flare-ups are completely avoidable though. Depending on whether you have proctitis, distal or total colitis, a flare-up may have different effects on the individual. Knowing how to recognise and manage these effects is very important.
In this short blog post, we will discuss what happens during a flare-up and how best to alleviate problems when it does.
Also Check: Wound Care For Stage 4 Pressure Ulcer
Read Also: What Age Does Ulcerative Colitis Start
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
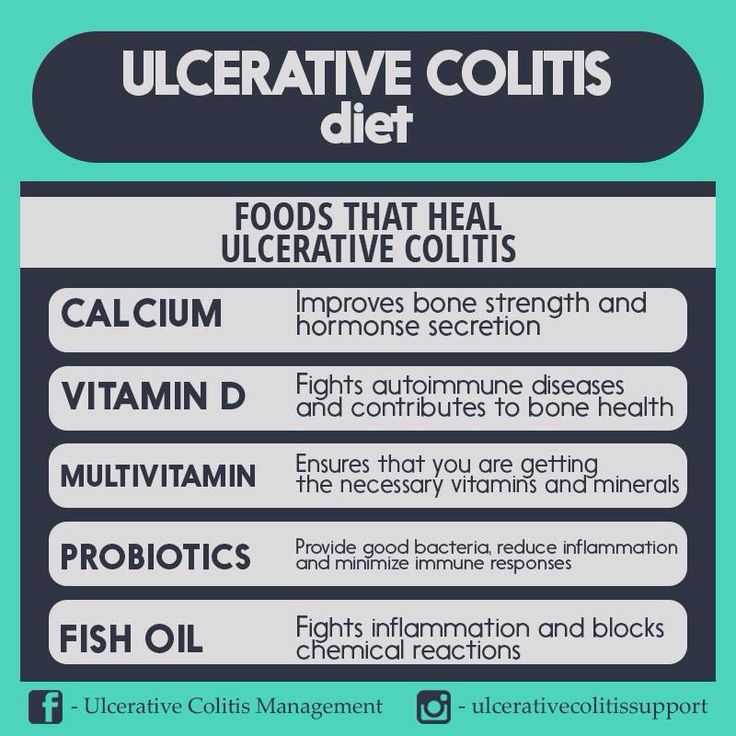
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Read Also: New Drugs For Ulcerative Colitis
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Identify Daily Stressors And Put Your Health First
The second tip to help you prevent an ulcerative colitis flare-up is to ensure that you learn how to identify daily stressors so that you may eliminate them. Stressors for many people come up on a daily basis, whether it be work based, family based, or even relationship/friends based. I think that always keeping in mind that your health comes first no matter what. In other words, no issue is as important as your own health. By always keeping this in mind I find that it helps me mentally to filter things that brings stress instead of peace.
Recommended Reading: Foam Boots For Pressure Ulcers
Also Check: How To Fix An Ulcer In Your Stomach
How Do I Know If My Uc Has Gone Into Remission
UC doesn’t have a cure. Instead, the goal of any treatment plan is to send the disease into remission.
When UC is in remission, you don’t experience as many symptoms and start to feel better. If your UC medications and lifestyle changes work well for you, remission may last for months or even years. There are several different kinds of remission:
- Clinical remission: When a patient isn’t experiencing symptoms and may feel better.
- Endoscopic remission: Testing of the intestinal lining shows no inflammation
- Biochemical remission: Blood and stool tests show no sign of inflammation
- Surgical remission: When UC goes into remission after surgery to treat it
- Histologic remission: When both clinical and endoscopic tests didn’t show signs of UC
With UC, it can feel like life revolves around symptoms. If UC symptoms keep coming back, it can be a sign that medications aren’t working. Consider taking part in a clinical trial researching an investigational treatment option for people living with UC.
To Ease Abdominal Pain
As your doctor treats the flare, your abdominal pain should get better. Remember to avoid nonsteroidal anti-inflammatory drugs , but Damas also recommends avoiding opioid analgesics . Your doctor may prescribe an antispasmodic medication, which relaxes the gut muscles.
Warning signs of a flare: People with ulcerative colitis often experience abdominal pain, but if the pain is worse or markedly different from your baseline, Damas recommends calling your doctor. Red flags that require medical attention include fever, fatigue, and intense abdominal pain.
Also Check: Does Kefir Help Ulcerative Colitis
How To Calm An Ulcerative Colitis Flare
This article was co-authored by Peter Gardner, MD. Peter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelors degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.There are 8 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 14,663 times.
Ial Or Total Colon Resection
In a total resection, the entire large intestine is removed. While this is the only true cure for UC, it can reduce quality of life.
In a partial resection, colorectal surgeons remove the diseased region of the colon with a margin of healthy tissue on either side. When possible, the two remaining ends of the large intestine are surgically united, reconnecting the digestive system.
When this cant be done, the bowel is routed to the abdominal wall and waste exits the body in an ileostomy or colostomy bag.
Read Also: Best Medication For Stomach Ulcers
How Does The Severity Of Your Ulcerative Colitis Affect Treatment
Thereâs no cure for ulcerative colitis. But treatments can help ease your symptoms, inflammation, and treat underlying conditions. With any form of ulcerative colitis, the goal is to go into remission and stay there. Certain medications work well to ease mild-to-moderate symptoms. There are also treatment options for more severe ulcerative colitis.
To improve your quality of life, your doctor may suggest:
Aminosalicylates. If you have mild to moderate ulcerative colitis, sulfasalazine may help your symptoms. Make sure to let your doctor know if youâre allergic to sulfa. If you are, they can give you alternatives.
Youâll take these drugs in capsule form through your mouth. They also come in a rectal form , which means youâll put it in your bottom.
Corticosteroids. For severe cases of ulcerative colitis, your doctor might suggest prednisone or budesonide . These drugs have serious side effects though. Your health care team will only suggest them for short-term use. Theyâll give you other drugs to help keep you in remission.
You can take these medications through your mouth, bottom, or through an injection.
Biologics. These are good options for moderate to severe ulcerative colitis. They target parts of your immune system to ease symptoms. Some you might try are adalimumab , certolizumab pegol , golimumab , or others.
Your doctor will give these to you through an IV. You may be able to give yourself these medications if your doctor allows you to do so.
Show Sources
Tips To Prevent An Ulcerative Colitis Flare

Please note: This article outlines 11 tips to help you prevent an ulcerative colitis flare, and is based on one patients experience. Nothing in this article is meant to replace any advice you have received from your doctor. This article was contributed by Ms. Wanni Z. Below is her story.
Every day during remission I am thankful. I remind myself constantly that I should not take it for granted. I feel that its important to never forget that there is currently no cure for ulcerative colitis . Even during periods of remission, we still need to take daily measures to ensure that we prevent any potential flare-ups. That being said, here are some key points I have learned that have helped my body over the last few years, I hope this will help others out there! Keep reading for some tips to help you prevent an ulcerative colitis flare:
You May Like: Icd 10 Code For Ulcerative Colitis With Bleeding
How To Treat An Ulcerative Colitis Flare
The great thing about the internet is that you have constant access to information on any topic you want to learn about. The bad thing about the internet is that it can be difficult to determine a credible source from a phony one. When it comes to finding information on how to best manage GI conditions like Ulcerative Colitis , online information can often be contradicting and confusing. Thankfully, were up to date on the current research and recommendations to help you best manage your Ulcerative Colitis symptoms.
The tough part about ulcerative colitis management is that our recommendations are specifically tailored to your stage of ulcerative colitis- active or dormant .
Keep Stress To A Minimum
With stress, your body produces higher cortisol levels, a stress hormone that can cause inflammation and UC flares.
While you may not be able to entirely stop your stressful days, there are some things you can do to help reduce your stress levels and keep yourself in a healthy state of mind. These include:
- getting enough sleep
Read Also: Foods Okay To Eat With An Ulcer
Foods To Eat During An Ulcerative Colitis Flare
Avoiding certain foods is only half the battle. Heres how to get the nutrients you need during an ulcerative colitis flare.
Jeff Wasserman/Stocksy
If you have ulcerative colitis, you may already know which foods worsen your flares. But figuring out what to include in your diet is equally important, because the right foods will provide you with key nutrients without aggravating your symptoms.
Most experts recommend that you limit your fiber intake when youre having an ulcerative colitis flare. A general rule is to replace high-fiber foods, such as nuts, seeds, and raw fruits and vegetables, with more easily digestible fare. Here are eight foods to eat during an ulcerative colitis flare and the reasons they can help.
1. Applesauce: Since your gastrointestinalsystem is experiencing a lot of irritation during a flare, you may want to stick to soft, easily digestible foods like applesauce. Be sure to choose an unsweetened variety though, because added sugar can cause more inflammation. You can also make your own sugar-free applesauce by cooking peeled, sliced apples with some water and then pureeing the mixture.
3. Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K. Just make sure the vegetablesare thoroughly cooked until they can be mashed with a fork, Szeles says so that any potentially irritating fiber is broken down.
Additional reporting by Nina Wasserman
How To Treat Ulcerative Colitis
The treatment of Ulcerative Colitis also depends upon the severity of the patient. The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis.
Following drugs may calm down the inflammation and make the patient feel better.
Read Also: Compression Stockings For Leg Ulcers
Natural Intestinal Healing Remedies
Due to the common complaints associated with medications and surgery, research has uncovered many natural options for healing a damaged digestive system. From lifestyle changes, dietary adjustments, and stress reduction techniques, ulcerative colitis can not only be prevented, but it can also be successfully healed.
One additional benefit is that many people, especially the elderly, cannot tolerate many medications. Natural options allow for healing without additional pain. These include:
Regular Exercise: Exercise is beneficial to your overall health, but when it comes to ulcerative colitis, regular activity can help with many of the complications associated with the condition. Studies have shown that individuals with ulcerative colitis also suffer from decreased bone density, emotional health problems, weight gain, and suppressed immune system.
| Related: Why a Workout Plan Improves the Benefits of Probiotics |
Exercise can help boost moods, promote weight loss, boost energy levels, and support bone health. In addition to this moderate exercise triggers the release of specific chemicals called myokines that promote healing from inflammatory-related damage.
Yoga is a specific exercise that takes care of the digestive system and provides relief for many ulcerative colitis symptoms.
Stress Reduction: Stress and anxiety are intricately linked to inflammation. The release of inflammatory chemicals is a direct result of the body experiencing stress.
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Recommended Reading: Does Ulcerative Colitis Cause Hair Loss
Find New Stress Management Techniques
Stress can trigger a colitis flare-up, so practice stress management techniques to reduce as much external stress on your body as possible.
Why does stress affect irritable bowel diseases so easily? Cortisol can increase inflammation in your body, and learning to manage stress can help you reduce that inflammatory response.
Reduce your stress levels through:
- Practicing deep breathing
- Prioritizing self-care
Self-care includes getting enough sleep each night, following a well-balanced diet, and setting aside time for your favorite activities each day.
All About Telehealth For Ulcerative Colitis

2022 Healthgrades Operating Company, Inc. The content on Healthgrades does not provide medical advice. Always consult a medical provider for diagnosis and treatment. All rights reserved. May not be reproducedor reprinted without permission from Healthgrades Operating Company, Inc. Useof this information is governed by the Healthgrades User Agreement.
Also Check: High Carb Diet For Ulcerative Colitis
Make Sure Youre Getting Enough Probiotics And Prebiotics
Whether you take probiotics tablets, eat fermented vegetables or other fermented products, or take kefir, I personally try to intake something with probiotics and prebiotics at least a few times a week. My personal favourite is a kefir smoothie its an excellent combination of probiotics and prebiotics! Learn more about how to choose the right probiotics here.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Read Also: Treating Ulcers In Horses With Omeprazole