What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohns disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Read Also: Does Kefir Help Ulcerative Colitis
Dairy Is A Common Trigger Food For People With Ulcerative Colitis
Lactose intolerance is a common issue affecting the general population, as well as people with ulcerative colitis, says Themistocles Dassopoulos, MD, the director of the Baylor Center for Inflammatory Bowel Disease in Dallas. Lactose intolerance prevents you from properly digesting lactose, the sugar found in milk and dairy products, because the small intestine lacks the digestive enzyme called lactase. While dairy doesnt seem to cause UC flares, lactose intolerance can cause symptoms such as abdominal pain and diarrhea that can be mistaken for UC. Avoid dairy products or add lactase supplements to reduce these symptoms.
Association Between Inflammatory Potential Of The Diet And Ulcerative Colitis: A Case
- 1Students’ Scientific Research Center, Tehran University of Medical Sciences, Tehran, Iran
- 2Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran
- 3Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
- 4Department of Community Nutrition, School of Nutrition and Food Science, Isfahan University of Medical Sciences, Isfahan, Iran
- 5Department of Medicine, University of Alberta, Edmonton, AB, Canada
- 6Integrative Functional Gastroenterology Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
- 7Obesity and Eating Habits Research Center, Endocrinology and Metabolism Molecular -Cellular Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
Background/Aim: Despite the inflammatory nature of inflammatory bowel disease , limited data are available on the association of inflammatory potential of the diet and risk of ulcerative colitis . We aimed to investigate the association of inflammatory potential of the diet score and odds of UC in a case-control study.
We found that adherence to a pro-inflammatory diet was positively associated with greater odds of UC. Further studies are required to confirm these findings.
Also Check: What Do You Do For An Ulcer In Your Stomach
Ulcerative Colitis Diet: What To Eat In A Flare Up
A low residue diet is often recommended to manage symptoms of ulcerative colitis. The Canadian Society of Intestinal Research outlines residue as the solid contents that stay in the bowel after digestion, with the goal of reducing the number of bowel movements that happen in a day. Residue includes fiber, which is limited to 10-15g per day, but the low residue diet differs from the low fiber diet by including foods that may stimulate frequent bowel movement, such as dairy, caffeine, alcohol and gristly or fatty meat.
Dr Deborah Lee, of Dr Fox Online Pharmacy, recommends the following foods for a low residue diet:
- Low fiber fruit and veg such as melon and bananas, as well as stewed fruit
- Lean protein such as white meat, eggs and tofu
- Refined grains such as white bread, white pasta and oatmeal
- Cooked seedless and skinless vegetables such as cucumber, potato and squash.
Cooking your food may also break down some of the dietary fiber to make it more digestible, as seen in a study in the journal of Plant Foods for Human Nutrition , which indicates that the process of cooking decreases the amount of insoluble dietary fiber in some vegetables.
Quick Tips For Nausea
If youre really having trouble keeping things down, here are a few of my tips:
- Be cautious about how much volume youre putting in and what ingredients you may be substituting. If youâre youâre questioning if youâll be able to keep it down at the rate that its dissolving, or wondering if it may just come right back up and leave you back to where you started ⦠consider this.
- Iâve heard of others using cupcake wrappers to poke through and hold the contents that melt if not consumed quickly enough. Cool, huh? But, eating faster doesnât mean better if youâre vomiting. If you find this to be true, consider putting less in each cube.
- Major nausea hack: In the past, Iâve taken a couple of tablespoons of the purée and placed pureed contents into one corner of a few small Ziploc bags. Freeze that, then cut off a very small tip of the corner of the bag, so when youâre ready to eat one, you can consume it at a slower rate.
Dont Miss: Wound Care For Diabetic Foot Ulcers
Read Also: Biological Medicine For Ulcerative Colitis
Swap Wheat Bran With Oatmeal Or Corn Flakes
Wheat bran and bran flakes are high in insoluble fiber, which passes through the gut undigested. Heart-healthy oatmeal, though, is a good source of soluble fiber, so its good to eat, even during a flare, says Cavagnaro. Plain, less processed oats are better. Avoid prepared oatmeal packs.
A study published in March 2019 in the journal Frontiers in Immunology reported that short-chain fatty acids, such as butyrate, which are produced by the good bacteria in the GI tract, have an anti-inflammatory effect in the intestines. You can find foods that produce short-chain fatty acids in whole grains, fruits, and vegetables.
Other cereals worth trying are cornflakes, Cheerios, and Rice Krispies. For hot cereals other than oatmeal, try grits or Cream of Wheat.
Read Also: Indian Diet For Ulcerative Colitis
How Can I Track Foods That Cause Flare
The Crohn’s and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohn’s and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
Also Check: What Is The Treatment For Ulcers
What To Eat After Surgery
If you have an operation for your UC, your doctor will ask you to stick to a soft, bland diet while your body heals. Gradually, you can start to eat foods with more fiber.
Depending on the kind of surgery you have, you might be able to eat anything after you’ve recovered, even things that caused problems when your UC was active.
Show Sources
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
Recommended Reading: Can You Drink Beer With Ulcerative Colitis
Eating When You Are In A Flare
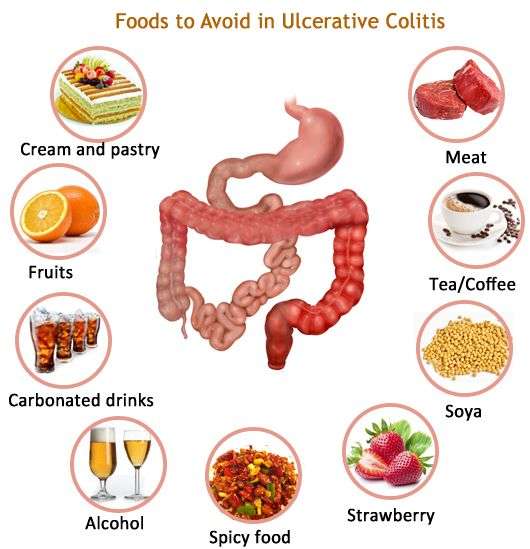
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
Eating With A Stricture
If you have a stricture , you may need to change what you eat to help prevent the intestine getting blocked.You might be advised to avoid foods that could block the intestine, such as:
If you have a severe stricture, you may only be able to eat very soft or liquid foods.Its important to speak to a dietitian to make sure youre eating a healthy, balanced diet. In some cases, they may recommend a vitamin and mineral supplement.
Also Check: What Medicine To Take For Stomach Ulcers
Also Check: Method For Cleaning Leg Ulcers
Foods To Avoid During Ulcerative Colitis Flares
During a flare, ulcerative colitis symptoms become more severe, and certain foods can worsen them further.
Following these guidelines can keep you away from the most common food triggers during UC flares:
- Avoid high-fiber foods, such as whole grains, dried fruit, and raw vegetables or vegetables with tough skin. Make sure to cook vegetables thoroughly, and avoid vegetables with seeds.
- Avoid cruciferous vegetables that produce gas, such as broccoli, cauliflower, and Brussels sprouts.
- Avoid spicy foods.
- Avoid caffeine in coffee, tea, and other beverages. This can contribute to diarrhea.
- Avoid whole nuts and seeds. Choose smooth nut butters. Almond butter, peanut butter, cashew butter, and sunflower butter are all great choices.
- Avoid fried foods, fatty foods, and highly processed foods.
- Avoid high-sugar foods, like fruit juice and baked goods. These can contribute to diarrhea.
Some members of MyCrohnsAndColitisTeam learned about their food triggers the hard way. Last time I drank coffee, I felt every centimeter of my intestines. Big no for me, shared one member. Another member communicated her hard-won personal rule very clearly: No sugar, and I mean NO SUGAR AT ALL!
What Should I Eat
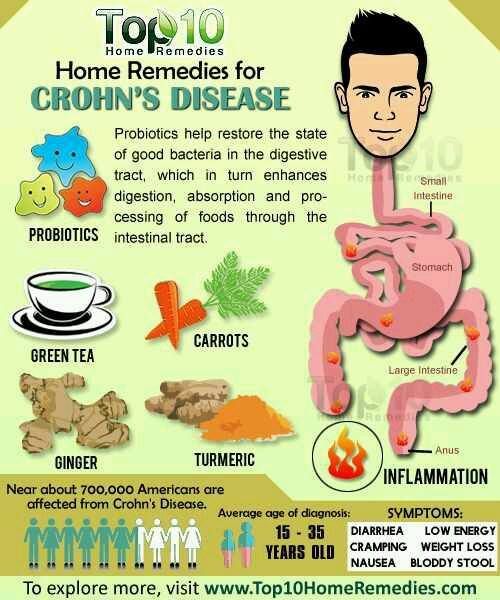
Its not always easy knowing what foods best fuel your body, especially when you have Crohns disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, thesymptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
Recommended Reading: Antibiotics For Leg Ulcer Infection
Read Also: What Are The Signs You Have An Ulcer
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
What Is The Best Diet For Colitis
Colitis is a type of inflammatory bowel disease. People who suffer from it can experience bloody diarrhea, abdominal cramps, or an inability to move the bowels. While the inflammation of the intestine is not necessarily caused by the foods a person eats, some people may have a worsening of symptoms after eating dairy products or foods that commonly cause gas. The best diet for colitis may be one that avoids too much fiber, dairy, and alcohol, and that includes plenty of protein, refined grains, and healthy fats. An effective meal plan may require that a person trade in three larger meals for five or six small ones each day.
When coming up with the best diet for colitis, a person should record everything he consumes and note any symptoms he experienced after eating a certain food so that he can avoid it in future. Some people may find that its best to avoid dairy products. Lactose in milk and other dairy products can make symptoms flare up. In some cases, taking lactase may help calm the condition.
Read Also: Natural Relief For Stomach Ulcers
Ulcerative Colitis Diet: Advice From A Dietitian
If you have ulcerative colitis, knowing what to eat can be tricky. Its important to customize your food choices based on your current tolerance and health goals. This post will help you understand the current scientific thinking on ulcerative colitis and diet and how to move forward with the approach that is right for you.
We have been working with clients with Crohns disease and ulcerative colitis in our practice for over seven years its an area I am passionate about because of the massive toll these diseases take on peoples quality of life. I also believe that nutrition can play a much larger role in the management of the diseases than is often discussed in the doctors office.
As a dietitian, I believe that the goal of nutrition is more than just ensuring you get all the vitamin D you need. I believe and have seen firsthand in my practice that creating a strong individualized approach to nutrition can help people find healing and learn how to thrive, no matter their diagnosis. Which is why it is frustrating that much of the scientific literature on ulcerative colitis is focused on either associating the risk of disease with certain foods, or acute strategies for securing remission in a flare.
General Guidelines When Ulcerative Colitis Is In Remission
Some members of MyCrohnsAndColitisTeam find they can eat a wider variety of foods safely during remission periods when ulcerative colitis is not as active and symptoms are absent or mild. Still, every individual is different, and purportedly beneficial foods may trigger symptoms. Trial and tracking is the only way to know for sure.
If it is safe for you, these guidelines may help you stay your healthiest during remission:
- Get 25 grams to 35 grams of fiber per day to promote bowel regularity and reduce inflammation.
- Consume plenty of lean meats, which are a good source of B vitamins. Include fatty fish, tofu, and nut and seed butters.
- Include probiotic foods such as yogurt, tempeh, kefir, kimchi, miso, and sauerkraut.
While some members find kefir too sour for their liking, others report experiencing benefits from trying the fermented drink. Kefir has been helping me over the past week, wrote one. Been trying kefir the past few days. Will keep you posted. So far less pain, said another.
You May Like: Best Fruits For Ulcerative Colitis