Left Sided Ulcerative Colitis/proctitis
There is overwhelming data to support the use of topical formulations of 5-ASA in distal left sided colitis. The question arises whether topical therapy alone is efficacious or if topical therapy combined with oral mesalamine would produce higher response rates. A study to compare the efficacy of mesalamine rectal suspension enema, Rowasa , alone, oral mesalamine alone, and the combination of enema and tablet in patients with distal UC found that the combination of oral and rectal mesalamine therapy was well tolerated and produced earlier and more complete relief of rectal bleeding than oral or rectal therapy alone . However, it has not been clearly defined whether this is a dose response effect or independently a benefit of topical therapy.
The combination of oral and rectal mesalamine therapy produced earlier and more complete relief of rectal bleeding than oral and rectal therapy alone. Pairwise analysis revealed that combination therapy resulted in significantly fewer days to cessation of rectal bleeding compared with either the mesalamine enema or mesalamine tablet group alone. Adapted from data: Safdi et al .
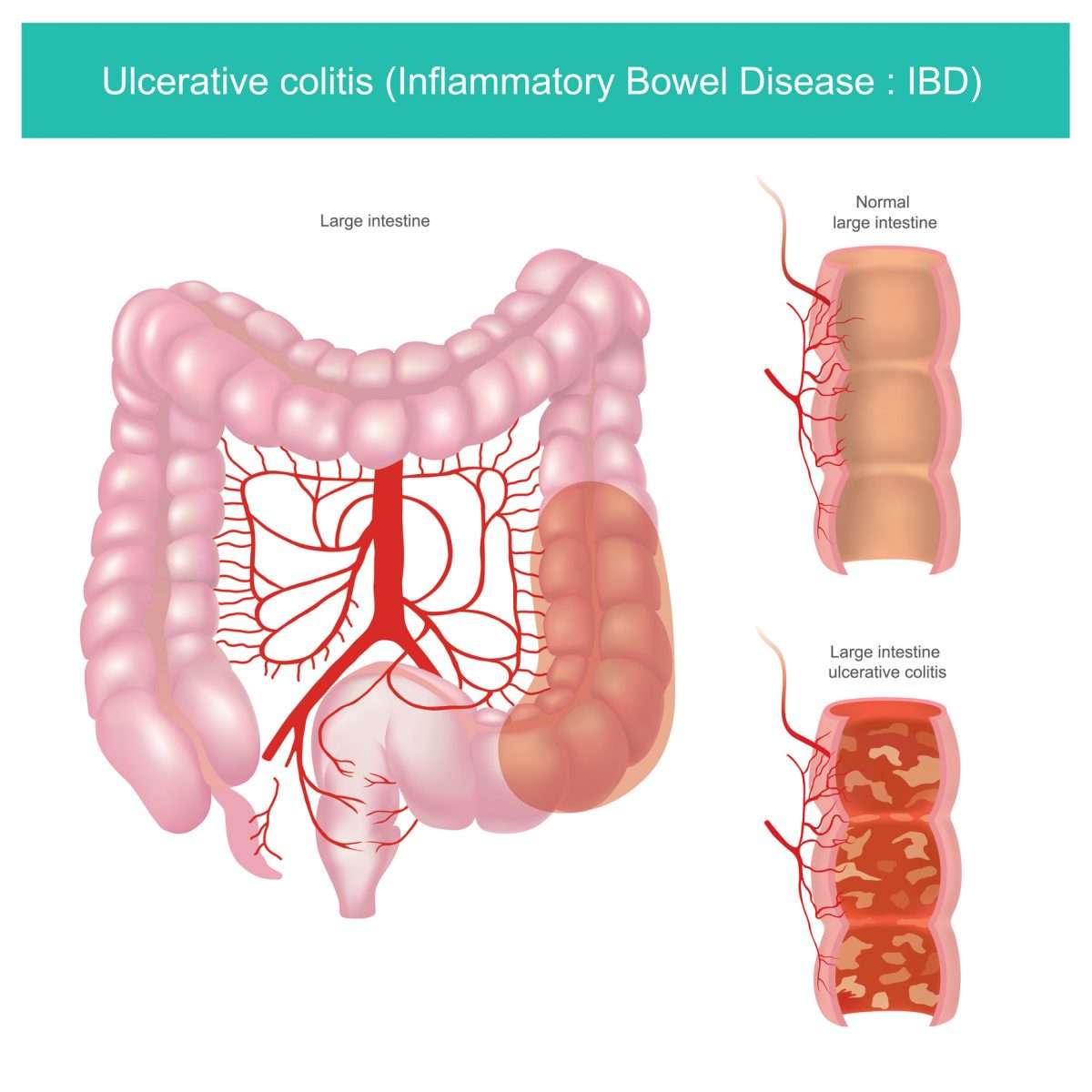
Will Ulcerative Colitis Affect Me Over Time
The effects of ulcerative colitis vary considerably from person to person, based on the nature and severity of their disease. In many cases, the condition does not have much impact on daily life, the ability to work or to enjoy an active social life but does take some getting used to. When it is at an active stage, symptoms such as diarrhoea and abdominal pain often require time away from work, college etc. and can make it difficult to cope going out or even being at home. However, treatment usually makes the symptoms better within days or weeks so normal quality of life can be restored quite quickly. Some severe cases of ulcerative colitis, however, can have a significant impact on peoples lives. This can be due to a weak response to treatment which makes symptom-free remission difficult to achieve and can involve frequent flare ups.
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohns Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohns disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Recommended Reading: Ulcerative Colitis Rectal Pain Relief
Crohn’s Colitis And Ulcerative Colitis Are Often Difficult To Distinguish Clinically What Are The Major Differences Seen At Colonoscopy
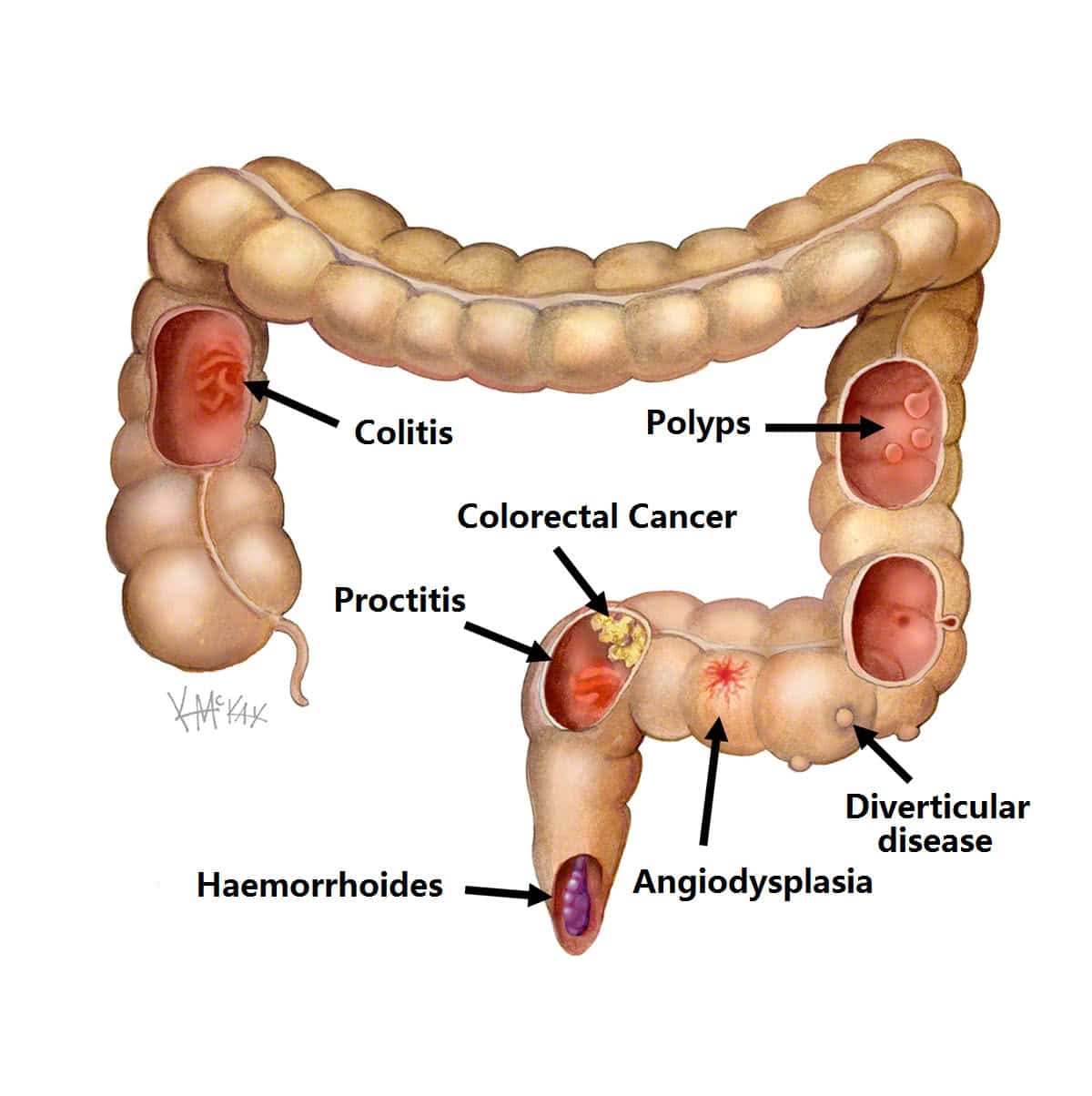
Crohn’s colitis is focal and predominantly right sided. Apthous ulcerations are the earliest lesions seen in Crohn’s disease. As the disease progresses, they may form linear or serpiginous ulcers in affected areas. When these large ulcerations migrate transversely, islands of normal mucosa appear, known as cobble stoning. In UC, disease begins in the rectum and progresses proximally. Skip areas are more common in Crohn’s disease, but be aware that UC patients treated with rectal suppositories or enemas may have a normal appearing rectum. Endoscopic findings in UC may range from simple edema of the mucosa to indurated, friable tissue that bleeds on contact.
How Is Ulcerative Proctitis Treated
Ulcerative proctitis is usually very responsive to treatment, says Dr. Yoon. Your doctor will likely start by prescribing topical therapy, which means youll either use a suppository or an enema with an anti-inflammatory medication called mesalamine.
Dr. Yoon explains that the recommendation is to either use it every single night or at least two or three times a week just to keep the inflammation from coming back. If it works, you should ideally continue using it every night moving forward.
But in a practical sense, most people dont want to do that. People with ulcerative proctitis are usually young, in their 20s, so getting them to use a suppository for the rest of their life is wishful thinking, Dr. Yoon says. I have patients do it for four weeks and if theyre feeling fine and symptoms are mild, they can go ahead and stop. In the future, if they start bleeding again, they can do it for another four weeks.
Treatment for ulcerative proctitis can also include corticosteroids, such as prednisone or budesonide, which help reduce inflammation. Treating ulcerative colitis in general can involve immune system suppressors, like the pill azathioprine, and biologics, which are antibodies given via IV infusion or an injection that stop certain proteins from causing inflammation, according to the Crohns & Colitis Foundation.
Read Also: How To Treat Bleeding Ulcer In Stomach
What Medications Can Cause Rectal Bleeding
Some of them can include:
- Alpha agonists such as Catapres-TTS
- Anticholinergic agents like Atropen and trihexyphenidyl
- Antihistamines such as Benadryl , Claritin , and
- Calcium channel blockers such as Cardizem , Norvasc , and Verelan
- Calcium and iron supplements, including antacids that contain calcium
- Histamine-2 receptor antagonists such as Pepcid and Tagamet HB
- Opioid pain relievers such as Anexsia
- Overactive bladder medications such as Detrol and Ditropan XL
- Parkinson’s disease medications such as Sinemet
- Tricyclic antidepressants such as amitriptyline and Norpramin
Nonsteroidal anti-inflammatory drugs such as Advil or Motrin and Aleve can cause intestinal ulcers that can lead to rectal bleeding.
There are other medications that can increase the risk of bleeding in the body. If theres an ulcer or another issue going on in the digestive system, a medication that increases bleeding could cause it to bleed more than it normally would.
Some of these medications are:
- Anticoagulants such as vitamin K antagonists, Coumadin , or heparin
- Corticosteroids, such as prednisone
- Direct oral anticoagulants such as Pradaxa , Eliquis , Savaysa , and Bevyxxa
- Platelet inhibitors such as Plavix or Effient
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Read Also: Do Ulcers Give You Diarrhea
How Is It Evaluated And Diagnosed
Your health care provider will evaluate rectal bleeding by asking questions, performing a physical exam, and doing some tests.
Your provider may ask questions such as:3,4,8
- What are your bowel movements like?
- Have you had any recent changes in bowel habits?
- Are your stools black or bloody? How often does this happen?
- Have you noticed blood on the toilet paper?
- Have you vomited recently? What did it look like?
- Have you had a recent colonoscopy?
- Have you had any recent trauma to the abdomen or rectum?
- What medications are you taking?
- Do you have a history of digestive or blood diseases?
- Have you been treated for prostate or pelvic cancer?
- Has anyone in your family had colon cancer?
- Have you experienced changes in weight recently?
Your health care provider may want to look at your stool.4 If you are in the hospital, you may be asked to use a special toilet or bedpan. If you are at home, your provider will instruct you on how to collect a sample.
Also Check: Signs Of Ulcerative Colitis Flare Up
A Terrible Colitis Flare And Bleeding
Thankfully, the bathroom was so small. Directly across the commode was the sink. As the dizziness continued and the nausea climbed my throat, I leaned my head against the edge of the sink. The cool ceramic lip offered support for my head while I continued to lose blood.
I dont recall how long I sat like that. I just remember that I stayed in that position for most of the evening. It was a terrible bout of rectal bleeding.
Looking back, I should have sought emergency medical attention. I didnt. But I did get to my gastroenterologist a few days later and ended up on prednisone.
Don’t Miss: Can Ulcerative Proctitis Be Cured
Consult The Gastroenterologist Regularly:
During your treatment, your gastroenterologist needs to see you for regular checkups and if you have any concerns or need help to manage Ulcerative Colitis flare-up, you should consult the physician. Establish a good relationship with your doctor and be honest about your symptoms and condition as how they are affecting you because this all helps the gastroenterologist to determine an appropriate treatment plan for you or makes changes in the prescribed treatment plan.
Number : Follow An Elimination Diet & Test Each New Food
This should be where you start.
The food list should be small initially.
It should comprise no more than 3-5 foods and should also be very minimal on the supplement front.
Yes, 3-5 foods is very limited, but thats the whole point.
This is so that your immune system does not have many potential triggers to react to.
And so that as you gradually introduce foods, you can work out what your triggers are.
Pick nutrient dense foods and/or add a multi-vitamin in the beginning to avoid any nutrient deficiencies.
There are many types of elimination diet.
Some of the main ones that people will use to stop an ulcerative colitis flare up are:
- A carnivore diet
Ive used all of these with my clients with good success.
There are others, of course, but these are the main ones.
As far as which specific foods to consume, stating the obvious, I cannot be more specific without knowing the dependences listed in the section above.
That being said, for the testing:
1. Consume 1 x serving of the new food you are testing once per day for 4 days.
Only test 1 new food at a time.
Be sensible with serving sizes if you are unclear on what a sensible serving size is, eat 0.5-0.75 cups of the specific food.
You can increase the serving size over time.
The new food can be consumed with other foods that youve already tested and marked as safe.
Which foods to test and in which order is dependent on your
- dietary preferences
Recommended Reading: Do Ulcers Make You Bloated
You May Like: Where Does It Hurt When You Have An Ulcer
Is Bright Red Blood In My Stool Worse Than Darker Blood
The longer the blood is in your digestive tract, the darker it will typically look. This is because there are digestive chemicals in your body that naturally break down everything that moves through your digestive tract. The blood gets darker the longer its in contact with these chemicals. If your bleeding is higher up in the digestive tract, it might appear darker in the toilet. If you see bright red blood, that can mean its lower in your digestive tract or is moving through your body very quickly. While there are many benign causes of bright red bleeding, there are fewer benign causes of darker blood for this reason, dark blood may be more concerning, and warrants workup by your healthcare provider.
Are There Any Foods That Can Change The Color Of My Stool In A Similar Way To Rectal Bleeding
There are certain foods that can make your poop an unusual color. You can have green, yellow and even black stool. This can happen for a variety of reasons having too much bile during digestion, having a medical condition like inflammatory bowel disease or celiac disease, being on antibiotics, or even just eating foods with strong color pigments.
Often, blood can make your stool look very dark and almost black. Foods like black licorice, beets, dark berries and red gelatin can all make your poop look very dark. This can easily be confused for blood in your stool. If you notice very dark poop during a bowel movement, think back to what you ate recently. Theres a chance that what you ate could be the cause for the usually dark stool.
Don’t Miss: What Can Be Done For An Ulcer
Does Ulcerative Proctitis Always Progress To Ulcerative Colitis
Getting treated for ulcerative proctitis can ease symptoms and even lead to remission, meaning you may not experience symptoms for a certain period of time, but thats not quite the same thing as a cure.
Progression of the disease can happen, but its not super common, although being younger at the time of your diagnosis tends to be a risk factor for more severe disease throughout life, adds Dr. Lerrigo.
Less than 15% of people with ulcerative proctitis go on to develop full-blown ulcerative colitis, according to the National Organization for Rare Disorders . A majority of the time, people with ulcerative proctitis just have ulcerative proctitis. It doesnt necessarily progress to other areas of the colon, Dr. Yoon says. In most people with IBD, wherever the disease is located, it usually stays in that area.
Immunofluorescence And Blotting Techniques
Histological staining was performed on paraffin-embedded sections with the classical haematoxylin-eosin staining procedure. Immunofluorescence of cryosections or paraffin-embedded slides was performed as described below and recorded on either a confocal laser scanning-microscope or a standard fluorescence microscope using overnight hybridisation with primary Abs specific for -smooth muscle actin , Beta-Catenin , E-Cadherin , EpCAM , citrullinated histone H3 , MPO , C3d . Detection was performed using either biotinylated secondary Abs and TSA Fluorescein/Cy3 kits or directly labelled Alexa 488 or Alexa 555-conjugated goat anti-rat antibodies . Before examination, the nuclei were counterstained with either Hoechst 33342, propidium iodide or SYTOX Green . Autofluorescence of blood clots in paraffin-fixed sections was determined at excitation 488 nm and emission 525 nm in the absence of Alexa 488/fluorescein isothiocyanate -based immunofluorescence. Tissue-derived proteins were isolated from snap frozen samples using Mammalian Protein Extraction Reagent complete buffer and mechanical disruption using a ball mill. Protein quantification was performed using Bradford reagent . For dot blots, protein lysates were directly administered to nitrocellulose membranes. For further analysis, Western blots were performed after sodium dodecyl sulphate-polyacrylamide gel electrophoresis using ready-made gels .
You May Like: What Kind Of Yogurt Is Good For Stomach Ulcer
When To Contact A Doctor
People need to discuss any blood in the stools with their doctor, even if they have experienced it before.
A person may also wish to monitor their UC symptoms, so they know what is usual for them to experience. People can then discuss any abnormal symptoms with a healthcare professional.
If individuals have ongoing diarrhea that lasts for a couple of weeks, they can contact their doctor to discuss concerns and treatment.
The Crohnâs and Colitis Foundation advises people to seek emergency medical attention if they experience any of the following:
- inability to keep down liquids due to nausea, vomiting, or pain
- rectal bleeding with blood clots in stools
- continuous pain
Managing UC with treatment may help reduce bleeding. There are medications that may reduce inflammation in the rectum and large intestines, which may, in turn, reduce bleeding.
Anti-inflammatory medications for UC can include:
- 5-Aminosalicylic acid: Medication that may help reduce acute inflammation and causes inflammation to become inactive over time.
- Corticosteroids: A short-term treatment to help reduce inflammation.
- Immunosuppressants: These medications can help suppress the immune response that can cause inflammation. However, they may take up to 6 months to be effective.
- Biologics: For treatment of moderate to severe UC, biologics help block molecules that trigger inflammation.
Available Topical Therapies For Distal Colitis
Common therapies for the treatment of UP and UPS include 5-aminosalicylic acid and steroids. Mesalamine and other 5-ASA substances are the first-line choice in treating mild-to-moderate UC, regardless of the physical extent of disease. Mesalamine has multiple reported anti-inflammatory effects that include inhibiting leukotriene and IL-1 production, impairing TNF and NF-B transcription signaling and having antioxidant properties by acting as a free-radical scavenger. Additionally, mesalamine reduces mucosal inflammation by acting on mucosal colonic epithelial cells and infiltrating leukocytes, with its clinical efficacy therefore correlating with its local concentration in the gut.
Practice guidelines recommend using topical mesalamine agents as first line compared to topical steroids or oral aminosalicylates for the treatment of distal mild-to-moderate UC, and the combination of oral and topical aminosalicylates is more effective than either alone. In addition, practice guidelines recommend mesalamine suppositories or enemas as the preferred agents to maintain remission in distal mild-to-moderate UC. Mesalamine suppositories maintain remission in 90% of patients with mild-to-moderate UP at 1 year, while mesalamine enemas maintain remission in 72% of patients with mild-to-moderate UPS when administered every other day at 1 year.,
Also Check: Natural Way To Cure Ulcer
Limit Intake Of Animal Products
Especially meats/red meats. I have read in many articles that because many people have low stomach acidity and poor digestion, meats tend to rot in our guts, thus producing pus and contributing to inflammation . This rotting can produce more intestinal gas and overall slower digestion. I personally try to limit my meat intake to 1-2 meals per week !
What Is A Uc Flare
A UC flare is an acute worsening of the symptoms of bowel inflammation. Flares may occur weeks, months, or even years apart, with different levels of severity.
Medication, your lifestyle, diet, and other factors may contribute to flare-ups. In the same way, taking all prescribed medications, eating balanced meals, and avoiding known triggers can often help prevent flares.
Ulcerative colitis symptoms change based on the severity of a flare-up and the location of inflammation in the intestine. Symptoms often include:
- moderate to severe abdominal pain or cramps
- persistent bowel movements
Also Check: What Does A Skin Ulcer Look Like