Different Therapies Can Also Aid In Easing The Flare
Different therapies can also aid in easing the flare-up in ulcerative colitis. The frequency and intensity of lesion pain and symptoms are often lessened by use of complementary and different therapies, additionally to standard medical aid. These different therapies include yoga treatment, massage and psychotherapy. However, you must consult your doctor before taking any different medical aid, so as to avoid complications and to understand the merits and demerits.
Are There Pancolitis Complications To Be Aware Of
The most alarming short-term complication of pancolitis is a rare condition called toxic megacolon.5 Thats when your colon becomes dilated due to inflammation and eventually perforates , which can be fatal, Dr. Schwimmer says. When toxic megacolon is discovered, he says, it means the person needs surgery immediately.
One bright spot, Dr. Schwimmer says, is that toxic megacolon happens less these days because people are more aware of ulcerative colitis symptoms, and modern medications work much better to control inflammation.
A longer-term consequence of pancolitis is an increased risk of colon cancer. Still, the risk is pretty lowabout 2% for someone who has had ulcerative colitis symptoms for at least 10 years, according to an older study published in the World Journal of Gastroenterology.6 The more colon tissue you have that is inflamed, the higher your cancer risk becomes. Since pancolitis affects the whole colon, it means more opportunity for inflammation. Thats why its extremely important for people with IBD to be screened for colon cancer according to their doctors recommendation.
You May Like: Removing Colon Due To Ulcerative Colitis
What Else Should I Know
People with ulcerative colitis are at risk for colon cancer, which is related to chronic inflammation. So they should get a colonoscopy every 1-2 years, starting about 10 years after diagnosis.
Kids and teens with ulcerative colitis may feel different and not be able to do the things their friends can do, especially during flare-ups. Some struggle with a poor self-image, depression, or anxiety. They may not take their medicine or follow their diet. Its important to talk to the doctor or a mental health provider if youre concerned about your childs mood, behavior, or school performance.
Parents can help teens take on more responsibility for their health as they get older. Encourage teens to take their medicine, take care of themselves, and manage stress in positive ways. Yoga, meditation, breathing and relaxation techniques, music, art, dance, writing, or talking to a friend can help.
You also can find more information and support online at:
Read Also: Compression Stockings For Leg Ulcers
Dietary Recommendations For Ulcerative Colitis
There are different dietary recommendations for each stage of Ulcerative Colitis, active and remission. Recommendations mainly revolve around the amount of dietary fiber in your diet. During a flare its best to minimize the amount of fiber in your diet, whereas during remission fiber can be a beneficial part of your diet. Fiber is a tough nutrient for the gut to digest so during a flare, when the gut is already stressed, fiber can aggravate the symptoms of Ulcerative Colitis. Fiber also adds residue to stool, which should be avoided to allow the bowels to rest and heal. This is specifically true for insoluble fiber, which does not dissolve, and moves through your GI tract unchanged. Consuming fiber during a flare can increase bloating, gas, diarrhea, and abdominal pain, and may even lead to intestinal blockage.
Active
When UC is active, let your bowel rest as much as possible. Therefore, we recommend a low fiber, low residue diet:
- Low fiber fruit: bananas, cooked fruit, canned fruit
- Non-cruciferous vegetables: asparagus, potatoes, cucumbers, carrots
- Refined grain products: white pasta, white rice, white bread
- Lean protein: fish, chicken, lean pork, eggs, tofu
Also Check: What Causes H Pylori Ulcers
How To Ease Flare
One of the major problems of suffering with ulcerative colitis is the sudden flare-ups which are caused by the triggers of ulcerative colitis. These flare-ups will cause diarrhea and bloody stools and can lead to complications. These flare-ups would possibly occur, no matter staying on your treatment. So it is crucial to understand the way to manage and ease the flare-ups in ulcerative colitis.
Getting treatment as long as you begin experiencing the symptoms is the major step in managing ulcerative colitis. However, this could be tough and you must so acknowledge what is traditional and is not traditional. The target of remission is to make sure you are feeling well for long durations. Therefore, you must not anticipate your symptoms to be worse so as to hunt medication. Besides, you must pay additional attention once exposed to triggers of the condition, like foods and stress that provoke your symptoms.
Getting treated by your doctor is that the best approach of easing the symptoms of ulcerative colitis. However, the below mentioned tips can help you in a long way in easing flare-ups caused by ulcerative colitis:
Don’t Miss: What Foods To Avoid If You Have Ulcerative Colitis
Manage Abdominal Pains To Ease The Flare
Your abdominal pain ought to recuperate as you receive treatment. However, you must avoid taking NSAIDs medication. Also, you must avoid taking narcotics to ease your flare-ups in ulcerative colitis. However, you will be able to use spasmolytic medication, because it relaxes your gut muscles. If your ulcerative colitis pain is severe, you must ask for medical facilitate from your doctor.
How Can I Live With Chronic Ulcerative Colitis
If you are struggling with colitis or another type of irritable bowel disease, help is available at Gastroenterology Associates of Southwest Florida, PA. Our team provides compassionate, expert care to help patients suffering from these types of chronic conditions. Find out how we can help you live with chronic ulcerative colitis
Recommended Reading: Preventing Pressure Ulcers Among Wheelchair Users
When To Call Your Doctor About A Flare
Flares come with different levels of intensity. You may be able to manage a mild flare-up of symptoms on your own. But a more severe flare may be a warning sign of an ulcerative colitis complication that needs immediate attention.
Theodore J. Saclarides, MD, a colon and rectal surgeon at Rush University Medical Group in Chicago, suggests calling your doctor if you have any of these ulcerative colitis symptoms:
- Severe abdominal pain that lasts more than 24 hours
- A decrease in bowel movements along with abdominal pain
- Abdominal pain with a high fever
- Blood during a bowel movement that is too thick to see through
Editor’s Picks
What To Do If Your Flare
Stress management goes a long way in supporting your overall mental and physical health, but sometimes stress management alone just isnt enough. If youre struggling with flare-up after flare-up, we can help.
Here at Atlantic Medical Group, its our mission to help you get the relief you need so you can live the life you want. For troublesome cases that dont respond to medication, we may suggest surgery.
To explore your treatment options for Crohns disease or colitis, our Kinston or Jacksonville, North Carolina, office today. You can also visit us online to request an appointment.
You Might Also Enjoy
Recommended Reading: Can Ulcerative Colitis Cause Low Testosterone
Recommended Reading: Imodium Ulcerative Colitis Toxic Megacolon
What Causes Ulcerative Colitis Flare Ups In The First Place
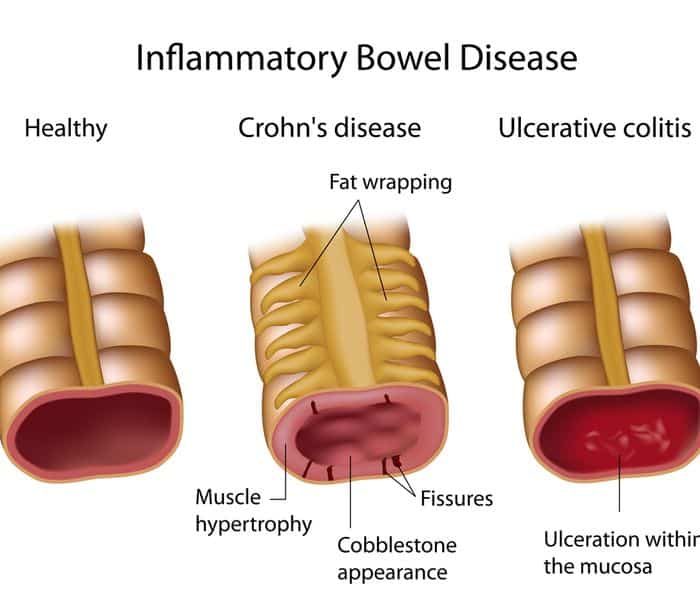
The experts arent exactly sure what causes UC, but they think its prob an autoimmune condition. Autoimmune conditions are basically what happens when the bodys defense mechanism is a little overzealous and attacks healthy tissue. Your body *means* well, but it causes inflammation.
In the case of UC, scientists think that the immune system might accidentally mistake perfectly harmless bacteria in the colon for serious threats, which causes the whole region to essentially swell up.
Though they dont know exactly what contributes to flare ups, a few possibilities include:
- Stress. According to 2016 research, being stressed out may trigger IBD flare-ups. Even though stress doesnt seem to directly cause UC, it does appear to weaken the intestinal wall and make it more vulnerable to issues. Researchers found that stress increased microbe activity in the colon and hindered the immune response.
- Diet. In a 2020 review, researchers found a correlation between diet and UC flare-ups. However, the research on exactly what triggers them just isnt there yet.
- Certain medications. Abruptly stopping medications like steroids or maintenance therapies, which slow the bods natural cortisol levels, can lead to flares and other negative side effects. Always talk to a doc before halting these drugs.
- Hormonal changes. There seems to be a link between IBD and hormonal changes in women, with some research from 2018 suggesting that UC symptoms worsen during pregnancy in particular.
How Do I Know If My Uc Has Gone Into Remission
UC doesnt have a cure. Instead, the goal of any treatment plan is to send the disease into remission.
When UC is in remission, you dont experience as many symptoms and start to feel better. If your UC medications and lifestyle changes work well for you, remission may last for months or even years. There are several different kinds of remission:
- Clinical remission: When a patient isnt experiencing symptoms and may feel better.
- Endoscopic remission: Testing of the intestinal lining shows no inflammation
- Biochemical remission: Blood and stool tests show no sign of inflammation
- Surgical remission: When UC goes into remission after surgery to treat it
- Histologic remission: When both clinical and endoscopic tests didnt show signs of UC
With UC, it can feel like life revolves around symptoms. If UC symptoms keep coming back, it can be a sign that medications arent working. Consider taking part in a clinical trial researching an investigational treatment option for people living with UC.
Don’t Miss: Is Ulcerative Colitis A Chronic Disease
Can I Treat Ibd If I Am Pregnant Or Breastfeeding
Yes, but your doctor may change the type or amount of the medicine you take. Some medicines, such as methotrexate and thalidomide, cause birth defects and other health problems and should not be taken while you are pregnant or breastfeeding.31
Before you get pregnant, make a plan with your obstetrician and gastroenterologist about the medicines you will take during and after pregnancy. Take your medicines as your doctor tells you to. If you stop taking your medicines and your symptoms come back , it may be difficult to get them back under control.31
Talk with your doctor about your medicines and breastfeeding before you give birth. You can search for your medicine in the LactMed database to find out if your medicine passes through your breastmilk and, if so, if it has any possible side effects for your nursing baby.
Also Check: How Do You Stop A Stomach Ulcer From Hurting
Keep Stress To A Minimum

With stress, your body produces higher cortisol levels, a stress hormone that can cause inflammation and UC flares.
While you may not be able to entirely stop your stressful days, there are some things you can do to help reduce your stress levels and keep yourself in a healthy state of mind. These include:
- getting enough sleep
Read Also: Off Loading Shoe For Heel Ulcer
I Take Medication Regularly Can A Flare
Unfortunately, yes. Ulcerative colitis is a chronic condition. Medications and lifestyle changes can help reduce the intensity and frequency of ulcerative colitis flare-ups, but not stop them completely.
Regular flare-ups may indicate a problem with your current treatment. If you are taking your medications as prescribed and still experiencing flare-ups, you should contact your physician who may adjust your medication or suggest other treatment options.
Coping With Stress And Ulcerative Colitis
To reduce ulcerative colitis flare-ups, it isnt always enough to take your medication and stick with your doctors treatment plan. Its can also be helpful to find ways to lower your stress level. Here are some strategies to help you manage stress:
Also Check: What Foods Cause Stomach Ulcers
What To Look For In A Meal Kit
While food triggers vary by person, Kennedy recommends looking for meals with soluble sources of fiber, which tend to be easier to digest and cause less inflammation in the digestive tract.
Things like white rice are minimally processed but still a great source of soluble fiber are great to look for, as are fruits and vegetables that either have the skin removed or can be removed during the prep process, she says.
But the general rule of thumb, says Kennedy, is that whatever meal delivery kit you choose, always opt for foods in their purest, most whole forms. The key is to find meals that use minimally processed foods, and preferably whole foods all together.
Heres a peek at the best meal delivery options for people with ulcerative colitis.
You May Like: Best Treatment For Ulcerative Colitis Flare Up
What Do Chills Feel Like With Ibd
Many people with IBD experience chills. MyCrohnsAndColitisTeam members describe this symptom in different ways. As one shared, Its like I cannot get warm.
Some people find that chills are accompanied by other symptoms, like fevers: I get flu-like episodes which come on suddenly, wrote one member. Headache, very sore neck and back, big spike in temperature, alternating sweats and chills. Its gone by the next morning. Another shared, The night sweats are horrible! My sheets are soaked every morning.
Sometimes, these chills and other flu-like symptoms are what spur a person with IBD to see a doctor in the first place. If a persons gastrointestinal symptoms are not particularly severe, fever and chills might be the first indication that something is wrong. As one member commented, Fevers and chills were part of what led to my Crohns diagnosis.
These symptoms may occur during IBD flares in some cases, even without accompanying gastrointestinal symptoms. Fever and chills are part of the symptoms of a Crohns flare-up I had, shared one member. These were the only symptoms for about a week.
However, some people with IBD experience these symptoms on a regular basis. For the past month or so, I have been getting chills while I have a bowel movement, and they are getting worse each day, one member wrote.
Read Also: Herbal Treatment For Stomach Ulcer
Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
Even On Good Days Take Your Meds
It can be easy to forget to take your medicines when you feel good. Or you might think it’s OK to skip them because you feel fine. But you need to stick with the plan your doctor prescribed to keep up those benefits.
You and your doctor will work together to decide if you need to stay on medicines to control your UC. The type of medicine will depend on how severe your UC is.
Read Also: Best Ointment For Leg Ulcers
Surgery For Managing Uc Flare
Surgery may be used to manage the symptoms of ulcerative colitis when other treatments are unable to get the disease under control . While surgery can often eliminate UC entirely, it usually requires removing the entire colon and rectum in a procedure called a total proctocolectomy. Some people with UC later have another procedure to create a J-pouch .
Stress And The Stress Response
To maintain homeostasis, a living organism must constantly adapt at a molecular, cellular, physiological, and behavioural level to environmental alterations. Stress can be defined as any threat to an organisms homeostasis. The function of the stress response is to maintain homeostasis and may involve both physiological and behavioural adaptations.
The stress response involves the complex integration of a series of interconnected regions within the brain, most notably the hypothalamus, amygdala, and hippocampus. This network receives input from both visceral and somatic afferents, and from higher cortical structures. In turn, it governs the neuroendocrine stress response via two interconnected effector pathways: the HPA axis and the autonomic nervous system .
Pathways mediating the effects of stress on the gastrointestinal tract. ACTH, adrenocorticotrophic hormone CRF, corticotrophin releasing factor.
Stress stimulates the release of CRF from the hypothalamus causing the release of adrenocorticotrophic hormone from the anterior pituitary gland. This in turn stimulates the secretion of cortisol, the principal glucocorticoid, from the adrenal cortex.
Also Check: How To Prevent Ulcers In Horses
The Role Of Peripheral Substance P
In addition to its central effects, peripheral release of SP from the ENS may have a role in stress induced increases in mucosal inflammation. Although there are no published data to show an increase in mucosal SP in response to stress, SP containing neurones are found in close association with mast cells, a cell type implicated as central in mediating stress induced permeability changes . SP has been shown to increase histamine release from mucosal mast cells in patients with IBD. Lastly, SP can act not only as a neurotransmitter but also an inflammatory cytokine in its own right, enhancing cytokine production and stimulating chemotaxis of inflammatory cells. It also increases expression of leucocyte adhesion molecules on microvascular endothelium, and of CD11b on neutrophils, facilitating leucocyte adhesion at sites of inflammation.