When To See Your Doctor
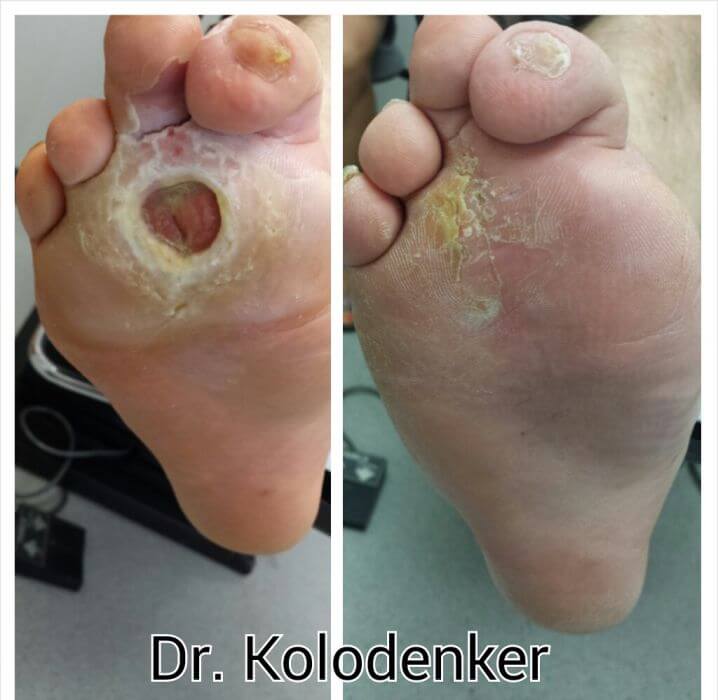
If you begin to see blackened flesh around an area of numbness, see your doctor right away to seek treatment for an infected foot ulcer. If untreated, ulcers can cause abscesses and spread to other areas on your feet and legs.
At this point, ulcers can often only be treated by surgery, amputation, or replacement of lost skin by synthetic skin substitutes.
Tell Us About The Skin
Our research, for the first time, uncovered a skin-to-brain signaling pathway. It showed that the wound itself could cause subsequent central nervous system and behavioral changes.
We, and others, have observed behavioral and cognitive changes in our patients who have chronic wounds. It is unknown if the wound causes these changes, or they are just associated findings. The idea we proposed is that when a patient gets a wound that heals right away, there is not much sustained signaling of stress to the brain. But a chronic wound keeps activating the sensory receptors for painful stimuli , sending a more continuous skin-to-brain relay. This continuous flare generates brain signals of stress that are translated into behavioral changes.
We carried out research in mice and found that skin wounds result in a relay to the brain. This relay leads to the activation of stress markers, alteration of inflammatory mediators and changes in behavior and cognition. Mice with wounds showed more signs of despair and impaired memory than those with no wounds.
We often see similar behavior in patients with chronic wounds that need daily wound care. Some seem unable to attend to their wounds despite the serious risk of losing their foot to amputation. We also observe depression and cognitive disability reflected in the perception of inability to take care of their wounds. Some even seem to be disassociated from the reality of the serious nature of this problem.
The 4 Stages Of Ulcers
When we cut or scrape our skin, our cells require adequate blood flow to that area in order to heal the wound. This blood delivers clotting agents that stop the wound from bleeding, in addition to oxygen and nutrients that allow new skin cells to grow. Wounds or sores that do not heal properly are called ulcers. Ulcers may form on our feet for a few different reasons, including narrow blood vessels or constant pressure on a particular area. Individuals with poor circulation, like smokers or diabetics, are more prone to foot ulcers.
Ulcers, like any other break in your skin, should be taken seriously because they can become infected. However, the development of an ulcer is a progressive process, and each stage comes with different signs and symptoms. Here are some brief differences between each stage:
- Stage 1: The skin becomes red and irritated where there is pressure, and does not go away when the pressure is relieved. Pain and discomfort are common.
- Stage 2: The skin is broken for the first time. The sore may look like a blister or a shallow crater, and is typically painful and tender.
- Stage 3: The ulcer penetrates even deeper into the tissue underneath the skin, possibly exposing fat cells. There may be no pain due to severe nerve or tissue damage.
- Stage 4: The sore is now so deep that it reaches the muscles, bones, or tendons. Infections and other serious complications may occur. As with a Stage 3 ulcer, it is possible that the individual feels no pain.
Don’t Miss: What Does Ulcerative Colitis Poop Look Like
What To Look For
Han says patients should be aware of gradual changes in sensations in the foot, such as tingling, burning and the feeling of pins and needles. This is known as neuropathy, which is diagnosed by visiting a specialist. Neuropathy can eventually lead to a loss of sensation, which makes the person more likely to experience repetitive foot trauma. This trauma can lead to foot injuries and ulcers that may become infected. Diabetes patients with hammertoes and bunions need to pay particular attention to shoes, as improperly fitted shoes can lead to corns and calluses that can become infected wounds.
A specialist will also be able to identify gradual loss of blood circulation to the lower extremities. This is caused by vascular damage in the lower legs due to high circulating blood sugar, leading to a buildup of plaque in major lower leg arteries and reduced blood flow. It is therefore imperative that patients with diabetes maintain stable blood sugar levels to prevent this vascular damage, and to visit a podiatrist regularly.
In most cases, through vigilance and working with a podiatrist, diabetes patients can avoid these complications. Data has shown that keeping blood sugar at normal levels reduces the risk of diabetic complications, including foot complications, by 50%. His mission, Han says, is to teach people how to recognize any subtle signs to get timely intervention so that foot infection and wounds can be prevented. My motto is, Educate, dont amputate!
Is Diabetic Foot Curable
Diabetic foot infections are a frequent clinical problem. About 50% of patients with diabetic foot infections who have foot amputations die within five years. Properly managed most can be cured, but many patients needlessly undergo amputations because of improper diagnostic and therapeutic approaches.
Also Check: Best Remedy For Stomach Ulcer
What Type Of Treatment Is Given For Leg Ulcers
The type of treatment that you are given will depend upon the severity of the ulcer. If the ulcer hasnt completely formed and a sore hasnt broken out, you may only need to use compression stockings and keep the leg elevated. This will help reduce swelling and prevent the ulcer from forming.
If an open sore has developed on the lower leg, the treatment that is recommended will be more intense. Treatment for severe ulcers includes antibiotics to fight infections, surgery to clean the wound, and dressing to protect the wound. If it is determined the ulcer is caused by venous insufficiency, your doctor may recommend you seek treatment from a vein specialist to treat the problem.
Schedule an appointment at Vein911 to discuss treatment options for leg ulcers and vein insufficiency.
About Foot And Leg Wounds And Ulcers
Most of the time, leg ulcers cause pain. If, however, you get leg ulcers due to nerve problems , you may not feel any pain. And because there is no pain, people tend to ignore the ulcer, which can lead to a leg infection.
In addition to non-healing wounds and pain, you may also have these symptoms in your legs:
- Change of color
There are several types of foot and leg wounds and ulcers.
- Venous ulcers are the most common type of foot and leg wounds and ulcers. They usually affect people with varicose veins or deep vein clots. They usually affect the inner part of the leg, above the ankle and may be irregularly shaped, reddish, and covered with yellow fibrous tissue. They also might have discharge.
- Arterial ulcers affect people who have poor circulation, high blood pressure, diabetes, or are smokers. These ulcers usually appear on the outer part of the leg and on the heels, tips of toes, and between the toes where the toes rub against each another. These ulcers vary in color and do not bleed. Often, patients report decreased pain after they dangle their feet over the edge of the bed.
- Neurotrophic ulcers/diabetic ulcers affect people who are diabetic, have nerve problems in their feet, or have had some sort of trauma to their legs or feet. These ulcers usually appear on the heels at the pressure points and may bleed. The surrounding skin is typically calloused.
- Diabetes mellitus
Recommended Reading: What Do You Do For A Stomach Ulcer
When Should I See My Doctor
See your GP if you think you might have an ulcer related to a mouth infection.
Also, see your GP if your child develops severe mouth ulcers with symptoms of general illness like:
- weight loss, stomach pain, unexplained fevers
- blood or mucus in their stool
- neck stiffness and tiredness
This may indicate conditions such as coeliac disease and inflammatory bowel disease.
Its also important to see your doctor or dentist for a mouth ulcer that lasts longer than 3 weeks and keeps coming back.
Although most mouth ulcers are harmless, a long-lasting mouth ulcer is sometimes a sign of mouth cancer. Its best to get it checked.
How Is A Diabetic Foot Ulcer Diagnosed And Treated
Your healthcare provider will ask about your symptoms and examine your foot and the ulcer. He or she may check your shoes. He or she may also send you to a podiatrist for treatment. The goal of treatment is to start healing your foot ulcer as soon as possible. The risk for infection decreases with faster healing. Do the following to help your ulcer heal:
Recommended Reading: Wound Care For Venous Leg Ulcers
Find And Treat Cuts Scrapes And Other Wounds Immediately
If you treat new wounds right away, you can start caring for them before things get bad. So as soon as you find a cut or sore:
Of course, if you dont know you have a wound, you cant treat it quickly. So if you suffer from neuropathy, keep an eye out for new wounds. Check your hands and feet daily, and dont forget to check between your toes.
Wearing white socks can help, too. If you see a red spot or a place where your sock is sticking to your skin, check your foot to see if you have a wound thats new or not healing.
How Do I Get Athletes Foot
Athletes foot commonly spreads through skin-to-skin contact or contact with a flake of skin. It spreads in areas used by large groups of people, like locker rooms, swimming pools and saunas.
It can also spread through contact with an infected surface. You can get athletes foot by sharing towels, socks or shoes with someone who has athletes foot.
You May Like: What Foods Are Good For Stomach Ulcers
What Does A Diabetic Foot Look Like
The foots appearance will provide some tell-tale signs of diabetic foot. A physical examination is, therefore, the usual starting place for doctors.
A diabetic foot may become discoloured . One or both feet may also develop:
-
A deformed appearance or abnormal shape
-
Loss of hair on the dorsum of the foot
-
Staining on socks
How Does Diabetes Increase The Risk Of Leg Ulcers

Neurotrophic ulcers, from nerve damage, affect diabetics who have high blood sugar levels.
These ulcers form most often at pressure points on the bottom of the feet. The ulcer may be discolored, pink, red, brown, or black, and is an open wound. The surrounding skin is often discolored and calloused.
Nerve damage to the legs or feet can cause symptoms such as a loss of feeling, changes to sweat glands, tingling, a burning or stinging feeling, and pain. These are predictive signs of a potential ulcer. Anyone with these symptoms should talk with a doctor and get checked.
People with diabetes should check their legs and feet frequently. Make sure there are no calluses, scrapes, or cuts. Wear good, closed footwear, never walk barefoot, and keep your legs and feet clean.
You May Like: Heel Protectors For Pressure Ulcers
Read Also: Crohn’s Disease Is Chronic Inflammation And Ulceration Of The
What Is A Foot Ulcer
Injuries happen when you least expect it. Know how to care for a foot injury if it happens to you.
Think about how often you are on your feet, running up stairs, chasing down your bus to work and wearing less-than-ideal shoes. Its probably a lot more than you realized. Your feet take a lot of abuse every day so it might not be all-too-surprising when a foot wound or ulcer occurs. From the office of your Newark and Wilmington, DE, podiatrists, Dr. Raymond Dipretoro Jr. and Dr. Aahba M. Suchak, find out what you should do to protect the health of your feet while caring for your wound.
Its true that those with peripheral neuropathy, as well as those with diabetes, are at an increased risk for developing ulcers. If youve been diagnosed with either of these conditions then you may find that ulcers dont heal as quickly as they should. Also, these ulcers are more likely to become infected. If an infection goes unnoticed it will continue to spread to the surrounding skin and even deep within the bone. Its important that you visit your Newark foot doctor immediately if you develop a foot ulcer.
What does a foot ulcer look like?
Ulcers are more likely to form on the bottoms or sides of the foot, as well as the toes. An ulcer will look like a red open wound. Some ulcers may be small and superficial while others can be rather deep. Most ulcers have a callused layer of skin that has formed around the wound.
Choice Of Outcome Measure
The primary outcome in the types of study being described should be clinically relevant. In studies of people with active ulcers, the ulcer-centered outcome of choice is healing by a fixed time or time to healing. An alternative measure is to document change in cross-sectional area , and this may not always be easily accomplished because of the curved surfaces of the foot . As change in early-phase cross-sectional area has been shown to correlate with later healing , the chosen primary outcome may be a relative short-term reduction in ulcer area. It is less precise as a measure but can potentially allow exploratory studies to be conducted more quickly.
But when expressed in person-centered termswhich is generally preferablethe outcome should ideally refer not just to the healing of the index ulcer but to the patient being ulcer free . If such a person-centered outcome measure is adopted, it might be expressed in terms of time to being ulcer free, being ulcer free after a fixed interval , or ulcer-free days from the date of randomization to a fixed point . The use of ulcer-free days as a primary outcome is also valuable in studies of attempts to reduce ulcer recurrence, just as antibiotic-free days may be used in studies designed to prevent or treat infection and amputation-free survival in people with limb-threatening PAD.
You May Like: What Vegetables Are Good For Ulcerative Colitis
Foot Ulcer Prevention Tips You Should Consider
People with diabetes and others who know they are at risk for foot ulcers should examine their feet daily and practice good foot hygiene.
Those with foot ulcers should keep the wound clean and dry, change the dressing as directed, take prescribed medications, maintain a healthy diet, and wear appropriate shoes.
Medical References:
When You Need More Treatment
If your wound doesnât heal in about a month or becomes an infection that spreads to the bone, you may need other treatments. These can include surgery and hyperbolic oxygen therapy, which involves breathing pure oxygen in a special room in order to help your body heal.
If your ulcer develops gangrene and your tissue dies, your doctor may have to amputate that area of your body.
Don’t Miss: How To Tell If I Have Stomach Ulcer
Wound Care And Dressings
Care for your wound as instructed by your provider. Other instructions may include:
- Keep your blood sugar level under good control. This helps you heal faster and helps your body fight infections.
- Keep the ulcer clean and bandaged.
- Cleanse the wound daily, using a wound dressing or bandage.
- Try to reduce pressure on the healing ulcer.
- Do not walk barefoot unless your provider tells you it is OK.
Arterial Foot Ulcers Vs Diabetic Foot Ulcers: How Are They Different
We want you to understand that having foot sores that dont heal doesnt necessarily mean that you have PAD. Several underlying health conditions can also cause decreased healing in the feet, including diabetes.
Individuals with diabetes can develop diabetic foot ulcers, which are different from arterial ulcers. This type of ulcer usually occurs due to neuropathy , which can desensitize feeling in the foot. According to Dermatology Advisor, diabetic foot ulcers tend to develop on the bottom of the foot, most commonly on the first metatarsal joint or the heel of the foot. They are not always painful in some cases, patients are completely unaware that open wounds are present.
Arterial foot ulcers develop due to poor circulation from peripheral artery disease. Although arterial insufficiency ulcers can appear anywhere on the lower extremities, they most commonly occur on the toes, heels, and ankles. They are usually painful and can be yellow, brown, gray, or black.
It is important to know that diabetes is a known risk factor for peripheral artery disease. Diabetic foot ulcers can be further complicated by the presence of vascular disease. If you have diabetes, we suggest working closely with your doctor to properly manage it. This may also help reduce your risk of developing vascular disease.
Read Also: How To Know If You Have A Bleeding Ulcer
Causes Of Canker Sores
- Canker sores have many causes.
- Minor injuries to the mouth can trigger a canker sore. Examples are from a rough food or a hard toothbrush. Biting oneself while chewing can start one.
- Food allergies or irritants may also be a trigger.
- Vitamin deficiencies can also be a cause. A vitamin deficiency can occur if your child is a picky eater.
- Canker sores can run in families .
- Often, the cause is unknown.
Other Types Of Leg Ulcer

Other common types of leg ulcer include:
- arterial leg ulcers caused by poor blood circulation in the arteries
- diabetic leg ulcers caused by the high blood sugar associated with diabetes
- vasculitic leg ulcers associated with chronic inflammatory disorders such as rheumatoid arthritis and lupus
- traumatic leg ulcers caused by injury to the leg
- malignant leg ulcers caused by a tumour of the skin of the leg
Most ulcers caused by artery disease or diabetes occur on the foot rather than the leg.
Page last reviewed: 11 January 2019 Next review due: 11 January 2022
Read Also: Diabetic Foot Ulcer Dressing Guidelines