Foods Rich In Sulfur And Sulfites
Foods like beer, wine, shellfish, some dried fruits, white bread, and cured meats containsulfur, producing excess gas in the colon. Even without these foods, UC patients produce more hydrogen sulfide than usual, and they have difficulty breaking the gas down due to inflammation of the colonic wall. Hence, ingesting more foods with sulfur causes more damage to the colon.
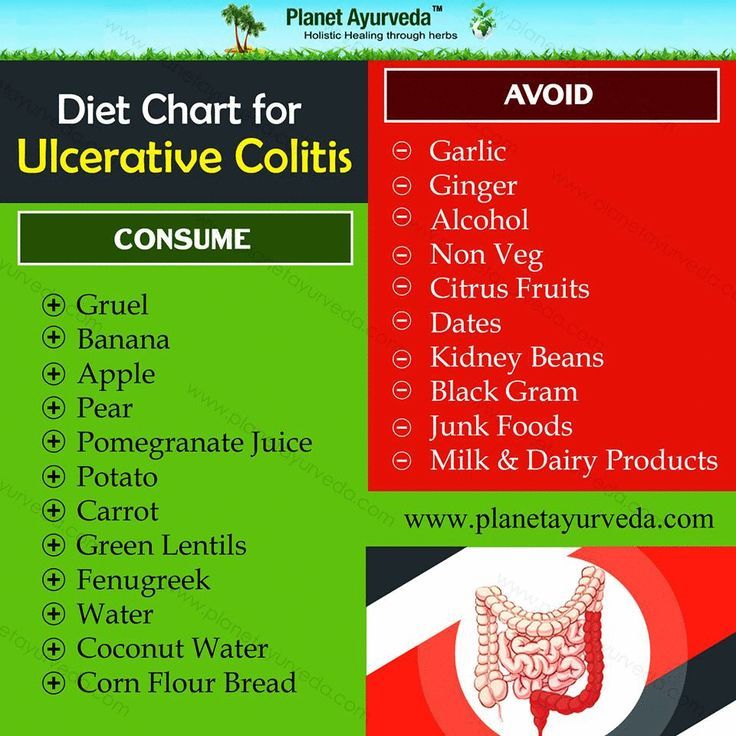
Foods To Avoid During Ulcerative Colitis Flares
During a flare, ulcerative colitis symptoms become more severe, and certain foods can worsen them further.
Following these guidelines can keep you away from the most common food triggers during UC flares:
- Avoid high-fiber foods, such as whole grains, dried fruit, and raw vegetables or vegetables with tough skin. Make sure to cook vegetables thoroughly, and avoid vegetables with seeds.
- Avoid cruciferous vegetables that produce gas, such as broccoli, cauliflower, and Brussels sprouts.
- Avoid spicy foods.
- Avoid caffeine in coffee, tea, and other beverages. This can contribute to diarrhea.
- Avoid whole nuts and seeds. Choose smooth nut butters. Almond butter, peanut butter, cashew butter, and sunflower butter are all great choices.
- Avoid fried foods, fatty foods, and highly processed foods.
- Avoid high-sugar foods, like fruit juice and baked goods. These can contribute to diarrhea.
Some members of MyCrohnsAndColitisTeam learned about their food triggers the hard way. Last time I drank coffee, I felt every centimeter of my intestines. Big no for me, shared one member. Another member communicated her hard-won personal rule very clearly: No sugar, and I mean NO SUGAR AT ALL!
Replace Red Meat With Salmon
Next time you’re thinking steak, make it salmon, or another meaty fish rich in omega-3 fatty acids like tuna, mackerel, or herring, recommends Rogers. Consumption of red and processed meats are tied to a worsening of UC symptoms, per the IOIBD’s most recent guidelines, while omega-3 fatty acids from seafood seem to help support lower levels of inflammation. Try a roasted salmon filet with a baked potato and sauteed spinach grilled, flaked tuna as a taco filling or use either fish to make burgers in lieu of the usual hamburger.
You May Like: Ulcerative Colitis How Much Blood Is Too Much
What To Do During A Flare
Medications are used to manage flares and induce remission as quickly as possible.
Doctors may prescribe a corticosteroid , antibiotic, 5-aminosalicylate, immunomodulator or biologic.
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day .
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 2530 grams.
- Drink plenty of fluids to avoid dehydration.
Quick Tips For Nausea
If youre really having trouble keeping things down, here are a few of my tips:
- Be cautious about how much volume youre putting in and what ingredients you may be substituting. If youâre youâre questioning if youâll be able to keep it down at the rate that its dissolving, or wondering if it may just come right back up and leave you back to where you started ⦠consider this.
- Iâve heard of others using cupcake wrappers to poke through and hold the contents that melt if not consumed quickly enough. Cool, huh? But, eating faster doesnât mean better if youâre vomiting. If you find this to be true, consider putting less in each cube.
- Major nausea hack: In the past, Iâve taken a couple of tablespoons of the purée and placed pureed contents into one corner of a few small Ziploc bags. Freeze that, then cut off a very small tip of the corner of the bag, so when youâre ready to eat one, you can consume it at a slower rate.
Dont Miss: Early Symptoms Of Stomach Ulcer
You May Like: Will Diabetic Foot Ulcers Ever Heal
Foods That May Fight Uc
Some research shows that certain nutrients may help fight the irritation and swelling in your gut caused by UC. Scientists have studied how linoleic acid affects people with the condition. Although everyone needs this “good” fat, donât overdo it, since there is some evidence it may play a role in inflammation if you get too much.
Other studies show that an omega-3 fatty acid called EPA may fight inflammation. This is another âgoodâ fat that blocks certain chemicals in your body called leukotrienes. Fish oil is a good source of EPA. In some studies, folks with UC saw some benefits when they took high doses. Many people, though, didn’t like the fishy taste. There is also some evidence that adding fish oil to aminosalicylates may be helpful, but this isnât proven. DHA is another omega-3 found in fish oil that can fight inflammation and is used by some people with UC.
Some research also shows that yogurt with gut-healthy bacteria, called probiotics, eases inflammation. Scientists are still studying how they may help people with UC and similar conditions. Some people also believe that a diet low in FODMAPs — a type of highly-fermentable carbs found in meats, fruits, dairy, and lots of other foods — may help ease UC symptoms. But the evidence is unclear if it does. And without close monitoring, any diet that restricts certain foods may lead to poor nutrition and other problems.
Show Sources
Is Ulcerative Colitis A Genetic Condition
One of the most significant risk factors for Ulcerative Colitis is family history. Scientists believe that individuals inherit genes that put them at risk for Ulcerative Colitis. At some point in life, environmental factors trigger the immune systems to attack the large intestine and the disease sets in.
Researchers estimate that between 10 and 25 percent of people with Ulcerative Colitis have an immediate family member with IDB. It is also believed that if one parent of a child has IBD, the child has a two percent risk of also developing IBD at some point in life. If both parents have IBD the risk for the child increases. Ulcerative Colitis is also more prominent in individuals who have more distant relatives that suffer from Ulcerative Colitis. Research also indicates that in individuals with a family history of Ulcerative Colitis, the age of disease onset tends to be earlier.
More specifically, studies have been conducted on both identical and fraternal twins who have Ulcerative Colitis. If one twin has Ulcerative Colitis, their identical twin will also have Ulcerative Colitis about sixteen percent of the time, while their fraternal twin will have Ulcerative Colitis about four percent of the time.
Read Also: All Symptoms Of Ulcerative Colitis
Read Also: How To Prevent Hospital Acquired Pressure Ulcers
Eating When You Are In Remission
While theres no cure for UC, you may experience periods of remission. During this time, youll be symptom-free and your UC wont interfere with your daily life.
Theres no definitive way to avoid flare-ups forever, but you can prolong your remission periods by maintaining a diverse and nutrient-rich diet that does not include trigger foods.
To stay symptom-free, it may be helpful to follow one of the diets that other individuals with UC find successful, as well as introduce new foods slowly and stay hydrated.
However, its important to consult with your doctor or dietician before making any changes to your diet.
Some foods that may help keep you feeling good and hydrated during remission
When Should You See A Doctor About Ulcerative Colitis Food Triggers
According to Dr. Schwimmer, seeing a doctor at the first sign of ulcerative colitis symptoms is your safest bet, especially if youve never been formally diagnosed. Concerning, unexplained symptoms like bloody stool, diarrhea, and abdominal cramping shouldnt be ignored, because even if its not ulcerative colitis, you might be dealing with something else that needs proper treatment.
After youve been diagnosed, your doctor might recommend making diet adjustments as a part of your ulcerative colitis treatment plan. But ultimately, FDA-approved medications, which help control the inflammation that sets off GI pain, are going to be the main course of treatment that your doctor suggests for the long haul of this chronic condition.
There is no secret treatment for inflammatory bowel disease. Everybodys looking for the secret pills. What diet can I follow? What supplement can I take? What probiotic can I take? Unfortunately, it just doesn’t exist, Dr. Schwimmer says. But the medicines we have work and they work better than anything else.
Thats why doctors who specialize in IBD caution that self-treatment with diet is not enough. If you arent working within the framework of a plan that includes proven, FDA-approved medication, you are at a higher risk of complications from your ulcerative colitis, including malnutrition.
You May Like: History Of Ulcerative Colitis Icd 10
The Nutritional Impact Of Uc
Changes in diet and nutrition are one part of a multifaceted approach for treating ulcerative colitis and other IBD conditions. Your doctor also will likely prescribe medication. In more severe cases, surgery may be needed, to repair or remove damaged portions of the colon.
Malnutrition, dehydration, and weight loss are major health risks of UC. When the colon becomes inflamed and ulcerated, its less able to absorb fluids and nutrients needed to help sustain your body.
Diarrhea, a symptom of UC, also increases loss of fluids and nutrients, such as sodium, potassium, magnesium, phosphorus, and zinc.
In severe cases, people with UC may need IV fluids to replace these lost nutrients and fluids.
Other UC symptoms, such as abdominal pain and nausea, can further rob you of nutrition as they reduce your appetite, so you consume fewer calories and nutrients.
Other Foods Are Known Uc Harmers
On the other hand? Things like full-fat dairy, red or processed meats, unhealthy fats, and fried or greasy meals are thought to have the opposite effect, per recent guidance developed by the International Organization for the Study of Inflammatory Bowel Diseases . If trying to get more of the good stuff and less of the bad seems overwhelming, read on. Here, Stein and Rogers share some of their favorite UC-friendly food strategies that can reduce your symptoms and even make it easier to manage your UC long-term.
You May Like: Do Probiotics Help Ulcerative Colitis
Ulcerative Colitis Diets You Might Try
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
How Can I Track Foods That Cause Flare
The Crohn’s and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohn’s and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
You May Like: Best Protein For Ulcerative Colitis
Carbonated Beverages May Increase Abdominal Pain
Fizzy drinks may cause gas or bloating in some people, possibly leading to increased abdominal discomfort. Many soft drinks or carbonated energy drinks also contain caffeine, which can stimulate the intestines and worsen diarrhea, according to Mayo Clinic. Drinking sugary soft drinks can contribute to obesity as well, which raises the risk of heart disease and other health problems.
An analysis of drinks published in May 2019 in the journal Medicine found that a high intake of soft drinks was associated with an increased risk of developing Crohns disease, while a high intake of tea was associated with a lower risk of the inflammatory bowel disease. For a refreshing beverage, choose fruit-infused water or herbal iced teas.
Eating With A Stricture
If you have a stricture , you may need to change what you eat to help prevent the intestine getting blocked.You might be advised to avoid foods that could block the intestine, such as:
If you have a severe stricture, you may only be able to eat very soft or liquid foods.Its important to speak to a dietitian to make sure youre eating a healthy, balanced diet. In some cases, they may recommend a vitamin and mineral supplement.
Also Check: How To Gain Weight With Ulcerative Colitis
What Is Ulcerative Colitis
Ulcerative colitis is a chronically inflamed colon. The colon is at the end of the digestive tract and connects to the rectum. The colon is hugely important for absorbing nutrition and eliminating waste in the body. When it becomes chronically inflamed, the cause may be ulcerative colitis.
Colitis is interrelated to another disease called Crohns. A person can have both Crohns and ulcerative colitis as part of an overarching diagnosis of irritable bowel disease . Colitis and Crohns are both long-term and chronic disorders affecting the gastrointestinal tract. Colitis, however, centers in the lining of the large bowel, or colon. Several diagnoses can be made to pinpoint the type of colitis you may have:
- Left-sided colitis is inflammation that starts in the rectum and extends to the left colon
- Pancolitis, also called universal colitis, affects the entire organ
- Fulminant colitis is a rare but serious form of pancolitis
- Proctosigmoiditis inflames the rectum and a short section of the nearby colon called the sigmoid colon
- Ulcerative proctitis is a type of inflammation that only affects the rectum
Keeping An Ulcerative Colitis Diary: 5 Tips For Top Results
Whatever approach you choose, these strategies are worth remembering:
⢠Write down everything you eat. A food-and-symptom diary only works if you record everything. The more accurate your inventory, the more reliable the insights you’ll get. Your dietitian may also want to review your food diary to make sure you’re eating a well-balanced diet that provides all the nutrients you need, so an accurate record is crucial.
⢠Record amounts and how foods are prepared. Some people are bothered by large servings of chocolate but untroubled by a bite-sized piece. Fried chicken may exacerbate symptoms while grilled chicken goes down fine. Write down not just what you ate but how much and how it was prepared.
⢠Keep track of your ulcerative colitis symptoms. Some people use a scale of 1 to 10 to describe how they’re feeling. Others prefer written notes. Use whatever system helps you be as accurate as possible.
⢠Don’t be afraid to experiment. While keeping a food-and-symptom diary, try small amounts of foods that you tend to avoid for fear they’ll cause problems. That way you can test whether they really do spell trouble for you. If a large serving of something bothers you, try cutting the serving size in half. Remember that your goal is to eat as wide a variety of foods as you can.
Recommended Reading: How To Know You Have A Ulcer
What Foods Should I Not Eat When I Am Having An Ulcerative Colitis Flare
Certain foods can exacerbate or aggravate an UC flare and should be avoided. They are more likely to trigger cramping, bloating, and/or diarrhea and are also not recommended in people diagnosed with a stricture, which is a narrowing of the intestine caused by inflammation or scar tissue, or in those who have had recent surgery. Examples include:
- Foods high in insoluble fiber that are hard to digest, such as seeds, raw green vegetables , whole nuts, whole grains, or fruits with a skin
- Lactose, which is milk sugar found in dairy products, milk, cream, cream cheese, and soft cheeses
- Non-absorbable sugars such as sorbitol, mannitol, and other sugar alcohols that are typically found in sugar-free gum, candy, ice cream, and certain types of fruits and juices such as pear, peach, and prune juice
- Sugary foods such as candy, pastries, and juices
- High-fat foods such as butter or margarine, coconut oil, or fatty, fried, or greasy food
- Alcohol such as beer, wine, or spirits
- Caffeinated drinks such as coffee or energy drinks
How Can Diet Help With My Symptoms
Making changes to your diet may help you manage some common symptoms of Crohns and Colitis, such as loose and runny stools, dehydration, bloating, wind, constipation, weight loss, tiredness, nausea and vomiting and pain. While changing your diet can help you manage your symptoms, it doesnt replace the medical treatment suggested by your IBD team.
Loose and runny stools
A common symptom of Crohns and Colitis is loose and runny stools, called diarrhoea. For some people, their diet has no effect on their diarrhoea. Others find that avoiding certain foods helps. You could use the food diary above to help you find out which foods might be causing your symptoms. Foods which sometimes make diarrhoea worse include spicy or fatty foods, high fibre foods, foods containing gluten and dairy foods. Drinks containing caffeine, sweeteners or alcohol can also make diarrhoea worse.Your IBD team or dietitian can advise you on how to manage your diarrhoea. They will want to make sure youre eating and drinking enough to get all the nutrients you need and to stay hydrated. In some cases, they may recommend medicines to help.Our guide Diarrhoea and constipation has more information about what causes diarrhoea and possible treatments.
Dehydration
If your body doesnt have enough water, you can become dehydrated. This might happen if you dont drink enough fluids or if your body loses too much fluid, for example, if you have diarrhoea or vomiting.You may be more likely to get dehydrated if:
Recommended Reading: Can You Eat Pizza With Ulcerative Colitis