Some Ingredients In Supplements
Some supplements are very beneficial for people with UC. These include calcium, folic acid, and iron. However, some ingredients in supplements may worsen the symptoms of UC.
According to the Crohns and Colitis Foundation, people should avoid supplements that contain:
All of these may aggravate a persons UC symptoms, particularly during a flare-up.
The Crohns and Colitis Foundation also adds that people should avoid taking any supplements on an empty stomach.
A person should check with a medical professional before taking any supplements, including herbal supplements, over-the-counter medications, and complementary therapies.
Risk Factors Signs And Symptoms Of Ulcerative Colitis
Ulcerative colitis occurs due to an immune system dysfunction. Normally, the immune system safeguards the body against disease-causing bacteria by sending fighter cells to counter-attack pathogens. However, people develop UC when the immune system mistakes food, beneficial bacteria, and cells lining the colon for intruders. As a result, the white blood cells meant to protect you attack the colonic walls, resulting in inflammation and ulcers.
Ulcerative colitis is an idiopathic inflammatory condition because doctors dont know why people experience on and off UC symptoms. Nonetheless, UC is associated with various risk factors that include:
- Age UC prevalence rate is high among individuals of 15-30 years and those older than 65.
- Ethnicity The risk of developing UC is highest among people of Ashkenazi Jewish descent.
- Family history If you have a close relative with UC, your chances of developing the condition are 30% and above.
Follow A Recommended Corticosteroid Dose
Corticosteroids are common treatments for UC flare-ups. It is important that a person follows their exact dosage over time.
Doctors may prescribe a higher dose that reduces gradually over time.
This is because if a person takes too much of a corticosteroid over a long period, it can put them at a greater risk of a number of problems, including heart problems and mood disorders.
It is important that a person gradually tapers off their use of corticosteroids. This is because instantly or rapidly stopping the course may harm their body.
Recommended Reading: What Causes Peptic Stomach Ulcers
Reintroducing Your Usual Diet
Your IBD team and dietitian will give you information about returning to your usual diet after youve finished enteral nutrition. They may suggest reintroducing foods slowly so you can see if any foods affect your symptoms and to help you feel more confident about eating again. There are three ways of doing this:
- the elimination diet after excluding all foods, they are reintroduced one by one every few days, to see if they cause problems
- the Royal Free method this is similar to the elimination diet but foods are reintroduced more quickly, over a period of days rather than weeks
- the LOFFLEX diet this excludes foods high in fat and fibre.
There isnt much evidence to show how well these diets work, or whether one works better than another. Your dietitian will explain the benefits and risks of all your options.
Ive found that you have to be very careful on the internet as there are many websites claiming to cure IBD through untested diets and supplements which are not properly regulated and could be harmful and also expensive.
Zaineb
This is an extreme form of low carbohydrate diet that limits:
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Also Check: Dac Cool Gut For Ulcers
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
Eating During A Flare
Even when you try your best, flare-ups still happen. They typically cause all the awful symptoms of ulcerative colitis like fatigue, frequent diarrhea, and rectal bleeding. During this time its important to understand which foods make your symptoms worse while also remembering to still nourish your body with essential nutrients.
Its also possible for ulcerative colitis sufferers to experience periods of remission, in which youll be symptom-free. While there is no proven way to prevent flare-ups from returning, you may be able to help prolong the remission period by avoiding trigger foods and eating a healthy diet. Its also important to work closely with your doctor and dietician to develop a healthy eating plan for you.
Also Check: How Can You Tell You Have An Ulcer
The Worst Foods For Those With Ulcerative Colitis
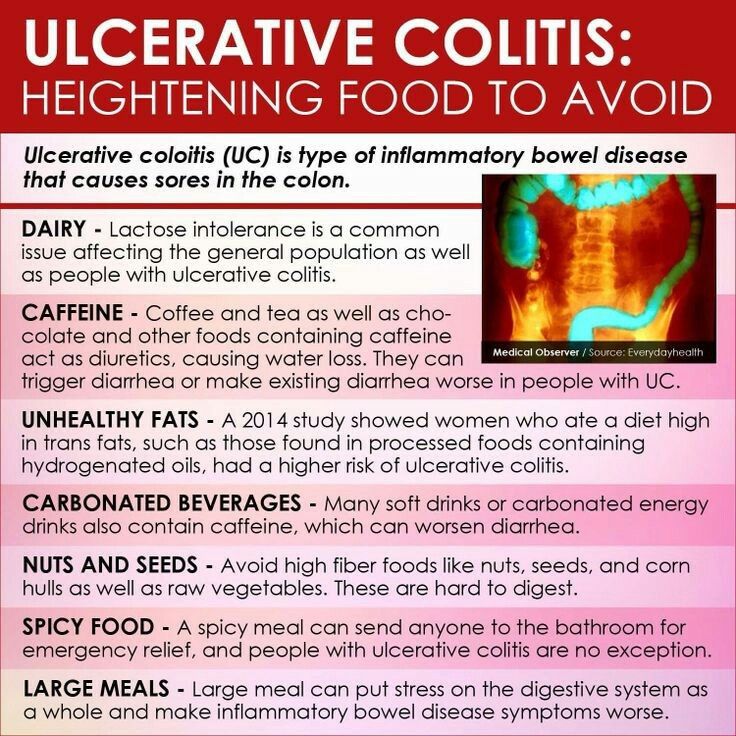
Ulcerative colitis is an inflammatory chronic disease of the colon and rectum where ulcers develop inside the lining of the large intestine. It is an inflammatory bowel disease along with Crohns Disease which causes a multitude of painful and unpleasant symptoms. Since dietary habits can contribute to ulcerative colitis symptoms, lets look at the worst foods for those with ulcerative colitis.
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Don’t Miss: Can Candida Cause Ulcerative Colitis
How Is Ulcerative Colitis Treated
Answered by Dr. Howard E. LeWine
M.D. Chief Medical Editor, Harvard Health Publishing · 40 years of experience · USA
Medications are very effective for improving the symptoms of ulcerative colitis. Most of the medications used work by preventing inflammation in the intestine. Depending on the location and severity of the colitis, the medications may be as an enema or suppository, pills by mouth, home injections or periodic intravenous injections at a medical site.
Learn more about ulcerative colitis: See the causes, symptoms, treatment options and more.
Disclaimer: This is for information purpose only, and should not be considered as a substitute for medical expertise. These are opinions from an external panel of individual doctors, and not to be considered as opinion of Microsoft. Please seek professional help regarding any health conditions or concerns.
You May Like: Wound Dressing For Stage 2 Pressure Ulcer
Back Up: What Is Ulcerative Colitis Exactly
Ulcerative colitis is a type of inflammatory bowel disease that causes ulcers and sores in the lower quarter to third of your digestive tract. Typically, these ulcers are found in your rectum or in the inner lining of your lower intestine . This can cause bloody diarrhea, the most common symptom of ulcerative colitis, but you might also experience things like abdominal cramping, constipation, and a general sense of fatigue. Weight loss and a loss of appetite can also crop up, per the U.S. National Library of Medicine.
Diana Whitehead, M.D., director of the Inflammatory Bowel Disease Center at the Greater Baltimore Medical Center, explains that though ulcerative colitis has a strong genetic component, symptoms are often set off by a triggering event that activates inflammation in the lower intestine. Basically, your immune system is not doing what it should do, which is to protect you, but its gone kind of into overdrive, Dr. Whitehead says. In other words, even though the exact causes of ulcerative colitis arent fully understood, experts consider it to be an autoimmune condition thats set off by this overreaction in the gut.
Dont Miss: Wet To Dry Dressing For Pressure Ulcers
Also Check: How To Stop A Bleeding Stomach Ulcer
Tips To Treat Episodes Of Ulcerative Colitis
To properly treat an episode of ulcerative colitis, its extremely important that you receive a medical diagnosis. A health professional can determine if the symptoms you experience are due to ulcerative colitis or other problems like Crohns disease or diverticulosis.
The medical examination might include blood tests, stool samples, a barium enema, or colonoscopy, among others. Then, if the symptoms correspond to an episode of ulcerative colitis, the doctor might suggest some medicine and lifestyle changes. In the most serious cases, surgery might be necessary.
Generally, there are some tips that can help prevent and treat these outbreaks. They are simple measures that you can take in your daily life, both in times of remission and during episodes. Put them in practice!
Drinking In Moderation Is Fine If You Have Uc
If you like to have a glass of wine or beer with family and friends over a heated fall football match or a festive holiday dinner, you probably dont need to worry about your UC symptoms flaring. Theres no evidence that alcohol increases UC flares, Dr. Hong says . If boozing is a trigger for you, stick to alcohol-free versions of your top tipples.
Read Also: Are Oranges Bad For Ulcerative Colitis
Are Beets Good For The Gut
May Improve Digestive Health It has been linked to many health benefits, including improved digestion. One cup of beetroot contains 3.4 grams of fiber, making beets a good fiber source . Fiber bypasses digestion and heads down to the colon, where it either feeds the friendly gut bacteria or adds bulk to stool.
Recommended Reading: Will Ulcer Cause Back Pain
Maintain A Balanced Diet
Like many digestive disorders, what works for some may not work for others. It can be difficult to say exactly what should be avoided for each person. However, those in the know agree that if you are living with UC it is extremely important that you drink plenty of liquids and maintain a healthy, balanced diet.
Don’t Miss: How To Manage Ulcer Pain
What Are The Basics Of A Healthy Diet For People With Uc
This whole UC situation would be a lot easier if it came with an instruction manual for eating. But even though were not quite as lucky as that, there are plenty of to help you along the way.
Case in point: Doctors and dietitians generally discourage people with UC from adopting fad diets like Keto or Paleo, which may do more harm than good because you may not get the nutrients you needor you may get too much of what you dont need. On the what-you-can-eat side, they generally recommend following a plant-based, Mediterranean diet . But what you eat during a flare and what you eat the rest of the time likely wont be exactly the same. Here are some things to keep in mind:
Foods That May Help Avoid Flares
Some healthful foods may have anti-inflammatory effects that can help control the underlying inflammation of Crohns disease and ulcerative colitis. Many of these foods are unprocessed. They also tend to have lots of color. Some of the substances that give fruits and vegetables their color have anti-inflammatory and other healthful effects.
Eating this way helps support anti-inflammatory pathways in our bodies, which may be very helpful when managing an inflammatory disease like IBD. In addition, if you are not flaring, eating healthful foods will also help you avoid any deficiencies in vitamins, minerals, and other nutrients.
You May Like: How Does Someone Get Ulcerative Colitis
Pick A Less Acidic Alternative To Tomatoes
Whether theyre juiced, cooked, or stewed, tomatoes can be notoriously hard on your gut. Not only are tomatoes acidic, which can irritate your intestinal lining, but their seeds can also be hard to digest.
If youre not in the middle of a flare, you may be able to indulge in an occasional helping of tomato sauce perhaps a quarter cup, suggests Craggs-Dino.
Do tomatoes trigger your UC symptoms? Make a sauce or bisque-style soup from pureed cooked squash instead.
Read Also: What Can You Put On Mouth Ulcers
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Also Check: Best Dressing For Stage 2 Pressure Ulcer On Buttocks
Be Mindful Of Portions
Eating a big plate of delicious food can be tempting but its important to be mindful of your portions whether you have ulcerative colitis or not. Not only can overeating lead to weight gain, but it can also put stress on your digestive system, making your symptoms worse, explains Everyday Health.
Instead of eating larger portions, focus on smaller, more frequent meals. This will help put less stress on your digestion and make it easier for your body to digest the food youre eating. The source recommends eating five or six smaller meals every 2- to 3 hours.
Eat These Foods To Avoid A Flare Up Of Ulcerative Colitis
The Heal Your Gut Cookbook: Nutrient-Dense Recipes for Intestinal Health Using the GAPS Diet by Hilary Boynton contains more than 200 easy, straightforward recipes that restore the balance between beneficial and pathogenic intestinal bacteria. These recipes contains foods that are natural remedies for painful ulcerative colitis symptoms by sealing the gut through the elimination of grains, processed foods, and refined sugars.
Gut and Psychology Syndrome refers to disorders, including ADD/ADHD, autism, addictions, depression, and obsessive-compulsive disorder, stemming from or exacerbated by leaky gut and dysbiosis. GAPS also refers to chronic gut-related physical conditions, including celiac disease, rheumatoid arthritis, diabetes type one, and Crohns disease, as well as asthma, eczema, allergies, and thyroid disorders.
You May Like: How Do They Check For Ulcers
How Are Nutrition And Inflammation Connected
The theory behind the anti-inflammatory diet is that by avoiding certain inflammation-triggering foods processed foods, high-sugar foods, fried foods, processed red meat and saturated fats you lower the amount of chronic inflammation in the body and therefore lower your risk of developing those problems or exacerbating any you already have.
The foods youre allowed to eat on the diet fruits, vegetables, omega-3 fatty acids particularly those found in fish, nuts and olive oil are foods we see over and over again in nutrition research as being associated with fewer health problems and generally longer, healthier living, explained Deirdre K. Tobias, ScD, associate epidemiologist at Brigham and Womens Hospital and assistant professor at Harvard Medical School and Harvard T.H. Chan School of Public Health.
Swap Wheat Bran With Oatmeal Or Corn Flakes
Wheat bran and bran flakes are high in insoluble fiber, which passes through the gut undigested. Heart-healthy oatmeal, though, is a good source of soluble fiber, so its good to eat, even during a flare, says Cavagnaro. Plain, less processed oats are better. Avoid prepared oatmeal packs.
A study published in March 2019 in the journal Frontiers in Immunology reported that short-chain fatty acids, such as butyrate, which are produced by the good bacteria in the GI tract, have an anti-inflammatory effect in the intestines. You can find foods that produce short-chain fatty acids in whole grains, fruits, and vegetables.
Other cereals worth trying are cornflakes, Cheerios, and Rice Krispies. For hot cereals other than oatmeal, try grits or Cream of Wheat.
Donât Miss: How Do You Heal Leg Ulcers
Don’t Miss: What Can I Do To Relieve Stomach Ulcer Pain
When Should You See A Doctor About Ulcerative Colitis Food Triggers
According to Dr. Schwimmer, seeing a doctor at the first sign of ulcerative colitis symptoms is your safest bet, especially if youve never been formally diagnosed. Concerning, unexplained symptoms like bloody stool, diarrhea, and abdominal cramping shouldnt be ignored, because even if its not ulcerative colitis, you might be dealing with something else that needs proper treatment.
After youve been diagnosed, your doctor might recommend making diet adjustments as a part of your ulcerative colitis treatment plan. But ultimately, FDA-approved medications, which help control the inflammation that sets off GI pain, are going to be the main course of treatment that your doctor suggests for the long haul of this chronic condition.
There is no secret treatment for inflammatory bowel disease. Everybodys looking for the secret pills. What diet can I follow? What supplement can I take? What probiotic can I take? Unfortunately, it just doesnt exist, Dr. Schwimmer says. But the medicines we have work and they work better than anything else.
Thats why doctors who specialize in IBD caution that self-treatment with diet is not enough. If you arent working within the framework of a plan that includes proven, FDA-approved medication, you are at a higher risk of complications from your ulcerative colitis, including malnutrition.