Preoperative Optimisation Of Refractory Moderate
Correction of altered body composition and nutrition imbalances is advised preoperatively, despite limited evidence . There is no evidence to support routine enteral or parenteral nutrition to improve the surgical outcomes of patients with UC . Iron supplementation is recommended when iron-deficiency anaemia is present
Nutritional alterations predict poor postoperative outcomes and mortality and affect QoL., Routine perioperative assessment by a nutritionist should be considered in IBD patients in remission, as part of multidisciplinary management. Even if current evidence is limited, it is advisable to correct undernutrition or overnutrition., No data support routine perioperative administration of enteral or parenteral nutrition. Delaying surgery by 714 days should be considered in patients with malnutrition. High-quality evidence suggests that iron supplementation is recommended when iron deficiency is present, with the goal of normalising haemoglobin levels and iron stores.,
Low-quality studies reported that patients who have received > 20 mg prednisolone for > 6 weeks are at 5-fold increased risk of infectious and short-term pouch-specific complications. Steroids should be weaned before surgery if this is not possible, pouch construction should be postponed. Thiopurines or cyclosporine do not increase the risk of postoperative complications.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Meet Your Uc Surgeons And Team
Most people who have surgery for ulcerative colitis are referred from their gastroenterologist. The surgeon that will complete the surgery is most often a colorectal surgeon, who specializes in surgery of the digestive system.
An enterostomal therapy nurse will be helpful before and after surgery to place an ileostomy. An ET nurse will help decide where the stoma will be placed and will make suggestions on which type of appliance will work best.
Don’t Miss: How Do You Prevent Pressure Ulcers
Which Alternative Is Preferred
It is important to recognize that none of these alternatives makes a patient with ulcerative colitis normal. Each alternative has perceivable advantages and disadvantages, which must be carefully understood by the patient prior to selecting the alternative which will allow the patient to pursue the highest quality of life.
Ready for an appointment?
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
You May Like: Is Colitis Different From Ulcerative Colitis
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Also Check: What Causes Acute Ulcerative Colitis
When Is Ulcerative Colitis Surgery Needed
Your doctor may suggest surgery if you can’t control inflammation and ulcers with medication or other treatments. You may also need an operation if you get emergency complications of ulcerative colitis such as severe bleeding or tears in the colon. Some people choose to have surgery if their symptoms affect their ability to work and stay active.
Ulcerative Colitis Treatment Options
The primary goal in treating ulcerative colitis is to help patients regulate their immune system better. While there is no known cure for ulcerative colitis and flare ups may recur, a combination of treatment options can help you stay in control of your disease and lead a full and rewarding life.
Treatment for ulcerative colitis is multifaceted and includes the use of medication, alterations in diet and nutrition, and sometimes surgical procedures to repair or remove affected portions of your GI tract.
Recommended Reading: Ozanimod Ulcerative Colitis Phase 3
Ulcerative Colitis Surgery Cost
As surgery for ulcerative colitis requires at least one and possibly three hospital stays, it comes at a higher cost than procedures that can be done as outpatient surgery. Ileostomy surgery may cost approximately $39,000, while j-pouch surgery may cost $50,000.
Check with your insurance provider to find out how much will be covered and what co-pays may be required. Using a hospital and surgical team in your plan’s network is key to preventing any unexpected charges.
Proctocolectomy With Brooke Ileostomy
Description of procedure
Indications
Most patients are suitable candidates for this operation irrespective of age. The choice of this operation is often appropriate for patients who wish to avoid the problems associated with ileoanal pouch procedure or those who are not suitable candidates for a resortative procedure, especially in elderly patients and those with poor sphincter function.
Contraindications
IPAA is now the surgical procedure of choice in most patients with UC .
Contraindications
Operative factors
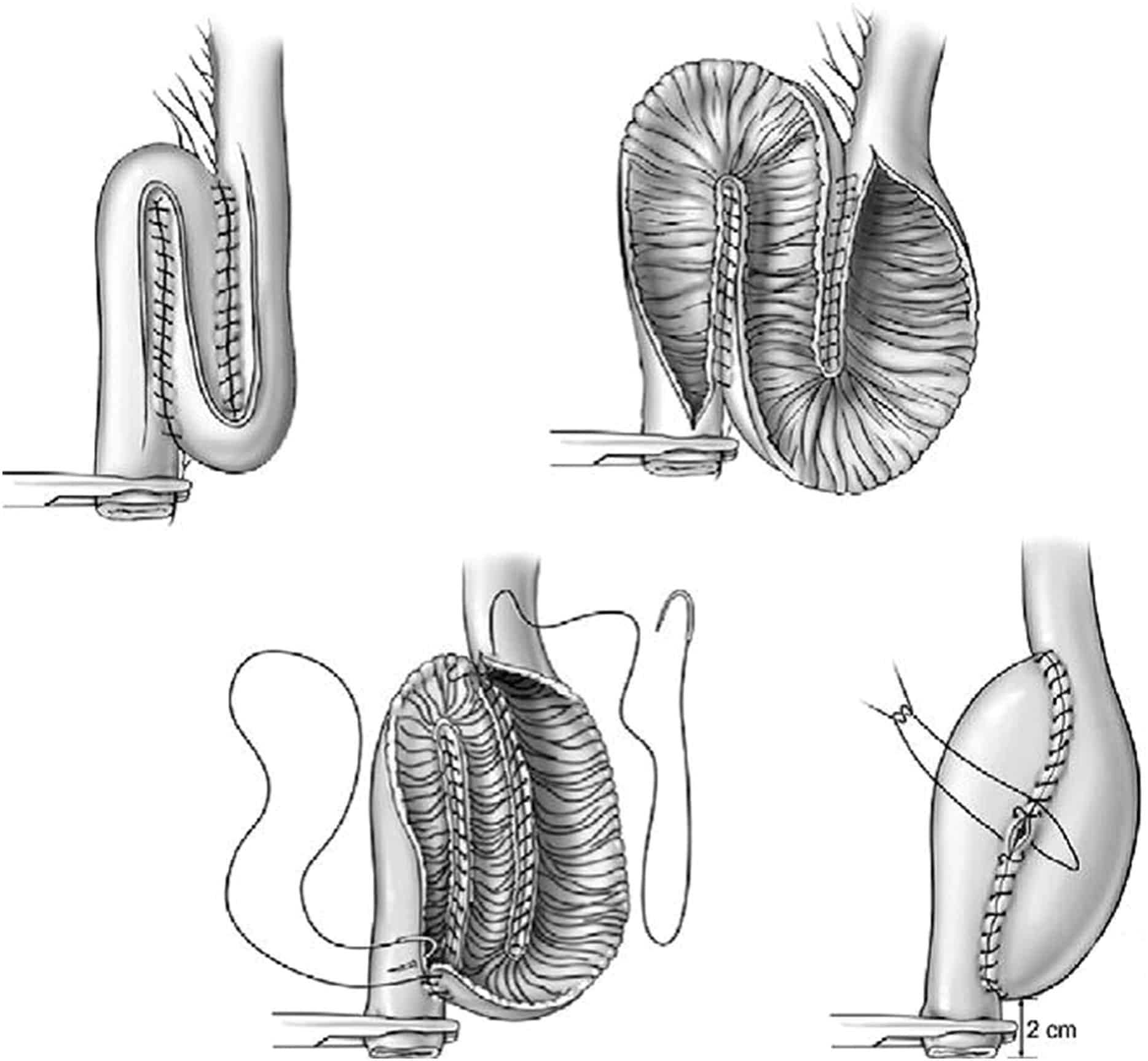
The ileal pouch is constructed using one of the several pouch designs, which include the J-pouch, S-pouch and W-pouch. The ultimate choice of pouch design is largely the surgeon’s preference, studies to date suggesting that J and W produce similar results. The S pouch is considered an inferior design, especially when there is a long exit spout, as this can cause obstructive defecation problems which at times require intubation of the pouch to empty it . The J-pouch design is the most commonly used in part due to the ease of construction.
Complications
Bowel obstruction is common following all types of surgery for UC. The annual risk for patients following IAPP is 1 in 25, 1 in 49 for a Kock pouch, 1 in 66 for a proctocolectomy and Brooke ileostomy, and 1 in 71 for colectomy and ileorectal .
Outcome
You May Like: How Long Do Stomach Ulcers Last
What Are The Benefits Of Ulcerative Colitis Surgeries
If the entire colon and rectum are removed, ulcerative colitis is cured. This should put an end to the diarrhea, abdominal pain, anemia, and other symptoms.
In addition, this surgery prevents colon cancer. Overall, an estimated 5% of ulcerative colitis patients will get cancer. Removing the colon cancer threat is especially significant for people who have ulcerative colitis that affects the entire colon. In these cases, as opposed to cases of ulcerative colitis that affect only the lower colon and the rectum, the cancer risk without surgery could be up to 32 times the normal rate.
Medical Versus Surgical Management Of Refractory Moderate
Reconstructive surgery may be offered to refractory and corticosteroid-dependent patients and improves quality of life despite the risk of early and late complications . Proctocolectomy with end-ileostomy is an alternative for some patients and has lower morbidity and comparable quality of life
Five systematic reviews were performed to define the risk of early and late complications after restorative proctocolectomy with IPAA. Early complications occurred in 965% of patients, and late complications occurred in 355% of patients., Systematic reviews indicate that the most frequent complications were pouchitis ,, wound infection ,,, bowel obstruction ,, ileus , sepsis ,, anastomotic leak ,, and fistula . The most common late complications were ileus , faecal incontinence , pouch loss ,, chronic pouchitis ,, Crohns-like disease of the pouch , and fistula . The overall mortality rate after surgery was 0.1%.
The studies that compared ileostomy with IPAA were all retrospective and revealed similar results, using a different QoL score. Occasionally the scores obtained in specific domains of health-related QoL differed significantly between the surgical techniques . Removing the diseased colon offers a good QoL when compared with medical treatment in UC patients, with a morbidity ranging between 20% and 25%.
Recommended Reading: Venous Stasis Ulcer Wound Care
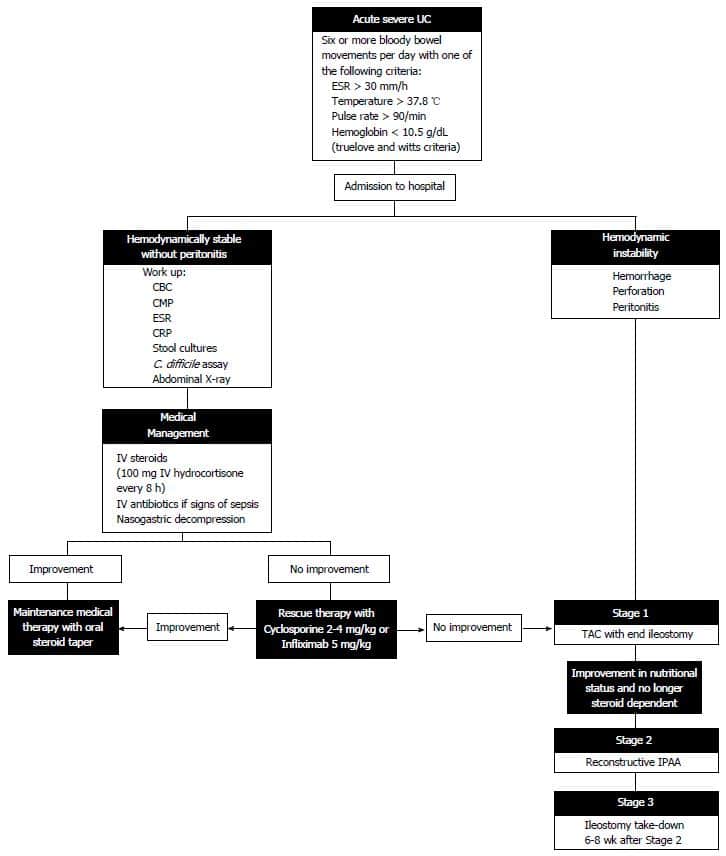
Timing Of Surgical Intervention
Timing of the surgical intervention is the major preoperative concern in UC. Emergency surgery should be avoided if possible, but if it is indicated, most advocate use of a staged procedure. Initially, emergency total colectomy with end ileostomy is performed to alleviate the major symptoms of the disease, including bleeding and pain, and allows the patient to be weaned from steroids.
Later, an IPAA is created, if the patient desires it, with removal of the remaining rectum. Most advocate leaving the rectum in place during the initial emergency operation to prevent disruption of the pelvic tissue planes, with the aim of making the subsequent pelvic dissection safer. If the patient has mild disease or disease in remission, total proctocolectomy with the creation of an IPAA may be performed as the initial definitive procedure.
Ulcerative Colitis Treatment: Surgery
If you did not respond to a medication regimen or you developed complications of colitis, you may be a candidate for surgery to treat ulcerative colitis.
Colectomy may be used in children with ulcerative colitis who experienced growth retardation. In all patients, elective colectomy can be a cure for ulcerative colitis. Almost always, the procedure is a total colectomy, meaning the entire colon is removed.
Surgical procedures include:
-
Total proctocolectomy with Brooke ileostomy. Removal of your entire colon and rectum. Your doctor will perform an ileostomy, which brings out your small intestine through the abdominal wall. Waste collects in an ileostomy bag. An ileostomy can be temporary or permanent.
Read Also: Most Common Extraintestinal Manifestation Of Ulcerative Colitis
Living With An Ileostomy
You can live a long, active, and productive life with an ileostomy. In many cases, ileostomy patients can participate in the same activities they did before the surgery, including sports, outdoor activities, swimming and other watersports, travel, and work.
Whether your ileostomy is permanent or temporary, it is common for patients to initially feel self-conscious about their ostomy and you may notice a change in how you feel about your body image. Some patients prefer to limit how visible the bag is to others. The ostomy bag typically lays fairly flat under your clothing.
Remember, it is just as important to take care of your mental and emotional health as it is your physical health. Speak with your doctor or a mental health professional if you feel you are experiencing symptoms of depression or anxiety.
-
There are several pouching systems for you to choose from. You will learn how to use your system as well as how to care for the skin surrounding the stoma.
-
Talk to your doctor about any specific dietary restrictions with an ileostomy. It is important for you to drink plenty of fluids to avoid dehydration and loss of electrolytes.
-
Eating foods high in pectin, including applesauce, bananas, and peanut butter, will help thicken your stool output and control diarrhea. Discuss this with your doctor.
The United Ostomy Associations of America has additional resources as you learn to live with your ostomy.
Medical Management Of Asuc
Intravenous corticosteroids as the initial standard treatment for adult patients with ASUC are recommended, as this treatment induces clinical remission and reduces mortality
The only randomised controlled trial including placebo in the setting of ASUC is the paramount work by Truelove and Witts, who observed that steroids induced clinical remission and decreased mortality without increasing serious adverse events., Risk of bias led to downgrading of the evidence level from 2 to 3. No conclusions could be drawn about the need for surgery, as the authors included derivative ostomies and colectomies without distinguishing the type of surgery in the report. Since the results of this pivotal study, placebo-controlled trials to clarify these and other aspects would be unethical.
Either infliximab or cyclosporine should be used in adult patients with steroid-refractory ASUC. When choosing between these strategies, centre experience and a plan for maintenance therapy after cyclosporine should be considered
There is currently insufficient evidence to determine the optimal regimen of infliximab rescue therapy in patients with ASUC refractory to corticosteroid therapy
A retrospective cohort study did not reveal differences in short-term or long-term colectomy rates between ASUC patients treated with accelerated- or standard-dose infliximab.
Don’t Miss: Infliximab Vs Adalimumab Ulcerative Colitis
Treating Uc Symptoms At The Source
To get ahead of UC symptoms, first you have to know whats behind them. UC symptoms are linked to excess inflammation that causes damage to your colon lining.
Controlling inflammation over time can help reduce UC symptoms such as frequent and urgent bowel movements, bloody stools, and abdominal pain. Controlling inflammation can also help repair the colon lining.
Controlling inflammation to help repair your colon lining and improve your symptoms is a goal of UC treatment.
UC treatments are designed to control the excess inflammation in your colon. When inflammation is suppressed, it can help relieve common UC symptoms, achieve and maintain remission, and also help heal the tissue in your colon lining.
While many UC treatments are designed to control excess inflammation, some treatments work in different ways than others. You and your doctor should discuss all treatment options and considerations to find the one that may be right for you.
What is remission?
When your UC is in remission, it means you are experiencing no symptoms. If you think about all the ways UC symptoms may be impacting your life, its easy to see why achieving and maintaining remission is so important.
Perforation Of The Colon
Chronic inflammation caused by ulcerative colitis can weaken the wall of the colon until a hole, or perforation, develops. Once the colon has been perforated, the contents of the intestine can spill into the abdomen and cause a serious infection called peritonitis.
This is a potentially life-threatening condition that needs immediate medical treatment.
Read Also: What Foods To Eat If You Have An Ulcer
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Also Check: What To Use For Stomach Ulcer