Ulcerative Colitis: Achieving And Maintaining Remission
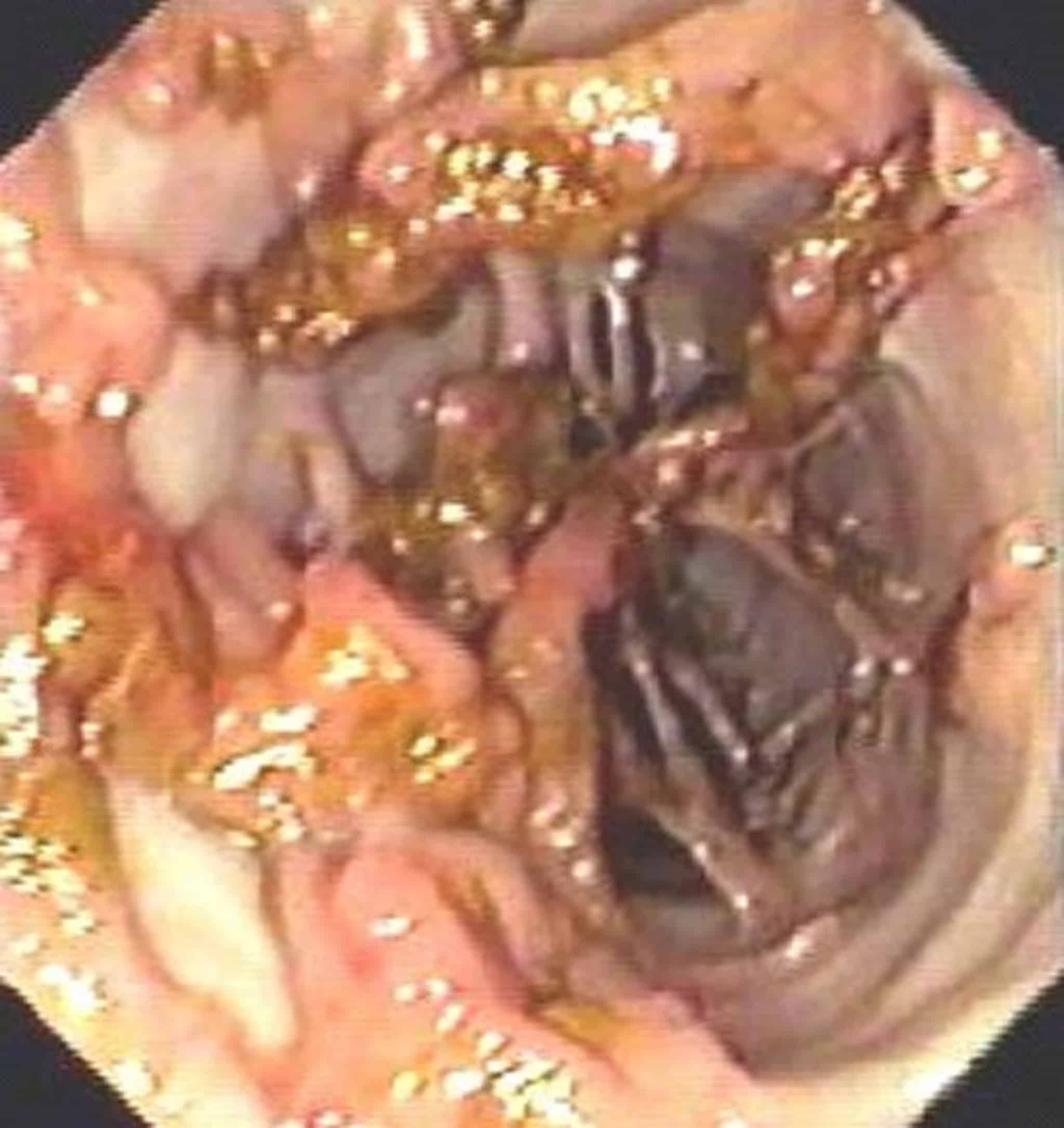
US Pharm. 2008 33:30-37. Ulcerative colitis is a chronic inflammatory bowel disorder characterized by diffuse mucosal inflammation of the colon. It affects between 250,000 and 500,000 Americans.1 Unlike Crohn’s disease, which may affect the entire gastrointestinal tract, UC is limited to the colon. UC almost always involves the rectum, but may extend proximally in a contiguous fashion to involve portions of, or the entire, colon . In the majority of new cases diagnosed, disease is limited to the distal or left side of the colon, and there is some evidence that aggressive pharmacotherapy early in the disease may prevent progression and extension of inflammation.2 This article will review the initial treatment options for UC and their place in therapy for both acute attacks and maintenance of remission.
Patients And Control Subjects
Between May 2007 to February 2013 all patients with UC who underwent a surveillance colonoscopy at the endoscopy unit at Umeå University hospital were invited to participate in the study . At our clinic all patients with an extensive UC are invited to enter a surveillance colonoscopy program for ten years after diagnosis with the aim to detect dysplasia and early cancer. Control subjects were recruited from patients who underwent a surveillance colonoscopy due to hereditary familiar colon cancer.
Both patients and controls were sent an informed consent, questionnaires and a faecal calprotectin test 46 weeks before the planned colonoscopy.
Exercising During A Flare
The first thing to know is that your exercise routine mid-flare is going to look different from your exercise routine during a remission.
During an IBD flare, your body works overtime to fight building inflammation. You may experience diarrhea, urgency, abdominal pain, rectal bleeding, and fatigue. With these symptoms, itâs understandable if you donât exactly feel like rushing off to the gym.
Even so, itâs not a good idea to avoid exercise altogether. After all, it still has the same benefits â increasing quality of life, reducing stress, and keeping your muscles and joints active â that it has at other times.
I know from personal experience how hard it can be to work out during a flare when I only feel like laying on the couch. I switched my language from âworking outâ to âmoving my body,â which has helped me shift the way I view exercise when Iâm sick.
Now, when Iâm in a flare, I challenge myself to move my body for 10 minutes every day. If you can only do 5 minutes on a given day, thatâs great too! I usually commit to stretching and walking every day, but other low impact exercises, such as yoga, biking, and swimming, are also good options during a flare.
For motivation, I talk with friends on the phone or listen to a favorite podcast while going for a slow walk around the neighborhood. On a day when Iâm experiencing less pain or fatigue, I challenge myself to walk a bit further.
Also Check: How To Self Treat An Ulcer
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
How I Exercise With Ulcerative Colitis In And Out Of Remission
Content created for the Bezzy community and sponsored by our partners. Learn More
Ella Uzan/Getty Images
â¢â¢â¢â¢â¢
Danielle Hildreth, RN, CPT
â¢â¢â¢â¢â¢
â¢â¢â¢â¢â¢
â¢â¢â¢â¢â¢
Danielle Hildreth, RN, CPT
â¢â¢â¢â¢â¢
â¢â¢â¢â¢â¢
IBD symptoms can make you want to retreat to the couch. Hereâs how â and why â to keep moving.
I grew up being active and participating in sports: track, softball, soccer, swimming, rock climbing. You name it, I played it.
Then, I was diagnosed with ulcerative colitis at the age of 19, and I had no idea if I would be able to be active again. I thought my life as I knew it was over. Little did I know, I would go on to run a marathon , get back to swimming, learn to enjoy yoga, and become an avid CrossFitter.
Over time, I discovered that movement is actually important in managing inflammatory bowel disease , so Iâve found ways to exercise that work well for me and my body â both during remissions and flares.
You May Like: Heel Protectors For Pressure Ulcers
Cut Out Triggers And Follow A Gluten
Cut out foods that can trigger your symptoms. In many cases, this could be gluten or dairy. GFCF refers to a strict elimination diet of foods containing gluten and casein . Know more here.
You may be prescribed an allergy test to identify foods you need to avoid. It may surprise you because sometimes, foods you have grown up eating may suddenly become allergens. Why? You have a weak gut. Eliminate these until you have rebuilt your gut health. Then under the supervision of your doctor and your integrative nutritionist, reintroduce them slowly.
That being said, remember you are unique. Different foods trigger inflammation in different people.
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Also Check: What Causes Ulcers In Your Colon
Clinical Remission At Week 14
The proportion of patients in clinical remission at week 14 was significantly greater in the combined VDZ group than in the PLA group: 32.7% vs 20.1% based on pMS , and 47.3% vs 28.9% based on RBS . The proportion of patients in clinical remission at week 14 in the VDZ/PLA and PLA treatment groups, respectively, was 61.1% vs 20.1% based on pMS and 69.8% vs 28.9% based on RBS .
Week 14 clinical remission rates in the week 6 responders within the VDZ group were similar to those in the overall VDZ/PLA group, whereas week 14 rates in the week 6 nonresponders within the VDZ group resembled those in the PLA group. Based on pMS, the week 14 clinical remission rates were 63.4% in week 6 responders in the VDZ group and 61.1% in the overall VDZ/PLA group, who were all week 6 responders. In contrast, week 14 clinical remission rates in week 6 nonresponders within the VDZ group were comparable to those in the PLA group . Results based on RBS paralleled those based on pMS, with week 14 clinical remission rates in week 6 responders within the VDZ group close to those in the VDZ/PLA group , and with the week 14 rates in week 6 nonresponders in the VDZ group also comparable to those in the PLA group .
The Right Way To Add Protein
Protein is crucial for building muscles and overall recovery, but it can cause heaviness if you overdo it. Be watchful. You can include these proteins in your routine: overnight soaked pulses, lean organic chicken , whole free-range eggs, and a few carefully chosen nuts or seeds. The more thoroughly and mindfully you chew it, the less likely it will worsen your symptoms because it will reduce the burden on your digestive system.
Recommended Reading: Can You Get An Ulcer In Your Colon
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Why Patients Stop Uc Treatment
People stop taking their ulcerative colitis medications for a number of reasons, says Phanijphand.
One of the leading reasons is the steep cost of the drugs. The out-of-pocket cost for prescription medicines can run over $2,000 per year, while the cost of UC care in general can run from roughly $15,000 to $25,000 per year, according to a study published in Inflammatory Bowel Diseases in January 2020.
The study also found that patients using biologics had the highest costs. Treating UC with corticosteroids had higher costs than with nonsteroidal anti-inflammatory drugs, but the latter groups costs rose more over time.
Also, when a person feels better, they may decide they no longer need UC medicine.
âSome patients think that once their symptoms are gone, they can stop taking their meds,â Phanijphand says. âThey believe theyâre cured or that they may have been misdiagnosed.â
Recommended Reading: Lunch Ideas For Ulcerative Colitis
Can I Stop Taking My Meds In Deep Remission
In a word: no. The key to remaining in remission is sticking to your recommended treatment plan. A study published in PLoS One found that people in remission who stopped taking their meds were five times more likely to relapse. Treatments that may help achieve or maintain UC remission include aminosalicylates, drugs that reduce inflammation in the lining of the colon, and immunomodulators, meds that modify the immune system in order to decrease the bodys inflammatory response. All treatments come with potential side effects, and it can take time to find the one that works best for you.
Small Intestinal Bacterial Overgrowth
Our guts are made up of trillions of bacteria. The majority of these bacteria live in our colon but sometimes some of the bacteria which should be living in your colon ends up in your small intestine1. This is known as small intestinal bacterial overgrowth – or SIBO. In a small number of cases SIBO occurs as a result of an overgrowth of the bacteria which are meant to be in your small intestine. This overgrowth can interfere with digestion of food and absorption of nutrients. This tends to happen by the bacteria damaging the cells lining the small bowel . Some people believe this damage can lead to leaky gut although not all medical professionals recognise this as a condition.
Symptoms of SIBO include bloating, abdominal distension, abdominal pain or discomfort, diarrhoea, fatty stools, fatigue, gas, belching, and weakness. In some severe cases weight loss and nutritional deficiencies may be present, particularly iron and vitamins A, B12, D, E and K. It can cause serious health issues if left untreated.
The believed cause of SIBO is complicated and may be as a result of a number of factors . These can include:
- Low stomach acid
- Diabetes mellitus
- Multiple courses of antibiotics
- Organ system dysfunction, such as liver cirrhosis, chronic pancreatitis, or renal failure
- Moderate to high alcohol consumption
- Oral contraceptive pills
- Immunosuppressant medications and proton pump inhibitors
Also Check: Do Bleeding Ulcers Cause Blood In Stool
Control And Manage Stress
If youre under any stress, you need to control, manage or avoid it. When youre stressed, your body triggers the release of chemicals such as cytokines which can attack your immune system and lead to inflammation.
If you need help managing things around you, make sure you ask for help from relatives or friends. While we cant eliminate stress altogether, we can change our relationship to it by bringing in stress resilience tools to help ourselves cope like meditation, yoga, walking, or calling a friend.
Clinical Remission Generally Means No Symptoms
When the symptoms of UC are gone , thats considered clinical remission, explains Steve Serrao, Ph.D., the division chief in gastroenterology at Riverside University Health System in Moreno Valley, CA. Gastroenterology societies use guides such as the Simple Clinical Colitis Activity Index to gauge UC activity, and doctors also recommend using a stool/food diary to log symptoms. Check out apps like mySymptoms Food Diary to help you collect this information.
Also Check: Stage 4 Pressure Ulcer Mortality
Can Your Ulcerative Colitis Go Into Remission
If you or a loved one has ulcerative colitis , you probably know there isn’t a cure for the disease. But thankfully, it’s possible to break free of symptoms by achieving remission.
Doctors define remission of ulcerative colitis as having three or fewer stools per day without blood or an increased urgency to go. Many people with UC can achieve remission with medications. This symptom-free time can last a few months or even yearsa welcome relief from the condition.
Fiber To Eat Or Not To Eat Is The Question
If you are an ulcerative colitis patient with a lot of pain during flare-ups, fiber could be your biggest enemy. Common triggers include highly fibrous foods like nuts, seeds, leafy green vegetables, and popcorn. Eating these difficult-to-digest foods with an already-inflamed colon will only aggravate symptoms.
Be careful. Dont just pump yourself with insoluble and soluble fiber. Use fiber in small amounts from fruits or certain vegetables. Cook or soak lentils or legumes. Use asafoetida to make these easy for your gut to break down. Try steaming, baking, or stewing certain fibrous foods like cruciferous vegetables.
Once you are in remission, fiber will become your best friend again.
Read Also: What Foods To Eat With Ulcerative Colitis
Active Uc Of Any Extent Not Responding To Aminosalicylates
In mild-to-moderate UC of any extent, aminosalicylates such as mesalamine are the preferred initial treatment . In patients with disease activity limited to the rectum, topical therapy alone might suffice, but combination therapy is more effective and is also recommended for left-sided and extensive UC . Table 2 gives an overview on current treatment options.
Table 2.
Medical therapy for UC
Fig. 1.
Active ulcerative colitis of any extent not responding to 5-aminosalicylates . MMX, multimatrix AZA, azathioprine 6-MP, 6-mercaptopurine.
Except in case of isolated proctitis, where topical corticosteroids alone may be considered, treatment with oral corticosteroids should be initiated in patients who do not respond adequately to 5-ASA . In case of isolated proctitis, topical corticosteroids alone might be considered. The introduction of corticosteroids should be a shared decision-making process that includes patients preference of therapy and tolerance to 5-ASA. It is, however, recommended to start corticosteroids in patients with sustained rectal bleeding for 2 weeks, persistent abdominal symptoms after 6 weeks of adequate therapy with 5-ASA or if symptoms deteriorate . In selected cases, a prolonged therapy with up to 16 weeks might still be able to achieve remission.
You May Like: Stage 2 Pressure Ulcer Treatment Dressing
Ulcerative Colitis Remission Better Maintained After Infliximab Treatment
New data has investigators caution against the discontinuation of ulcerative colitis treatment, due to threat of relapse.
Taku Kobayashi, MD
A recent study found that maintaining ulcerative colitis remission was significantly more common in patients who continued treatment with infliximab, compared to those who discontinued treatment.
The use of anti-tumor necrosis factor agents is common in the treatment of refractory UC, but the long-term use of anti-TNF therapy can increase the risk of malignancy or infection.
No previous study trial has evaluated the safety of anti-TNF agent discontinuation in patients with UC in remission.
The team, led by Taku Kobayashi, MD of the Center for Advanced IBD Research and Treatment, Kitasato University Kitasato Institute Hospital in Tokyo, looked to compare outcomes in patients who continued and discontinued infliximab treatment.
Thus, investigators conducted an open-label, randomized controlled trial at 24 specialist centers in Japan.
The study enrolled patients with UC in remission who had been treated with intravenous infliximab every 8 weeks. Patients were required to have started treatment 14 weeks prior to enrollment in the study.
Patients were also required to be in remission for more than 6 months, to be corticosteroid-free and have a Mayo Endoscopic Subscore of 0 or 1. The group was then randomized and put into either the infliximab-continued group or the infliximab-discontinued group.
Read Also: What Foods Can You Eat With A Peptic Ulcer
Will My Uc Symptoms Come Back
Because UC is a chronic disease, its possible that you could have a flare-up in the future, even after a long period in remission. And even if you stay in remission, you might still have symptoms like diarrhea, abdominal pain, or fatigue from time to time. It can be difficult to tell whether these symptoms are caused by UC, or whether theyre caused by something else, like irritable bowel syndrome , an infection, small intestinal bacterial overgrowth, or even dietary changes, Dr. Chang says. If you do experience any symptoms, you should discuss them with your doctor.