Pain As A Tool For Diagnosis
Because pain can come from different sources, and pain in the abdomen is particularly difficult to pinpoint, it is not a symptom that is normally used to diagnose IBD or a particular form of IBD.
Rather, the type and location of pain is more often used together with other signs and symptoms when diagnosing IBD or other conditions. In other words, it might be a starting point to help a healthcare provider know where to start looking for inflammation, but its only one part of the picture.
What Are The Causes And Risk Factors Of Ulcerative Colitis
Ulcerative colitis is believed to be caused by an abnormal response by your bodys immune system.
Your immune system is supposed to defend you against harmful invasive bacteria and viruses. But in some people, the immune system mistakenly attacks the bodys own tissue.
While we dont know exactly what causes ulcerative colitis, there are two leading theories:
Experts believe that ulcerative colitis develops because of a combination of environmental factors and genetic predisposition.
Fatty cold-water fish such as mackerel, tuna, salmon, sardines, and herring are rich sources of omega-3 fatty acids.
Editorâs Picks
Treating Back Pain In Ulcerative Colitis
Treating back pain in ulcerative colitis can be complicated. Research shows that treating the underlying UC can help lessen the severity of spondyloarthritis, but it will not resolve spondyloarthritis and back pain. Back pain must be addressed separately and in a way that does not make a persons UC symptoms worse.
People with ulcerative colitis may need to work with both a rheumatologist and a gastroenterologist to manage their gastrointestinal and spinal health properly. These doctors may prescribe or recommend the following treatments and therapies.
You May Like: Doctors Specializing In Ulcerative Colitis
The Role Of Other Proteins
Macrophages expressing the transmembrane protein CD163, which is a member of the scavenger receptor cysteine-rich superfamily that functions in the development and regulation of the immune system, are increased in noninflamed SpA colonic mucosa and in SpA synovium. Demetter et al. found that CD163+ macrophages are increased both in CD and SpA gut mucosa. These observations illustrate that not only T cells but also antigen presenting cells accounts for the relationship between joint and gut inflammation.
Demetter et al. observed an upregulation of E-cadherin, a transmembrane glycoprotein which mediates intercellular adhesion of epithelial cells, and an upregulation of its associated catenins in gut mucosa in IBD. This upregulation was detectable in acute as well as in chronic subclinical gut inflammation in SpA., E-cadherin is also a ligand for the E7 integrin, which is upregulated in colonic mucosa in CD and AS patients and in inflamed synovial tissue in SpA patients., These findings may suggest that these upregulations may play a role in the pathogenesis of IBD or SpA, or both.
-
Activated intestinal lymphocytes in IBD patients adhere to inflamed synovial vessels were VAP-1 supports the binding of all leukocytes.
-
NOD2 does not have a clear association with arthropathy in IBD patients.
-
HLA-B27 carriers and AS in IBD patients are associated.
Back Pain Often Comes Directly From Back Or Spinal Structures But Sometimes Its A Sign Of A Medical Condition Elsewhere In Your Body Heres What Else Could Be Causing Your Back Pain
Heres a scene that plays out every day, all over the world: Someone thinks they have a little back strain. Perhaps they lifted something wrong or moved the wrong way. It was just a twinge, so they waited it out a few days for the pain to go away. It doesnt, so they head to their doctor. Turns out, they hadnt lifted anything wrong at all. It was the start of a kidney infection, or a UTI, or pancreatitis.
Heres how to tell the difference between a back strain and something more serious going on.
How do you know when the root cause of back pain is elsewhere in your body? There are two types of pain we look at, explains Matthew Crooks, MD, a pain specialist at Pinnacle Pain and Spine in Scottsdale, Arizona: visceral pain and somatic pain. Visceral pain is pain from an organ or internal pain that can radiate to the spine with conditions like pancreatitis, ulcerative colitis or Crohns disease, gall stones, cancers, kidney pain, and urinary tract infection, says Dr. Crooks.
Whats more, thanks to aging, injury, or a sedentary lifestyle, almost everyone has some wear and tear in the spine and pain in the musculoskeletal system . When you do develop visceral pain, it can flare up your somatic pain. And thats separate from the pain thats radiating from an organ, says Dr. Crooks. It can be activated from overall inflammation and the stress of the body dealing with the medical issue. Its the BOGO special that you never want.
Don’t Miss: Best Treatment For Stage 3 Pressure Ulcer
Mri Scans And Mr Enterography
An MRI scan uses a magnetic field and radio waves to create two- and three-dimensional images of the body. MRI scans are especially helpful when doctors need to visualize soft tissues, such as the lining of the intestines. They may reveal small tears or ulcers, as well as irritation or bleeding.
To get a better look at the gastrointestinal tract, the doctor may ask you to drink a contrast agent just before the MRI. This is called MR enterography.
Skin Joint Or Eye Problems
When you have UC, the lining of your large intestine gets inflamed and sets off your symptoms. For some people, this inflammation also shows up in other body parts during a flare. Experts arent sure why.
You could have symptoms like:
Let your doctor know whenever you get new UC symptoms. That way, they can change your treatment plan if needed.
Recommended Reading: Over The Counter Remedies For Ulcers
Read Also: Turning Patients Every 2 Hours To Preventing Pressure Ulcers
When Does Cramping Usually Happen
UC cramps can be exacerbated by food, so many people notice cramping after eating or before a bowel movement, says Ha. Cramping can also be tied to eating trigger foods, which often include high-fiber fruits and veggies, lactose, nonabsorbable sugars, high-fat or sugary foods, alcohol, and caffeine.
The hormone fluctuations that occur during a womans menstrual cycle may also trigger UC cramping, according to a study published in January 2018 in Inflammatory Bowel Diseases.
Cramping can occur at all times and throughout the night. Medication and other treatments can help reduce symptoms.
Heres What You May Not Know About Ibd And Arthritis
Inflammatory bowel disease is associated with arthritis. Research suggests there could be a genetic component or the connection could be associated with an inflamed gut. Learn more here.
Inflammatory bowel disease has long been associated with the development of arthritis. Research suggests there could be a genetic component or the connection could be associated with an inflamed gut.
While rheumatoid arthritis patients can develop IBD, the type of arthritis typically associated with IBD is entirely different and is one that primarily affects the large joints but without long-term damage as seen in RA.
In this article, we feature a Q& A by Timothy R. Orchard, M.D., a gastroenterologist with St. Mary’s Hospital of Imperial College in London, that was published in 2012 in Gastroenterology and Hepatology. Dr. Orchard shares his expertise and insights on arthritis after an IBD diagnosis.
Types of arthritis in IBD
There are some joint problems that are unique to patients who suffer from inflammatory bowel disease : inflammatory arthritis and arthralgia with the latter occurring in 40-50 percent of IBD patients. Of these, 15-20 percent have Crohn’s disease and 10 percent have ulcerative colitis.
A smaller number of IBD patients have symmetrical polyarthritis which is typically seen in rheumatoid arthritis patients who develop inflammation in any joint, but most often smaller joints in the hands.
Misdiagnosis
Arthritis in Crohns disease and ulcerative colitis:
Treatment
Don’t Miss: Ulcerative Colitis Diet During Flare
Our Approach To Arthritis Of Inflammatory Bowel Disease
Treatment for arthritis linked to inflammatory bowel disease aims to address the underlying condition, the IBD itself. Most patients’ arthritis symptoms improve dramatically once their IBD is controlled.
UCSF provides comprehensive evaluations and advanced care for all types of inflammatory bowel disease. Our team includes many kinds of specialists, such as gastroenterologists, surgeons, radiologists, pathologists, immunologists, nutritionists and psychologists. Treatment options include modified diets, medications and surgery. Our goal is to improve patients’ quality of life, and we encourage their input when making treatment decisions.
In addition to caring for patients, our providers are exploring potential new therapies for IBD. Interested patients may have the option to receive investigational treatments by participating in clinical trials.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Read Also: Whats A Stomach Ulcer Feel Like
Articles On Ulcerative Colitis Overview
Ulcerative colitis affects your colon, which is part of your digestive system. A lot of things can cause trouble in that general area, so how do you know what it feels like to have ulcerative colitis?
It depends on how severe it is, and on what part of your colon is affected.
Also, symptoms can come and go. You might not have any for weeks, months, or even years, and then they come back. Chances are about 50-50 that the effects will be mild.
Still, most people with the disease have a few common issues:
Diagnostic Tests/lab Tests/lab Values
The diagnosis of Crohns disease is made by ruling out other potential causes to explain the patients signs and symptoms. Some of the tests include blood tests, fecal occult blood test , colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.
The blood tests are used to check for anemia which would indicate inflammation within the body, infection, and antibodies that might be present with individuals with inflammatory bowel disease.
The FOBT assesses an individuals stool sample for the presence of blood.
A colonoscopy allows the doctor to take a biopsy or tissue sample to determine if there is a presence of any granulomas which are common with Crohns disease and not ulcerative colitis.
The flexible sigmoidoscopy allows the doctor to assess the last portion of the colon for any biopsy samples. This allows the doctor to determine if there is any inflammation or bleeding amongst the intestines.
Barium enemas allow the doctors to assess the intestines via x-ray. The barium coats the inner lining of the GI tract to allow the lining to be visible on the x-ray.
A CT of the GI tract allows a quick look at the entire bowel in a way that cannot be seen in other diagnostic tests. This helps to assess for blockages, abscesses or fistulas.
Also Check: Dressing For A Stage 2 Pressure Ulcer
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I can’t bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I can’t fully stand upright sometimes for a minute or so. It’s frustrating.
What Kind Of Diet Is Helpful For Living With Colitis
Your healthcare provider may suggest one or several of these diets, depending on the type of colitis you have and the condition youre in:
- Low-residue diet. A low-residue diet is easy to digest when your symptoms are acute or severe. It limits fiber and fat and emphasizes soft, well-cooked foods. If you have a temporary infection or radiation colitis, your healthcare provider may recommend a low-residue diet.
- Anti-inflammatory diet. To keep chronic inflammation low, your healthcare provider might recommend you avoid highly inflammatory foods, especially fast and processed foods high in sugar and fat. They might suggest more healthy, unsaturated fats to calm inflammation like olive oil, avocados, nuts and oily fish.
- Elimination diet. If you have an inflammatory bowel disease, your healthcare provider will likely recommend an elimination diet to isolate the foods that cause your symptoms to flare up. An elimination diet eliminates certain types of foods and then adds them back in a systematic way so that you can observe how your gut responds to them. After the temporary elimination diet, you can use what you learned to design a personalized, long-term maintenance diet.
A note from Cleveland Clinic
Last reviewed by a Cleveland Clinic medical professional on 06/22/2022.
References
Recommended Reading: When Should I Go To The Hospital For Back Pain
Read Also: Can You Take Tylenol With Ulcerative Colitis
Joint Pain: The Most Common Non
About 30 percent of people with ulcerative colitis experience joint pain, according to the Crohns and Colitis Foundation, making it the most common non-GI symptom of the disease. Joint pain often occurs in the knees, ankles, elbows, and wrists. Its usually joint pain thats symmetrical, meaning both knees or both ankles, says Dr. Rubin. This type of joint pain tends to parallel bowel activityso if you fix the intestine, the joint pain goes away.
However, ulcerative colitis is also related to inflammatory joint conditions that affect your spine, like ankylosing spondylitis. This type of joint pain can be independent of your bowelso your bowel can be completely in remission, and your back or your pelvis is inflamed, and you can have joint damage, says Rubin.
The good news: Some medications used to treat ulcerative colitis are also used to treat inflammatory joint conditions like ankylosing spondylitis. Its not that fixing the bowel makes these joints betterits that the medication that works on the bowel also works on these joint conditions, says Rubin. So if youre experiencing joint pain, its important to work with your doctor to understand what type of joint pain you have and get proper treatment. In some cases it may be necessary to see a doctor who specializes in the joints, a rheumatologist, to work with your IBD doctor.
What Is The Interpretation Of The Ana Screen Result
The ANA test is a sensitive screening test used to detect autoimmune diseases. Autoimmune diseases feature a misdirected immune system, and each of them has characteristic clinical manifestations that are used to make the precise diagnosis. The interpretation or identification of a positive ANA test does not make a diagnosis. It simply suggests to the doctor to consider the possibility that an autoimmune disease is present.
Don’t Miss: Stage 2 Pressure Ulcer Treatment Cream
Believe It Or Not This Digestive Disorder Can Wreak Havoc On Your Elbowsand Knees Too We Asked The Experts For The Bottom Line
by Health Writer
Bowel inflammation may be the main characteristic of , but joint pain is far more common than many people realize. According to the Crohns and Colitis Foundation, as many as 30% of people with UC and Crohn’s disease may also experience . Most of the time, UC causes joints to feel stiff without inflammation, but other times you may also experience inflammatory arthritis that includes swelling in areas where two bones join, such as your knees, elbows, or wrists. Arthritis that is associated with UC doesnt just target your large joints in your arms and legs, thoughit can also affect your spine.
The good news? Joint pain usually disappears once the inflammation in your colon is treated. Still, it can seem a bit confusing to be experiencing joint aches when youve been diagnosed with a gastrointestinal disorder. How does it all relate? We asked the experts to break down the ways ulcerative colitis and joint pain are related.
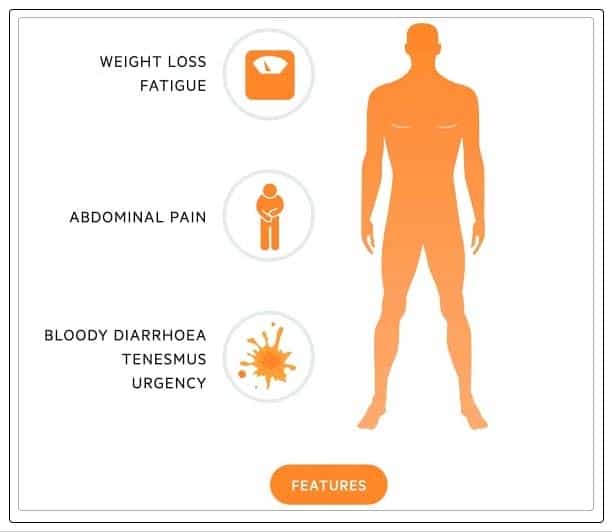
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Don’t Miss: What Foods Should You Avoid When You Have An Ulcer