About Colorectal Cancer Screening
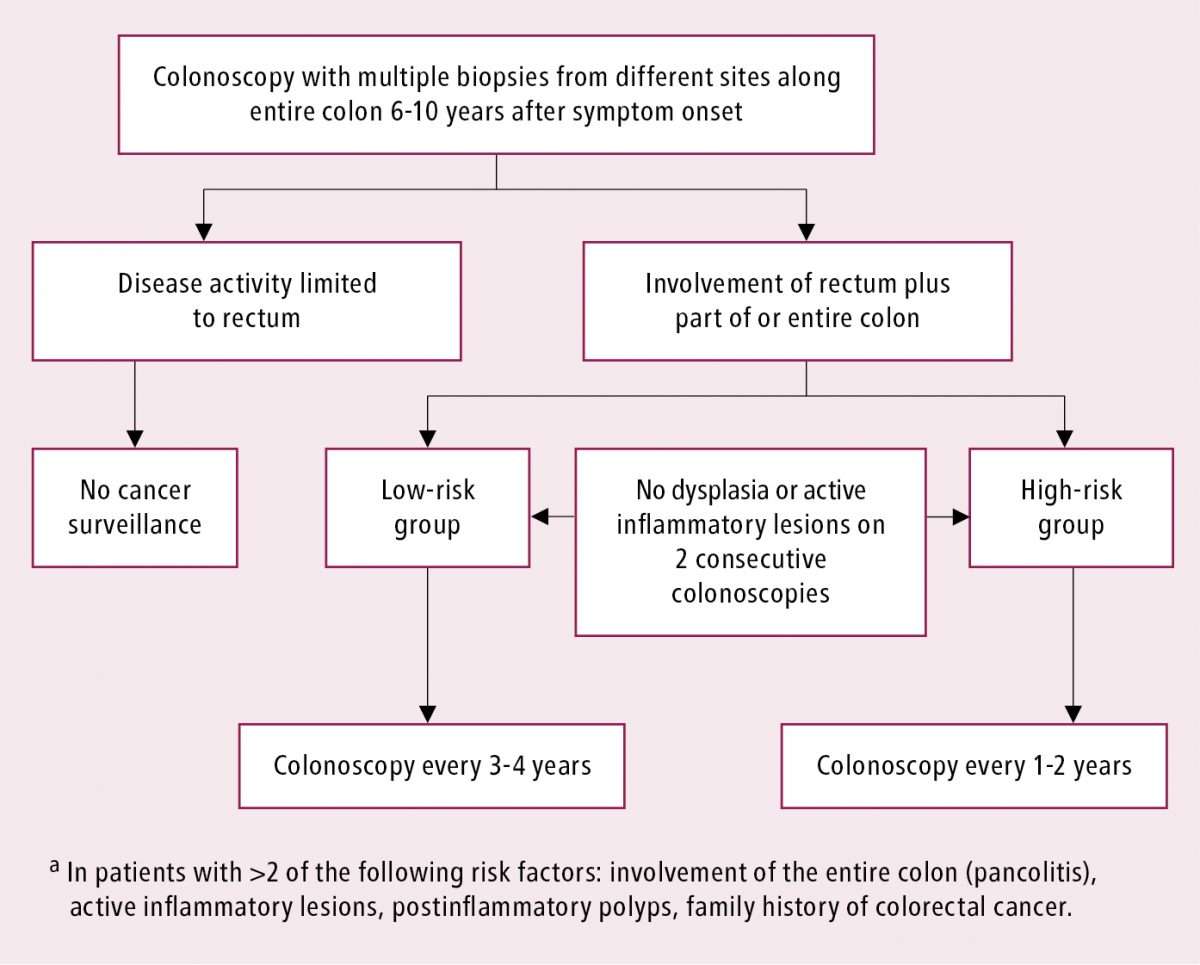
Endoscopic screening has helped increase the chances of surviving CRC in people with IBD1. ECCO recommend that all people with IBD are screened by colonoscopy to monitor for CRC. The first colonoscopy is recommended 68 years after the symptoms of IBD first occurred and either every 12 years afterwards for people at high risk of CRC or 35 years for people at lower risk of CRC.1,9
For CRC screening, a full colonoscopy is necessary, where the doctor inspects the rectum and entire colon through a flexible lighted tube, and can remove any abnormal growth. The entire colon has to be cleansed before the colonoscopy, for which the patient is usually sedated.
Colon cleansing involves taking cleansing agents, such as polyethylene glycol with or without electrolytes, or sodium picosulphate and magnesium oxide, which cause a laxative effect by drawing water into the colon and stimulating peristalsis to wash out the contents of the colon.10
References: 1: Van Assche G, Dignass A, Bokemeyer B, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: special situations. J Crohns Colitis 2013 7: 133.9: Annese V, Daperno M, Rutter MD, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis 2013 7: 9821018.10: Connor A, Tolan D, Hughes S, Carr N, Tomson C. Consensus guidelines for the safe prescription and administration of oral bowel-cleansing agents. Gut 2012 61: 152532.
Ibd Increases Colon Cancer Risk
Colon cancer is the second-leading cause of cancer death in the United States. Although anyone can develop colon cancer, certain risk factors and conditions can increase the likelihood of developing the disease. One condition that can increase the risk of colon cancer is IBD, a general term that describes chronic inflammation of the gastrointestinal tract.
There are two types of IBD:
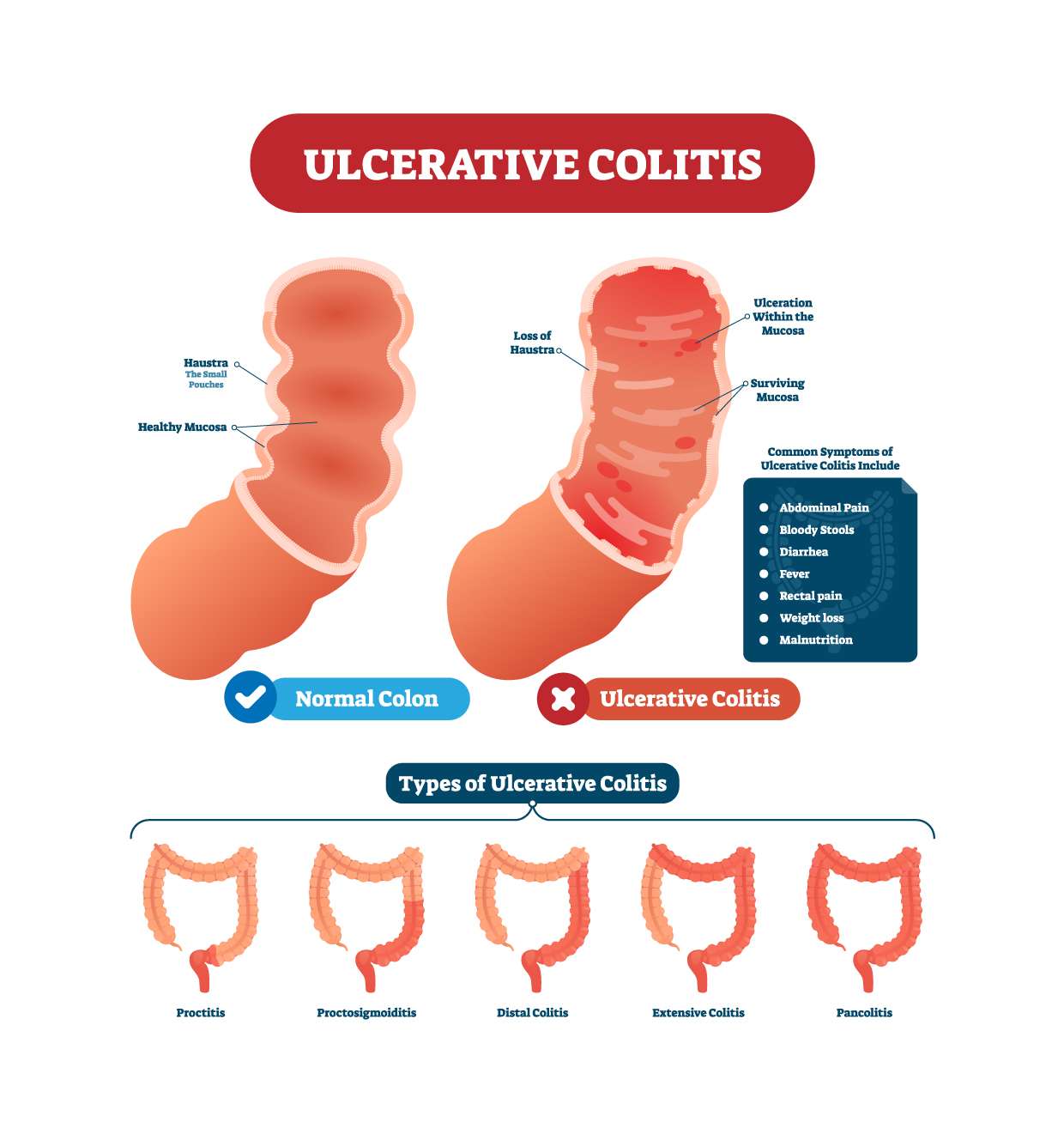
- Ulcerative colitis a chronic condition that causes inflammation of the colon
- Crohns disease a chronic condition that affects the digestive tract lining. Patients with Crohns disease may have healthy parts of the intestine as well as inflamed regions in both the small and large bowel.
Colon inflammation can cause a constant turnover of cells in the lining of the intestine, which increases the likelihood of cell irregularities that can result in cancer.
People With Iron Deficiency Anemia
- Iron deficiency anemia may be a presentation of colorectal cancer. People who present with unexplained iron deficiency anemia should be referred to have a colonoscopy on a prompt basis.
- Stool-based testing should not be used to guide the decision to refer or investigate people with symptoms or other conditions suggestive of colorectal cancer because it may lead to a delay in diagnosis.Reference 6Close referenceNarula N, Ulic D, Al-Dabbagh R, Ibrahim A, Mansour M, Balion C, et al. Fecal occult blood testing as a diagnostic test in symptomatic patients is not useful: A retrospective chart review. Can J Gastroenterol Hepatol. 2014 28: 42126.OpenCloseReference 7Close referencevan Rijn AF, Stroobants AK, Deutekom M, Lauppe C, Sturk A, Bossuyt PMM, et al. Inappropriate use of the faecal occult blood test in a university hospital in the Netherlands. Euro J of Gastroenterol and Hepatol. 2012 24:1266-69.OpenCloseReference 8Close referenceIp S, Sokoro AA, Kaita L, Ruiz C, McIntyre E, Singh H. Use of fecal occult blood testing in hospitalized patients: results of an audit. Can J Gastroenterol Hepatol. 2014 28: 489-94.OpenClose
You May Like: Ulcerative Colitis Worse At Night
Who Should Be Offered Endoscopic Surveillance
Our recommendation: After endoscopic screening, endoscopic follow-up should be performed for all patients except for those with ulcerative proctitis, CD with involvement of less than 1/3 of the colon, and those in which the risks outweigh the possible benefits.
This aspect is addressed by the majority of the guidelines, and there is a general consensus about not performing endoscopic surveillance for CRC screening in patients with proctitis or with CD of minimal extent, as their risk of developing neoplasia is very low. AGA also excludes patients with procotosigmoiditis from follow-up. Only the ECCO-Elderly, NICE and NZGG guidelines refer to the need for balancing the risks and benefits of performing endoscopic surveillance for elderly patients and those with significant comorbidities or with a short life expectancy.
Getting Screened For Cancer
Because your risk for colorectal cancer increases over time if you have UC, its important to receive regular screenings for colorectal cancer.
People with UC should talk to their doctors about getting a colonoscopy, the main test used to detect this cancer.
Getting regular colonoscopies can help lower your risk for developing colorectal cancer or dying from colorectal cancer.
For people with IBDs who underwent regular screenings, the odds of developing colorectal cancer dropped by 42 percent. The odds of dying from the cancer dropped by 64 percent.
Also Check: Foods To Avoid With An Ulcer Nhs
Ulcerative Colitis And Cancer: What Is The Connection
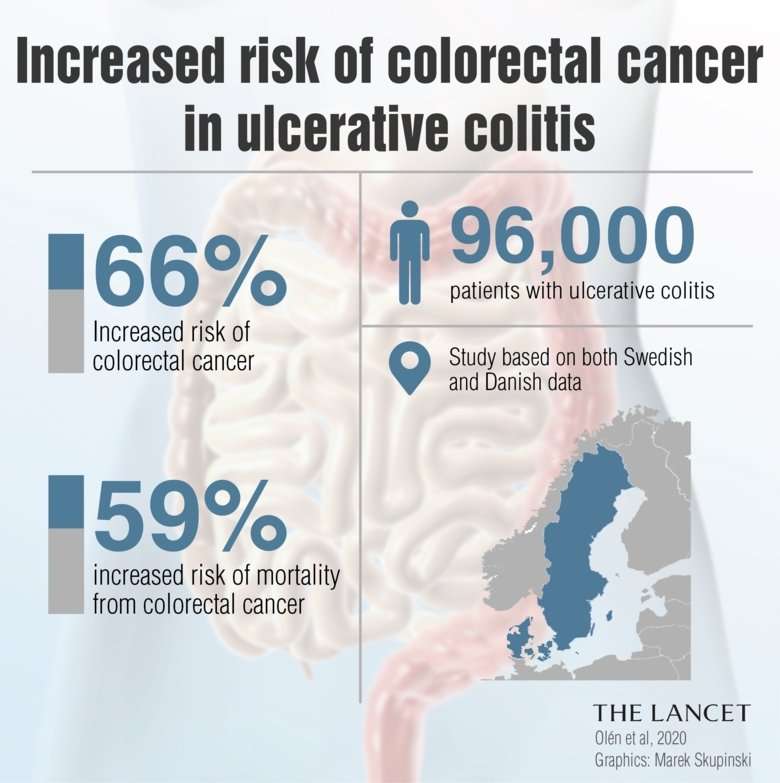
People living with ulcerative colitis are 4 to 10 times more likely to be diagnosed with colorectal cancer compared with the general population.
This is because UC patients have higher levels of inflammation in the colon and an increased risk of developing inflammatory polyps in the lining of the colon or rectum. The majority of polyps are benign , but over time, some polyps can become cancerous.
The exact risk of colorectal cancer for people with UC varies depending on these three factors:
- Duration of the disease: It is believed that the risk of developing colorectal cancer starts to increase eight to 10 years following the onset of UC symptoms. One meta-analysis of 116 studies found that 10 years after onset, the risk is 1.6% at 20 years, it increases to 8.3% and 30 years after onset, it increases to 18.4%.
- Severity of inflammation: The more inflammation that is in your colon or rectum, the more damage there is to cells in the colon lining. This causes more cell turnover, which allows more opportunity for mutations in the DNA of these cells that can lead to cancer.
- How much of the colon is affected: Those with UC of the entire colon are at the highest risk. If UC only affects the left side of the colon, the risk of developing cancer is lower. And those with UC only in the rectum don’t have a heightened risk of colorectal cancer.
How Should A Visible Lesion Be Managed
Our recommendation: Visible lesions which are well delimited, with no evidence of dysplasia in the mucosa adjacent to the lesion and without synchronous dysplasia, should be resected endoscopically regardless of the degree of dysplasia.
Lesions that are endoscopically visible and well-defined, irrespective of their location and degree of dysplasia or whether or not there is involvement by colitis, should be endoscopically resected by an expert endoscopist, and biopsies should be taken of the adjacent mucosa. The ASGE guideline also recommends preparing tattoo and photo-documentation of the resected lesions. They also suggest colectomy as a possibility to discuss with the patient, if the completely excised lesion exhibits high-grade dysplasia . If complete resection is anatomopathologically confirmed, and there is no dysplasia in the adjacent mucosa or elsewhere in the colon, the indication is close endoscopic follow-up. If the described conditions are not met, the treatment would be total colectomy.
You May Like: Besivance Dosage For Corneal Ulcer
Ibd Patients May Need A Colonoscopy Every One To Three Years
A new study published in Clinical Gastroenterology and Hepatology evaluated how varying colonoscopy intervals affected colon cancer outcomes in patients with IBD. The outcomes evaluated included the following:
- Stage of colon cancer at the time of detection
- Colon cancer treatment
- Mortality
The study showed that Colonoscopy within three years prior to CRC diagnosis compared with no colonoscopy was less likely to be diagnosed with late tumor stage, said Hyun-seok Kim, MD, MPH, of Baylor College of Medicine. Colonoscopy within one year was associated with lower all-cause mortality than no colonoscopy. Our findings support the use of surveillance colonoscopy to improve CRC outcomes in IBD patients .
What Methods Are Used To Screen People For Colorectal Cancer
Several screening tests have been developed to help doctors find colorectal cancer before symptoms begin, when it may be more treatable. Some tests also allow adenomas and polyps to be removed before they become cancer. That is, colorectal cancer screening may be a form of cancer prevention in addition to early detection.
The US Preventive Services Task Force considers the following methods to be acceptable screening tests for colorectal cancer:
Don’t Miss: Can Stomach Ulcers Cause Blood In Your Stool
Keep Up With Regular Physicals
Getting an annual physical is always smart, but it’s especially important if you have UC.
During the checkup, your healthcare provider will ask whether your treatments are going well and ensure that screening is performed at the appropriate intervals to catch any cancer in the early stages. Even if your UC symptoms are in remission , seeing a healthcare provider regularly can help ensure that you stay on the healthy track.
How Often Should I Have A Colonoscopy With Ulcerative Colitis
If you have ulcerative colitis, you may need a colonoscopy as often as every 1 to 3 years. Ulcerative colitis is an inflammatory bowel disease, and it can raise your colon cancer risk. Your colonoscopy test frequency depends on how long you have had ulcerative colitis and how much of your colon is inflamed.
Its recommended that healthy people who dont have any risk factors undergo a colonoscopy to screen for colon cancer every 10 years starting at age 45. The frequency thereafter depends on the findings.
However, ulcerative colitis is a risk factor for colon cancer, especially if your entire large intestine or bowel is involved. More frequent colonoscopies may be needed if you have ulcerative colitis, and they may need to start sooner, depending on how old you are when you are diagnosed. The peak age range for diagnosis is 15 to 30 years old.
You May Like: How To Treat Pressure Ulcers On Buttocks
Does The Occurrence Of Dysplasia Require Confirmation
Our recommendation: The occurrence of dysplasia must be confirmed by a second pathologist.
Histopathological analysis is qualitative and consequently has a high inter-observer variability, especially in low grade dysplasia and in inflamed mucosa. Therefore, there is a general consensus that the occurrence of dysplasia should be confirmed by an independent expert gastrointestinal pathologist.
For People At Increased Or High Risk
People at increased or high risk of colorectal cancer might need to start colorectal cancer screening before age 45, be screened more often, and/or get specific tests. This includes people with:
- A strong family history of colorectal cancer or certain types of polyps
- A personal history of colorectal cancer or certain types of polyps
- A personal history of inflammatory bowel disease
- A known family history of a hereditary colorectal cancer syndrome such as familial adenomatous polyposis or Lynch syndrome
- A personal history of radiation to the abdomen or pelvic area to treat a prior cancer
The American Cancer Society does not have screening guidelines specifically for people at increased or high risk of colorectal cancer. However, some other professional medical organizations, such as the US Multi-Society Task Force on Colorectal Cancer , do put out such guidelines. These guidelines are complex and are best looked at along with your health care provider. In general, these guidelines put people into several groups .
Don’t Miss: How To Treat Skin Ulcer On Leg
Primary Sclerosing Cholangitis After Orthotopic Liver Transplantation
An increased risk of colorectal cancer after orthotopic liver transplantation in patients with PSC and UC has also been reported with an incidence of approximately 1% per person per year. The risk is therefore clinically important and thus annual surveillance colonoscopy is recommended in the post-transplant period.
What Terminology Should We Use To Describe Lesions Detected With Endoscopy
Our recommendation: The terms dysplasia-associated lesion or mass and flat lesions should be discontinued. We should be using the modified Paris Classification in which lesions are divided into visible dysplasia and invisible dysplasia depending on whether the biopsy has been taken from a lesion visualised in the colonoscopy or not. Visible dysplasia is divided into polypoid and non-polypoid depending on whether or not the lesion protrudes from the lumen 2.5 mm. The descriptions of visible lesions should also include mention of whether they are ulcerated and whether the borders are easily distinguished from the surrounding mucosa.
Recommended Reading: What Does Ulcerative Colitis Mean
Availability Of Data And Materials
The data that support the findings of this study are available from the DCCSD and The Danish Health Data Authority . Restrictions apply to the availability of these data, which were used under license for this study. Data may be available upon reasonable request to the DCCSD and The Danish Health Data Authority.
How Can I Get Screened
FIT kits are currently available in every NWT community. Book an appointment with your primary care provider to get screened FIT kit. If you are aged 50-74 and of average risk, you will complete a Fecal Immunochemical Test every 1 to 2 year to be screened. This test is a simple one-and-done, at-home poop test that only requires one sample.
NEW TESTING METHOD: This test used to be a three-sample smear poop test. In June 2018 this was changed to a simple, 1-sample poke test.
In communities with hospital laboratories your primary care provider will give you a laboratory requisition to take to the lab to pick up a FIT to take home to complete. Once youve done the FIT at home you need to bring it back to the lab within 7 days.
In the communities without laboratories the FIT will be provided from the Health Centre or Health Cabin. Once youve done the FIT at home you need to bring it back to the Health Centre or Health Cabin within 7 days.
If youre considered to have an increased or special risk or developing colorectal cancer, talk to your primary care provider for them to complete a referral to the specialist.
Recommended Reading: Over The Counter Remedies For Ulcers
What Do Colorectal Cancer Screening Guidelines Say About Who Should Have Colorectal Cancer Screening
Expert medical groups, including the US Preventive Services Task Force , strongly recommend screening for colorectal cancer. Although some details of the recommendations vary, most groups now generally recommend that people at average risk of colorectal cancer get screened at regular intervals beginning at age 45 or 50 .
The expert medical groups generally recommend that screening continue to age 75 for those aged 76 to 85 years, the decision to screen is based on the individuals life expectancy, health conditions, and prior screening results.
People who are at increased risk of colorectal cancer because of a family history of colorectal cancer or documented advanced polyps or because they have inflammatory bowel disease or certain inherited conditions may be advised to start screening earlier and/or have more frequent screening.
How Can I Reduce My Cancer Risks
Healthy lifestyle choices are especially helpful in preventing both ulcerative colitis and colon cancer and help detect it early. Some of the most important choices you can make include:
- Eat a healthy diet with less red meat and processed meats, sugar, fat, soft drinks, and other processed foods. Increase fish, chicken, and protein options like cheese, cottage cheese, nuts, and beans, as well as vegetables, fruits, and whole grains. Frying, broiling, or grilling meats at high temperatures increases cancer risk.
- Maintain a healthy weight.
- Stay physically active 30 minutes to an hour of activity on most days.
- Stop smoking.
- Limit or stop drinking alcohol.
- Try to drink 100 ounces of water per day to keep your body cleansed.
- Have regular colorectal cancer screenings.
You May Like: Stomach Ulcer Pain Relief Medicine
Endoscopic Recommendations For Colorectal Cancer Screening And Surveillance In Patients With Inflammatory Bowel Disease: Review Of General Recommendations
Correspondence to: Jose María Huguet, PhD, Digestive Diseases Department, General University Hospital of Valencia, Avenida Tres Cruces, 2, 46014 Valencia, Spain.
Telephone: +34-60-6394982 Fax: +34-96-3131901
Dont Wait Until You Are 45 To Talk To Your Doctor About Screening
Reasons to get screened for colon cancer also include:
- If you are experiencing symptoms.
- If you have been diagnosed with inflammatory bowel disease .
- If your parents or immediate family members have had polyps, talk to your doctor about starting screening at an age 10 years before their polyps were discovered.
- If you have a family history of colon cancer or a genetic syndrome like Lynch syndrome or FAP .
Important! If you feel your concerns are being ignored by your current physician, dont be afraid to seek a second opinion and continue to request screening. You are your own best advocate and should feel empowered to take control of your health.
More information about screening options is available from the CDC.
Information on these pages is provided for informational purposes only. Consult your own physician before making any medical decisions.
Don’t Miss: Ulcerative Colitis Symptoms Back Pain