What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Nutritions Role In Treating Uc
Your health care provider can help you make up for these nutritional deficits by identifying foods to help control your UC symptoms and provide you a well-balanced, nutritious diet.
Certain foods or beverages may irritate your digestive tract and trigger flare ups of UC symptoms. Your health care provider will help you identify these foods, so you can avoid them and identify substitute foods that provide the same nutrients, without flare ups.
Foods more likely to trigger UC symptoms include:
-
Plant foods that contain insoluble fiber, such as fruits with skin or seeds raw green vegetables, especially cruciferous vegetables, such as broccoli or cauliflower whole nuts or whole grains and anything with a peel
-
Lactose, a sugar in dairy products, such as milk, cream, and soft cheeses
-
Sugary foods such as pastries and juices
-
Non-absorbable sugars: sugar alcohols found in sugar-free gum, candy, ice cream, and certain types of fruits/juices such as pear, peach, and prune
-
High-fat foods, including fried or greasy foods, butter, coconut, margarine, and cream
Recommended foods for UC include:
-
Refined grains, such as sourdough, potato, or gluten-free bread, white pasta, white rice, and oatmeal
Your health care provider may also recommend:
Also Check: Fasting To Heal Ulcerative Colitis
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
How Should I Begin To Find The Right Diet For My Ulcerative Colitis
Ulcerative colitis is a difficult condition to live with. Curing it is impossible: You can only hope to manage it to the best of your ability. Doctors advise eating foods that help to calm down your symptoms, so you should pay attention to what you eat and simultaneously avoid “bad” foods that aggravate your ulcerative colitis.
The food you eat is crucial to your nutrition and well-being. People with inflammatory bowel disease are frequently malnourished, and this is because ulcerative colitis often causes the following:
- Limited absorption of proteins, fats, carbohydrates, water, vitamins, and minerals
- Loss of the urge to eat
- Unintentional weight loss
- More significant nutritional needs due to the disease
Because of this, you must eat a diet that helps manage your ulcerative colitis and contains many nutrients. No one diet works for everyone that has this condition. The best way to figure out what works for you is by keeping a food journal.
To do this, you should write down what you eat every day. Then, write down all of your symptoms and their severity. From this, you will be able to tell which foods trigger or worsen your ulcerative colitis.
Be sure to never eliminate a whole food group at once, as this can often lead to a lessening of vital nutrients. Additionally, try to only add in types of food one at a time so that you can understand their impact on your body.
Don’t Miss: Can You Take Tylenol If You Have An Ulcer
How Is Colitis Treated
Medications and surgeries have both helped colitis patients. However, no medication can cure the disease. Colitis typically undergoes several changes during the illness where the patient may experience remission of symptoms where they feel better or flare-ups that cause them to relapse. One of the best ways to manage these ups and downs is to closely monitor the diet to control disease symptoms.
It’s Easy To Get The Care You Need
See a Premier Physician Network provider near you.
The foods you eat cannot cause ulcerative colitis , however certain foods can trigger and worsen your symptoms, if you have UC.
Dietary changes and good nutrition practices can help you control the symptoms and make living with UC more bearable comfortable.
Like Crohns disease, ulcerative colitis is an inflammatory bowel disease . Unlike Crohns, which can affect any part of the gastrointestinal tract, ulcerative colitis targets the colon .
UC inflames the innermost lining of your colon. As the diseases name implies, the inflammation causes ulcers.
What causes UC? One culprit may be an abnormal immune system response that mistakenly attacks the lining of the colon, causing inflammation. Genetics may also play a role. The disease affects people in certain population groups more than others such as those living in northern climates and people of Jewish descent.
Your health care provider can help you make up for these nutritional deficits by identifying foods to help control your UC symptoms and provide you a well-balanced, nutritious diet.
Recommended Reading: Sample Menu For Ulcerative Colitis
Some Types Of Fermented Food
If you are not a fan of yogurt, there are still plenty of foods that you can eat that are good sources of probiotics. These include some fermented foods like sauerkraut and kimchi.
If you are familiar with Korean food, you will most likely be familiar with kimchi, which is their version of pickled vegetables. The most common vegetables that are made into kimchi include Napa cabbage and radish. You can try to make your own at home or go to your local Asian store to buy.
It may be an acquired taste for some, but it can be paired with any type of meat.
Are Food Triggers The Only Cause Of An Ulcerative Colitis Flare
Regardless of your diet, there may be times when your ulcerative colitis symptoms seem to disappear completely for months at a time before making a dramatic reappearance. When this happens, its .
But the foods youre eating arent the only possible culprit. Emotional stress, not taking medications as prescribed, and use of certain medications, like steroids and antibiotics, can also trigger ulcerative colitis flares, according to the Cleveland Clinic.
Flares take different forms for different people, and theres no formula that predicts what will bring them on. Different people will claim a medicine or anxiety will set their symptoms off. But some people just seem to have had flares when they have flares, and you can drive yourself crazy trying to find the cause, Dr. Schwimmer says.
Read Also: Ozanimod Phase 2 Ulcerative Colitis
Lifestyle Diet In Inflammatory Bowel Disease
Topics in this Post
Inflammatory bowel disease, also known as IBD, consists of Crohn’s disease and ulcerative colitis. No specific food, diet or lifestyle causes, prevents or cures inflammatory bowel disease. And multiple factors can trigger the diagnosis.
Your diet does not cause inflammatory bowel disease, or induce a flare. However, modifying your diet can manage symptoms during a flare.
While several specialized diets may help certain patients, no plan has been proven to prevent or control inflammatory bowel disease, except for enteral nutrition, which is delivered in a nutrient-rich formula.
Keeping a food diary is a great way to manage flare-ups. A dietitian specializing in inflammatory bowel disease may recommend a particular diet based on your symptoms.
These tips may help you manage inflammatory bowel disease:
Be careful with vitamins and mineral supplements. Remember, most of your needed vitamins are obtained by eating a balanced diet. Some over-the-counter supplements can contain lactose, starch and other ingredients that can worsen your symptoms.
Besides eating a recommended diet, some supplements may be suggested for patients with inflammatory bowel disease. Talk to your health care professional about healthy levels of calcium, vitamin D, folic acid, vitamin B12, iron and zinc.
As with any health condition, a healthy lifestyle makes it easier to manage your diagnosis:
Topics in this Post
Finding The Right Uc Diet For You
For those living with ulcerative colitis, choosing the right foods to eat may feel overwhelming. If you are worried you may not be getting enough of one or more nutrients, speak with your gastroenterologist. They may test your blood for nutrient levels to find out whether you are deficient. If you are deficient in any nutrient, your doctor may recommend a safe and effective dietary supplement.
You can also request a referral to a registered dietitian who can work with you to get the most out of the nutrients in the foods youre able to eat. Working with a registered dietitian or nutritionist can also help you navigate life events, such as parties, dining out, vacations, and more. Understanding what triggers your flare-ups life stress or specific foods is important information that a food journal can help you decipher.
The good news is that for people with UC who establish a healthy and safe diet plan, sticking to it often helps them feel better and manage symptoms. Feeling pretty good today, wrote one MyCrohnsAndColitisTeam member. Ive gone lactose- and gluten-free, and symptoms have reduced a lot. Also gave up caffeine. Living on avocado!
You May Like: How Do They Treat Ulcers
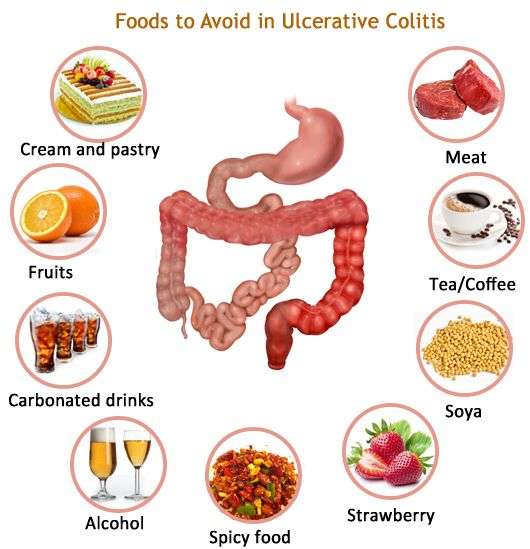
Foods That Trigger Ulcerative Colitis
Ulcerative colitis is a type of inflammatory bowel disease that occurs as the result of inflammation in the digestive tract. Some of the symptoms of ulcerative colitis may include diarrhea, rectal bleeding, rectal pain, weight loss and fatigue. Medication is the standard treatment for ulcerative colitis. However, medication wont cure the condition it will only help manage symptoms.
Avoiding the following trigger foods can also help reduce symptom flare ups:
1. AlcoholAlcohol is something that you should avoid if you have any type of inflammatory bowel disease IBD. It has a tendency to stimulate the intestines. That is why if you drink alcohol, then you are likely to suffer from diarrhea.
2. CaffeineCaffeine is a stimulant, so it isnt good for people who have Crohns disease or ulcerative colitis. You may find yourself going to the bathroom a lot if you consume caffeine. You will need to limit your consumption of tea, coffee, energy drinks and chocolate.
3. Carbonated beveragesCarbonated beverages are ones that contain dissolved carbon dioxide. This includes beers and sodas. Carbonated beverages can irritate the digestive tract. That is why they can trigger unpleasant symptoms, such as gas and bloating. Many carbonated beverages also contain sugar or artificial sweeteners.
6. Sulfur or sulfatesSulfates are foods that are naturally found in many foods. They may be artificially added to processed foods. It is estimated that 1 in 100 people has a sulfate sensitivity.
What Can I Eat During Remission

When your UC is in remission, your instinct might be to reach for foods that are normally off-limits during a flare. But its still best to stick with generally trigger-free fare.
I would advise someone to eat plenty of diverse vegetables and fruits and consider following an anti-inflammatory style diet or Mediterranean diet, says Dr. Singh.
Though, fiber, in its many forms, may be better tolerated during remission, says Freuman. Go for the raw veggies, eat the salad, have a handful of whole nuts, or leave the skin on your fruits and vegetables, she says.
That said, Freuman adds that some people find that these types of foods bother them even in remission, and thats perfectly okay. Its not worth suffering or making yourself sick to push beyond the comfortable limits of tolerance, notes Freuman.
Ultimately, she encourages her clients to eat the greatest variety of plant-based foods they can comfortably tolerate as the foundation of their diets.
Read Also: Ulcerative Colitis And Blood Clots
Read Also: Home Remedies For Dog Mouth Ulcers
Carbonated Beverages May Increase Abdominal Pain
Fizzy drinks may cause gas or bloating in some people, possibly leading to increased abdominal discomfort. Many soft drinks or carbonated energy drinks also contain caffeine, which can stimulate the intestines and worsen diarrhea, according to Mayo Clinic. Drinking sugary soft drinks can contribute to obesity as well, which raises the risk of heart disease and other health problems.
An analysis of drinks published in May 2019 in the journal Medicine found that a high intake of soft drinks was associated with an increased risk of developing Crohns disease, while a high intake of tea was associated with a lower risk of the inflammatory bowel disease. For a refreshing beverage, choose fruit-infused water or herbal iced teas.
Canned Or Cooked Seedless Skinless Vegetables And Fruits
As mentioned above, its important to avoid high-fiber fruits and vegetables during a flare-up. However, its still important to give your body the nutrients it needs. For this reason, youll want to make sure that you eat plenty of cooked or steamed fruits without skins or seeds. You can also safely eat pureed soups and sauces made from vegetables.
Also Check: Can Ulcerative Colitis Cause Positive Ana
The Nutritional Impact Of Uc
Changes in diet and nutrition are one part of a multifaceted approach for treating ulcerative colitis and other IBD conditions. Your doctor also will likely prescribe medication. In more severe cases, surgery may be needed, to repair or remove damaged portions of the colon.
Malnutrition, dehydration, and weight loss are major health risks of UC. When the colon becomes inflamed and ulcerated, its less able to absorb fluids and nutrients needed to help sustain your body.
Diarrhea, a symptom of UC, also increases loss of fluids and nutrients, such as sodium, potassium, magnesium, phosphorus, and zinc.
In severe cases, people with UC may need IV fluids to replace these lost nutrients and fluids.
Other UC symptoms, such as abdominal pain and nausea, can further rob you of nutrition as they reduce your appetite, so you consume fewer calories and nutrients.
Ulcerative Colitis Diet: Food Preparation And Meal Planning
While the idea of an elimination diet or restricting your intake of fiber, fat or other trigger foods may seem daunting, meal planning and preparing your food ahead of time can take some of the stress out of eating in a flare up. If your appetite is impacted as well, you can batch cook and eat what you want of a larger pre-prepared meal when you feel like eating, rather than preparing yourself a whole new meal from scratch.
The Crohns and Colitis Foundation indicates that rates of depression and anxiety are higher in those with IBD, so anything that can reduce stress for those with ulcerative colitis might be helpful for managing mental health. As such, pre-planned meals based around particular dietary needs can make the day-to-day experience of ulcerative colitis slightly less stressful, and may make the experience of a flare up more bearable.
This article is for informational purposes only and is not meant to offer medical advice.
You May Like: Ulcerative Colitis And Menstrual Cycle
Food Prep And Meal Planning
Although there is no cure for UC, meal planning and prepping food ahead of time can help people living with UC limit foods that trigger their symptoms.
Planning meals, snacks, and even your hydration efforts in advance gives you control over everything youll be consuming.
With preparation, you can avoid making quick decisions when youre hungry or thirsty that could result in a flare-up.
Taking the time to plan out your meals and read nutrition labels may take a couple of hours initially, but it can save tons of time throughout the week overall. Helpful steps include:
- buying ingredients in bulk
- cooking in batches
- preportioning your meals before storing them in the fridge or freezer, making them easier to reheat and eat
Not only will you have your meals prepared ahead of time, but youll also help limit food triggers, allowing you to feel better and be more productive overall. Buying and planning your snacks ahead of time is a good way to avoid reaching for trigger foods, too.
Additionally, because frequent diarrhea from UC can cause you to lose more fluid than you put into your body, planning water intake can help you avoid dehydration.
Constipation can be a symptom for some individuals, and their dietary needs may differ.
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohn’s disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
Also Check: Symptoms Of Ulcer In Female
Ulcerative Colitis Foods To Avoid
In general, its best to avoid foods that are low in fiber, as a protective measure. However, if you are experiencing a flare-up, youll want to eat low-fiber foods – this will help your colon recover more quickly from a UC attack. Once you are feeling better, returning to those high-fiber foods will be better for your gut microbiome. The following list of foods will be foods that you should avoid to help minimize your symptoms during a flare-up. Remember to reintroduce high-fiber foods slowly once your symptoms have resolved. Here are some Ulcerative Colitis foods to avoid during a flare-up: