Symptoms: Pain And Severity
The most frequently observed symptom in UC is the presence of blood in stools . It may be associated with mucus discharges, diarrhea, abdominal pains, etc. Severe flare-ups may result in weight loss, severe fatigue and fever.
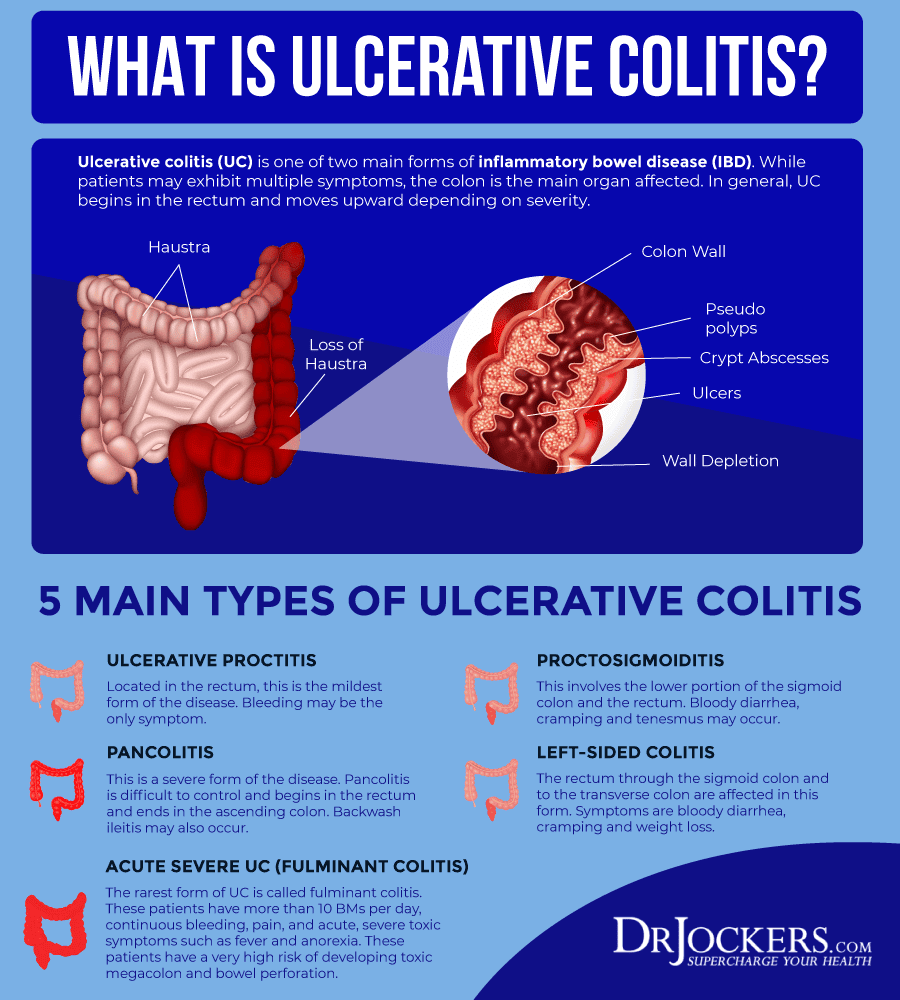
In almost one third of cases, the disease starts with lesions limited to the rectum, while one third of the patients experience inflammation of the whole large intestine from the start . After 20 years of progression, this pancolitic form of the disease is found in 50% of the patients.
Extra-intestinal symptoms may appear: in the joints , on the skin , sometimes in the eyes or the liver.
In children, ulcerative colitis leads to malnutrition, which may cause severe failure to thrive.
A number of not rare and sometimes inaugural complications add burden to the medical and surgical care of these patients: severe colitis, fistula, stenosis, cancerous degeneration with a risk 18 times higher than in general population after 20 years of progression of a pancolitic form of the disease.
Pain Prevalence And Associated Factors
Slightly more than half of the entire group endorsed at least some pain over the previous two weeks before or during their index visit, with 108 people reporting a SIBDQ Pain Score of at least 4 . Considering the emphasis on frequency rather than severity, we correlated the SPS with the pain severity rating of the Colitis Activity Index, which showed a significant relationship between the two measures . Significantly more women than men described their pain as more frequent . Of note, 16 patients used opioids at the time of their index visit. Abdominal discomfort was the main reason for opioid use in 6 of these individuals, with the remaining patients receiving pain medications for joint, back, bone or muscle pains or chronic pancreatitis . In the remaining patients, no reason for opioid therapy could be identified. Opioid use was significantly more common in patients rating their pain as frequently or constantly present compared to those with no abdominal pain .
Abdominal Pain Prevalence in UC Patients with SIBDQ Scores. The histogram shows the distribution of pain scores, which are inversely related to pain frequency. The insert defines the fraction of patients with and without pain.
Whats A Good Plan To Manage Uc Cramping
Monitor your medications. Talk to your doctor about any prescription, over-the-counter, or herbal medications youre taking. Iron deficiency is common with UC, but oral iron supplements have been shown to increase the risk of inflammation and cramping. Some antibiotics and pain relievers, such as ibuprofen, may also increase flare-ups and cramping.
Review your diet.Keep a food diary and note the connection between the foods you eat and your UC symptoms. In general, its smart to stay away from processed foods and those high in saturated fat and sugar. High-fiber foods and dairy products can also cause UC cramping, but check with your doctor before eliminating foods from your diet, to ensure youre getting the nutrients you need.
Eat frequent, small meals. Instead of two or three large meals, eat four to six smaller meals spaced more closely throughout the day. Also, take your time while eating and chew thoroughly.
Skip caffeine and carbonated drinks. Caffeine can cause gas, intensifying abdominal cramping. It is also a stimulant, which can make cramping and diarrhea worse.
Drink enough water. People with UC may be at increased risk of dehydration, so be sure to drink plenty of H2O. A good rule of thumb, according to the Crohns and Colitis Foundation, is to aim for about 64 ounces or eight 8 oz glasses per day.
Also Check: Ulcerative Colitis Back Pain Treatment
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
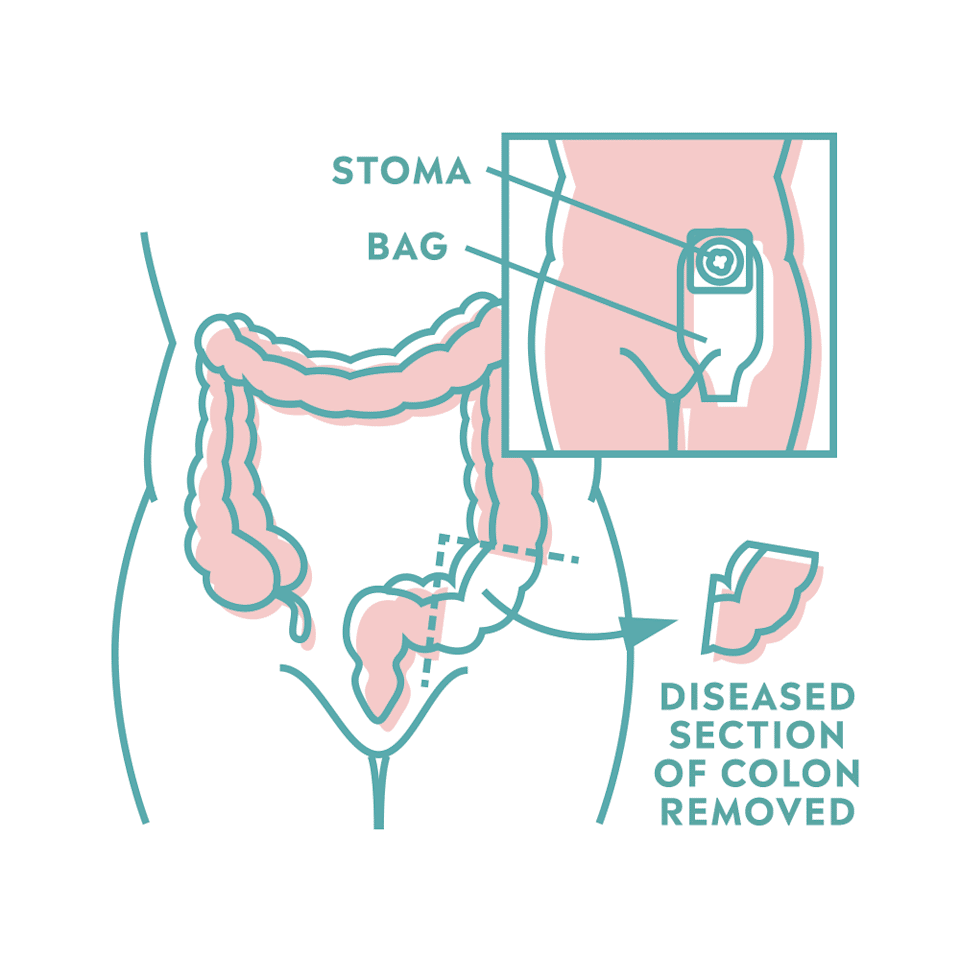
Surgery to remove the entire colon eliminates the risk of colon cancer.
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Also Check: Ulcerative Colitis Mouth Sores Pictures
How Is Acute Severe Ulcerative Colitis Treated
ASUC is a challenging condition to treat. Once youâre admitted to the emergency room, youâll get a series of tests, including blood tests, stool tests, and an exam of your bowel called a sigmoidoscopy. Youâll also get intravenous fluids to boost hydration.
The average hospital stay for ASUC treatment ranges from 4.6 to 12.5 days. During this time, your health care providers may include a gastroenterologist, colorectal surgeon, dietitian, pharmacist, and stomal therapist. The goal of hospitalizing you is to end the flare, get your symptoms under control, and put the disease into remission. Your doctors will want to make sure that rectal bleeding and diarrhea have stopped and normal bowel movements have returned. Rehospitalization is common.
Intravenous steroid medications are the most common treatment for ASUC. For 30% to 40% of ASUC patients, steroid treatments donât work â and taking steroid medications for more than 10 days increases your risk of complications.
If the steroids donât help within 3 to 5 days, your health care team will start âmedical rescue therapyâ with immunosuppressive drugs like cyclosporine or infliximab.
You might get an operation to remove part of your colon, called a colectomy, if your ASUC doesnât respond to steroids, immunosuppressants, or other medical treatments.
You May Like: How To Lose Stomach Fat Extremely Fast
Ulcerative Colitis And Colonoscopy
Doctors can use a colonoscopy to diagnose UC or determine the severity of the condition.
Before the procedure, a doctor will likely instruct you to reduce solid foods and switch to a liquid-only diet. Then youll fast for a period of time before the procedure.
Typical colonoscopy prep involves taking a laxative the evening before the procedure, too. This helps eliminate any waste still in the colon and rectum. Doctors can examine a clean colon more easily.
During the procedure, youll lie on your side. Your doctor will give you a sedative to help you relax and prevent any discomfort.
During the exam, the doctor will look for signs of inflammation and check for precancerous growth called polyps. The doctor may also perform a biopsy. The tissue can be sent to a laboratory for further examination.
If youve been diagnosed with UC, a doctor may conduct periodic colonoscopies to monitor inflammation, damage to your intestines, and healing progress.
These symptoms are sometimes associated with UC complications.
If you havent been diagnosed with UC, see a doctor if you experience multiple symptoms of the condition. They can help determine whether you may have UC or another bowel disease.
UC is a chronic condition. The goal of treatment is to reduce the inflammation that causes your symptoms to prevent flare-ups and have longer periods of remission.
You May Like: What Not To Eat When You Have Ulcerative Colitis
Clinical Presentation And Differential Diagnosis
Figure 3Ulcerative colitis phenotypes by Montreal Classification71
Symptoms and treatment strategy can differ based on extent of disease. Illustration by Jill Gregory. Printed with permission of ©Mount Sinai Health System.
Extraintestinal manifestations can occur in about a third of patients with ulcerative colitis, and up to a quarter might have extraintestinal manifestations before inflammatory bowel disease diagnosis .75,76 Peripheral arthritis appears to be the most common extraintestinal manifestation primary sclerosing cholangitis and pyoderma gangrenosum are more common in ulcerative colitis than in Crohns disease.75,76 The risk of venous thromboembolism in patients with inflammatory bowel disease is increased three to four times, and is greater when the patient is admitted with a flare or being treated with corticosteroids.7780 Clinicians should have a high index of suspicion for venous thromboembolism, and hospitalised patients with ulcerative colitis should be prescribed venous thromboembolism prophylaxis.81
When To Call A Professional
New or changing symptoms often mean that additional treatment is needed. People who have ulcerative colitis should be in frequent contact with their physicians.
Common symptoms that require a doctor’s immediate attention are:
- Fever, which could indicate infection or a ruptured intestine
- Heavy bleeding from the rectum
A serious, but uncommon, complication is called toxic megacolon. This results when the colon inflammation is so severe that it stops the colon’s motion. Megacolon causes the abdomen to swell. This can cause vomiting or severe abdominal pain and bloating. Megacolon requires emergency treatment, often surgery.
Also Check: Holistic Medicine For Ulcerative Colitis
Inflammatory Bowel Disease And Colitis
Ulcerative colitis and Crohns disease are the two types of inflammatory bowel disease that cause colitis. Crohns disease and ulcerative colitis are considered autoimmune diseases .
- Ulcerative colitis always begins in the rectum and may spread to the rest of the rest of the colon, spreading from the rectum to the sigmoid, descending, transverse, and finally the ascending colon and cecum in that order. Ulcerative colitis is considered an autoimmune disease, and symptoms include abdominal pain, and bloody, diarrheal bowel movements.
- Crohns disease may occur anywhere in the gastrointestinal tract , including the esophagus, stomach, small intestine, and colon. In Crohns disease, there may be skip lesions, that is, abnormal segments of the GI tract interspersed with normal segments.
Both Crohns disease and ulcerative colitis may have other organ systems involved in addition to the gastrointestinal tract.
Either collagen or lymphocytes infiltrate into the layers of the wall of the colon, presumably as a result of inflammation. This is an uncommon illness and maybe an autoimmune disease. Diarrhea often is watery, and no blood is present in the stool.
What You Can Do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there’s anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you’re experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements that you’re taking. Be sure to let your health care provider know if you’re taking any herbal preparations, as well.
- Ask a family member or friend to come with you. Sometimes it can be difficult to remember all the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
Your time is limited, so preparing a list of questions ahead of time can help you make the most of your time. List your questions from most important to least important in case time runs out. For ulcerative colitis, some basic questions to ask include:
Read Also: Prednisone For Ulcerative Colitis Dosage
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
Recommended Reading: Ulcerative Colitis Increased Risk Of Colon Cancer
Historical Information Important In The Diagnosis Of This Problem
1. When did the pain start or how long have you had the RLQ pain?
Acuity, intensity and duration of pain may be helpful in assessing severity of disease. A sudden onset of pain suggests a serious intra-abdominal event such as an organ perforation or Ischemia or obstruction of a small tubular structure .
A more gradual onset of symptoms suggests an infectious or inflammatory cause , or obstruction of a large tubular structure .
2. Has the pain changed location?
The pain of acute appendicitis may start in the periumbilical area and then a few hours later localize in the RLQ as the peritoneum overlying the inflamed appendix gets affected .
3. Any recent trauma to this area? Any recent abdominal surgery?
Rule out trauma as the cause of pain.
4. Have you ever had this problem before?
A positive response would suggest a chronic intermittent problem e.g. inflammatory bowel disease , diverticulitis, nephrolithiasis.
5. Any history of diverticulitis, Crohns disease or ulcerative colitis, hernias or nephrolithiasis? Any family history of IBD? Any prior abdominal surgeries specifically appendectomy, bowel surgery and in females prior history of salpingo-oopherectomy?
This line of specific questioning helps rule out certain possibilities and make some more likely.
Any intra-abdominal medical devices e.g. ventriculoperitoneal shunts presence raises index of suspicion for intra-abdominal infection .
6. Is the pain dull and constant or is it colicky in nature?
12. Any fever or chills?
Favorite Orgs For Essential Uc Info
CCF is the leading nonprofit organization dedicated to finding the cure for UC and Crohns. The organization is at the forefront of IBD research and works to educate, empower, and support individuals afflicted with these diseases. Find your local chapter by visiting the CCF website.
This research institute at Virginia Mason in Seattle is one of the few establishments devoted to finding the causes of autoimmune diseases like UC and their cures. Benaroya has already helped advance research in more than 80 diseases of the immune system. The autoimmune life blog provides information on community events and personal stories from patients living with an autoimmune disease.
Read Also: Nursing Care Plan For Pressure Ulcer Prevention
How Is Ulcerative Colitis Different From Crohns Disease
Ulcerative colitis is different from other inflammatory bowel diseases like Crohns disease. Crohns can affect any area of the gastrointestinal tract, including the small intestine and colon. Ulcerative colitis, on the other hand, affects only the colon. The inflammation involves the entire rectum and extends continuously up the colon. There are no normal areas of the intestine between the areas of ulceration. In Crohns, the inflamed areas are scattered and can affect the entire thickness of the bowel wall.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Don’t Miss: Dr Reckeweg Medicine For Ulcerative Colitis
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I cant bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I cant fully stand upright sometimes for a minute or so. Its frustrating.
Also Check: Silver Dressing For Leg Ulcers