Diet Recommendations For Ulcerative Colitis Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
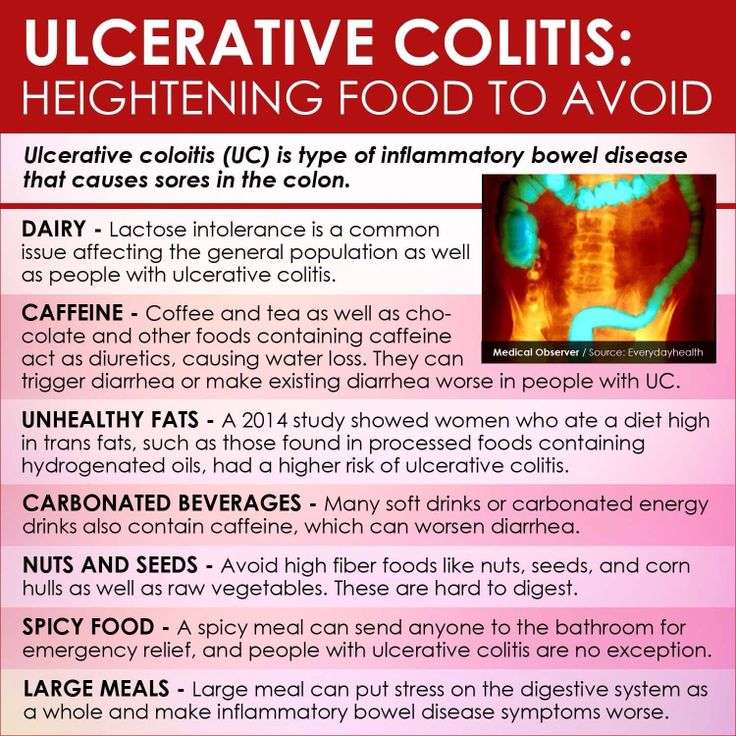
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages.
- Try incorporating more omega-3 fatty acids in your diet. These fats may have an anti-inflammatory effect. They are found in fish, including salmon, mackerel, herring and sardines.
- Patients often find that smaller, more frequent meals are better tolerated. This eating pattern can help increase the amount of nutrition you receive in a day.
- Consider taking nutritional supplements if appetite is poor and solid foods are not tolerated well .
Eating When You Are In Remission
While theres no cure for UC, you may experience periods of remission. During this time, youll be symptom-free and your UC wont interfere with your daily life.
Theres no definitive way to avoid flare-ups forever, but you can prolong your remission periods by maintaining a diverse and nutrient-rich diet that does not include trigger foods.
To stay symptom-free, it may be helpful to follow one of the diets that other individuals with UC find successful, as well as introduce new foods slowly and stay hydrated.
However, its important to consult with your doctor or dietician before making any changes to your diet.
Some foods that may help keep you feeling good and hydrated during remission
Ulcerative Colitis Crohns Disease Or Something Else
The colon, also known as the large intestine, has three parts or section: ascending colon , transverse , descending colon , and the sigmoid colon just before the rectum.
Ulcerative colitis symptoms in each person will be different depending on where inflammation occurs and how bad it is. The most common symptoms include:
There are common complications that tend to come with UC, even though they are not actually a direct result of this chronic health condition. Fever, fatigue, and anemia are perhaps the most common additional symptoms. Additionally, inflammation beyond the colon often shows up as skin sores, skin rashes, mouth sores, joint pain, red and painful eyes, and sometimes even liver disease.
While both are referred to as inflammatory bowel disease or IBD, and Ulcerative colitis is related to Crohns disease, they are still different. Crohns disease, unlike ulcerative colitis, is not limited to the colon and is a chronic inflammatory disease of the intestines or the entire GI tract. Crohns often affects the small intestine and colon although occasionally it, too, is limited to the colon.
Read Also: Mouth Ulcer On Tongue Causes
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Do Certain Desserts Cause Flares
Diets high in sugar and fat have been associated in multiple studies with worsening inflammation. These ingredients are commonly present in trigger foods, which are items that can make your ulcerative colitis symptoms worse and cause a flare.
One study of people with ulcerative colitis found that eliminating these foods helped people experience symptom remission:
- Corn
- High-fructose corn syrup
- Packaged or convenience foods
Dairy products have also been shown to make ulcerative colitis worse, so a lactose-free diet may be beneficial.
Many desserts do include these ingredients, so its important to know what causes your flares so you can avoid them when you have dessert.
Recommended Reading: Best Probiotic For Ulcerative Colitis
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
When Should You See A Doctor About Ulcerative Colitis Food Triggers
According to Dr. Schwimmer, seeing a doctor at the first sign of ulcerative colitis symptoms is your safest bet, especially if youve never been formally diagnosed. Concerning, unexplained symptoms like bloody stool, diarrhea, and abdominal cramping shouldnt be ignored, because even if its not ulcerative colitis, you might be dealing with something else that needs proper treatment.
After youve been diagnosed, your doctor might recommend making diet adjustments as a part of your ulcerative colitis treatment plan. But ultimately, FDA-approved medications, which help control the inflammation that sets off GI pain, are going to be the main course of treatment that your doctor suggests for the long haul of this chronic condition.
There is no secret treatment for inflammatory bowel disease. Everybodys looking for the secret pills. What diet can I follow? What supplement can I take? What probiotic can I take? Unfortunately, it just doesn’t exist, Dr. Schwimmer says. But the medicines we have work and they work better than anything else.
Thats why doctors who specialize in IBD caution that self-treatment with diet is not enough. If you arent working within the framework of a plan that includes proven, FDA-approved medication, you are at a higher risk of complications from your ulcerative colitis, including malnutrition.
Recommended Reading: Icd 10 Stage 3 Pressure Ulcer Sacrum
What Desserts Can You Eat With Ulcerative Colitis Recipe Ideas
Just about everybody enjoys a sweet treat now and then, but if youre living with ulcerative colitis, it can be tough to decide what to eat and when. Can you eat dessert at all? If so, which desserts are best?
In this article, youll find some ideas of what to keep in mind when you look at dessert options, along with resources on where to find recipes. Doing your research and learning from others is a great way to have your cake and eat it too.
Foods To Eat During An Ulcerative Colitis Flare
Avoiding certain foods is only half the battle. Heres how to get the nutrients you need during an ulcerative colitis flare.
Jeff Wasserman/Stocksy
If you have ulcerative colitis, you may already know which foods worsen your flares. But figuring out what to include in your diet is equally important, because the right foods will provide you with key nutrients without aggravating your symptoms.
Most experts recommend that you limit your fiber intake when youre having an ulcerative colitis flare. A general rule is to replace high-fiber foods, such as nuts, seeds, and raw fruits and vegetables, with more easily digestible fare. Here are eight foods to eat during an ulcerative colitis flare and the reasons they can help.
1. Applesauce: Since your gastrointestinalsystem is experiencing a lot of irritation during a flare, you may want to stick to soft, easily digestible foods like applesauce. Be sure to choose an unsweetened variety though, because added sugar can cause more inflammation. You can also make your own sugar-free applesauce by cooking peeled, sliced apples with some water and then pureeing the mixture.
3. Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K. Just make sure the vegetablesare thoroughly cooked until they can be mashed with a fork, Szeles says so that any potentially irritating fiber is broken down.
Additional reporting by Nina Wasserman
Read Also: How Do They Test For Ulcerative Colitis
Diet Recommendations For Crohn’s Disease Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- If you have strictures, it is especially important to avoid nuts, seeds, beans and kernels.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages. Cold foods may help reduce diarrhea.
- If you have lactose intolerance, follow a lactose-free diet. Lactose intolerance causes gas, bloating, cramping and diarrhea 30 to 90 minutes after eating milk, ice cream or large amounts of dairy. A breath hydrogen test may confirm suspicions of lactose intolerance.
- If you have oily and foul-smelling stools, you may have fat malabsorption. Treat fat malabsorption by following a low-fat diet. Discuss these symptoms with your doctor or nutritionist.
- Smaller, more frequent meals are better tolerated and can maximize nutritional intake.
- If your appetite is decreased and solid foods not tolerated well, consider taking nutritional supplements .
Foods To Eat During Ulcerative Colitis Flares
A bland diet is best during periods of active ulcerative colitis, when you may experience abdominal discomfort, blood in your stool, loss of appetite, fatigue, weight loss, vomiting, nausea, abdominal pain, and diarrhea. A safer diet during flares might include dry toast, applesauce, and white rice. Although some foods are more likely to be safe for those with UC, individual experiences can vary, especially during flares.
Here are some safer foods to try during ulcerative colitis flares:
- Low-fiber refined grains, such as oatmeal, potatoes, and sourdough bread
- Well-cooked vegetables that are easier to digest
- Vegetable broth, which can be added to grains like rice for additional nutrients
- Fruits or vegetables that contain more soluble fiber than insoluble fiber, such as bananas, carrots, and apples
- Bland protein, such as nut butters, eggs, tofu, and chicken
Diarrhea specifically raises concerns for loss of nutrients, such as potassium, sodium, magnesium, and phosphorus, through bodily fluids. If you choose to drink an electrolyte beverage, choose low sugar versions such as G2, Propel, or BodyArmor Lyte. You can also cut regular Gatorade or BodyArmor with water, diluting it by half.
Don’t Miss: How To Prevent Ulcers In The Stomach
What Foods Should You Eat With Ulcerative Colitis
If you have Ulcerative Colitis, very minor changes to what you eat can make a BIG difference in your symptoms. Consider keeping food logs or adjusting foods that trigger your symptoms. You may also want to work with your doctor or dietitian to work through an elimination diet. Generally, you should try to:
In terms of specific food recommendations, go with these:
| Food Type |
|---|
|
During a flare up, you many find it more comfortable to eat bland, soft food, otherwise limiting spicy foods. During periods of remission, you should eat all of your usual items with the omission of known offenders.
Are Food Triggers The Only Cause Of An Ulcerative Colitis Flare
Regardless of your diet, there may be times when your ulcerative colitis symptoms seem to disappear completely for months at a time before making a dramatic reappearance. When this happens, its .
But the foods youre eating arent the only possible culprit. Emotional stress, not taking medications as prescribed, and use of certain medications, like steroids and antibiotics, can also trigger ulcerative colitis flares, according to the Cleveland Clinic.
Flares take different forms for different people, and theres no formula that predicts what will bring them on. Different people will claim a medicine or anxiety will set their symptoms off. But some people just seem to have had flares when they have flares, and you can drive yourself crazy trying to find the cause, Dr. Schwimmer says.
Recommended Reading: What Can I Do For Ulcers In My Stomach
Ulcerative Colitis: This Is Why You’re Here Right
- Why did you get Ulcerative Colitis? The short answer is that scientists still don’t know. Genetics are a major risk factor, but some people without a family history develop the condition
- Ulcerative Colitis is caused by an autoimmune response from your body
- Your symptoms may include:
- GI: loose and urgent bowel movements, bloody stool, abdominal pain and cramps, persistent diarrhea
- Non-GI: appetite loss, weight loss, nausea, low energy, anemia
- There are flares and periods of remission throughout disease course UC is different from other types of colitis because tiny ulcers form, causing long term inflammation
Can Ulcerative Colitis Cause Rash And Skin Irritation
Swollen and painful areas of skin are common and affect up to 15 percent of individuals with UC. In general, skin irritation and rashes will get worse during a flare and resolve during periods of remission. These rashes oftentimes fluctuate in-line with the inflammation throughout your entire body. While most skin irritation and rashes are caused by Ulcerative Colitis inflammation, general UC symptoms do not always cause the irritation and rashes.
There are numerous skin conditions associated with Ulcerative Colitis, many of which are caused by auto-immune functions:
- Erythema nodosum
- Acne
- Hives
Learn more about these conditions and how to treat them in our full discussion on Ulcerative Colitis and skin irritation / rash.
You May Like: How You Know If You Have A Stomach Ulcer
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
What Are The Basics Of A Healthy Diet For People With Uc
This whole UC situation would be a lot easier if it came with an instruction manual for eating. But even though were not quite as lucky as that, there are plenty of to help you along the way.
Case in point: Doctors and dietitians generally discourage people with UC from adopting fad diets like Keto or Paleo, which may do more harm than good because you may not get the nutrients you needor you may get too much of what you dont need. On the what-you-can-eat side, they generally recommend following a plant-based, Mediterranean diet . But what you eat during a flare and what you eat the rest of the time likely wont be exactly the same. Here are some things to keep in mind:
Also Check: What Are The 4 Stages Of Pressure Ulcers
Ulcerative Colitis Foods To Avoid
In general, its best to avoid foods that are low in fiber, as a protective measure. However, if you are experiencing a flare-up, youll want to eat low-fiber foods – this will help your colon recover more quickly from a UC attack. Once you are feeling better, returning to those high-fiber foods will be better for your gut microbiome. The following list of foods will be foods that you should avoid to help minimize your symptoms during a flare-up. Remember to reintroduce high-fiber foods slowly once your symptoms have resolved. Here are some Ulcerative Colitis foods to avoid during a flare-up:
How A Professional Can Help
Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
You May Like: Foods That Cure Ulcerative Colitis
Read Also: Do Enemas Help Ulcerative Colitis
Keeping A Food Journal
Everyones body is different, so its possible for two people who have UC to have different trigger foods.
Logging what you eat throughout the day and when digestive issues occur can help you and your doctor narrow down your personal food triggers.
A food journal can be especially helpful if youre trying a new diet.