Warning Disclaimer Use For Publication
WARNING: Please DO NOT STOP MEDICATIONS without first consulting a physician since doing so could be hazardous to your health.
DISCLAIMER: All material available on eHealthMe.com is for informational purposes only, and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified healthcare provider. All information is observation-only. Our phase IV clinical studies alone cannot establish cause-effect relationship. Different individuals may respond to medication in different ways. Every effort has been made to ensure that all information is accurate, up-to-date, and complete, but no guarantee is made to that effect. The use of the eHealthMe site and its content is at your own risk.
If you use this eHealthMe study on publication, please acknowledge it with a citation: study title, URL, accessed date.
Peptic Ulcer Disease Or Gastritis
When the protective mucus that lines the stomach deteriorates due to the overproduction of acid, open sores may form in the digestive tract. These open sores are called ulcers. Ulcers may become agitated and inflamed due to bacteria or overuse of anti-inflammatory drugs. Symptoms of PUD include nausea, vomiting blood, unintentional weight loss or suppressed appetite, bloody or tarry stools. Peptic ulcer disease treatment should be discussed with your Gastroenterologist.
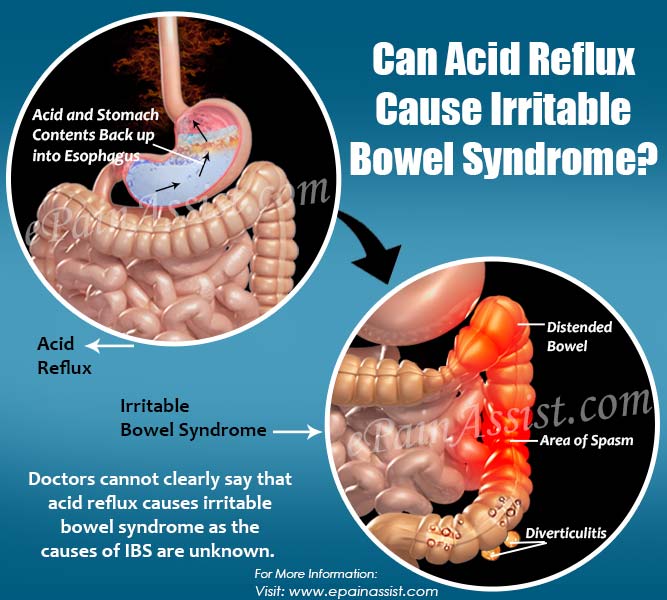
What Are The Causes Of Acid Reflux
Heartburn is normally caused by lifestyle choices and what you put into your body. More specifically.
- Eating large meals or lying down right after a meal
- Being overweight or obese
- Eating a heavy meal and lying on your back or bending over at the waist
- Snacking close to bedtime
- Eating certain foods, such as citrus, tomato, chocolate, mint, garlic, onions, or spicy or fatty foods
Recommended Reading: How Severe Is Ulcerative Colitis
Add A Comment7 Comments
I recently had a biopsy that revealed Collagenous Colitis. I also have reflux. I tested negative for H-Pylori. However, I did show on a lower GI test an enormous amount of Dysbiotic/ overgrowth bacteria and very low good bacteria. Basically, SIBO . I also have a high gluten intolerance based upon my Secretory IgA which my health practitioner believes allowed gut permeability causing the Colitis. So, perhaps this is something you may also have going on from what I hear you saying. Maybe you should get tested for SIBO.
My daughter had similar issues. She was diagnosed with Celiac. You may have gluten sensitivity at the least.
Hi,I have the exact same problem as yours. The order is different though. I first had chronic diarrhea which was eventually diagnosed as microscopic collitis, then I started having GERD and nausea. My dr seems to imply the gerd episodes are stress related…I am interested in looking at alternative/natural remedies to address the problem. I eat very carefully but that is having no affect whatsoever. The dr also thinks that is not the solution for me . Also do yoga regularly.So theoretically I am doing all the right things but am still not going through a particularly bad episode. At this point I am pretty desperate to try anything.
Pat provided you with some wonderful information, and I wanted to add one resource for the “holistic” approach that you are looking for.
2. Have you sought the care of a homeopathic physician?
Take care,
What Are The Complications Of Ulcerative Colitis
Colon Cancer
Although most patients with ulcerative colitis will not develop colon cancer, patients with ulcerative colitis are at a 2 to 5 fold increased risk of developing colon cancer compared to persons without ulcerative colitis. Researchers believe the increased risk of colon cancer is related to chronic inflammation in the colon. In order to detect colon cancer at an early stage, most patients with ulcerative colitis will need to undergo colonoscopies on a regular interval that is more frequent than for patients without ulcerative colitis. The risk of colon cancer may be even higher in individuals who have a condition of the liver called primary sclerosing cholangitis or with family members who have had colon cancer. All patients with ulcerative colitis should discuss the timing and frequency of colonoscopy with their gastroenterologist.
Surgery
Patients with ulcerative colitis may have symptoms in parts of their bodies outside of the digestive system.
Joints
There are forms of arthritis and back pain that are related to ulcerative colitis. Some of these conditions improve with medications for the digestive symptoms of ulcerative colitis. The use of over-the-counter pain medications such as ibuprofen, naproxen, and aspirin may increase the symptoms of ulcerative colitis. Patients with ulcerative colitis should speak with their gastroenterologist before using these medications.
Eyes
Skin
Other Complications
Read Also: Is Coconut Good For Ulcerative Colitis
Tests To Evaluate For Acid Reflux Disease
Upper Endoscopy: This test involves passing a thin flexible tube through the mouth into the esophagus, stomach and the beginning of the small bowel to examine for abnormalities. The tube has a light and a camera at the tip and the lining of the digestive tract is directly visualized. The test is performed using sedation. It is the best test to identify injury in the upper GI tract and Barretts esophagus.
Upper GI Series: This test involves drinking a liquid barium mixture. The radiologist uses a fluoroscope to watch the barium as it travels down the esophagus and into the stomach. The patient is asked to move into various positions on the X-ray table while the radiologist watches the GI tract and takes X-rays.
Esophageal Manometry or esophageal PH: Esophageal manometry involves passing a small flexible tube through the nose into the esophagus and stomach in order to measure pressures and function of the esophagus. The acid level in the esophagus can be measured over a 48-hour period by attaching a capsule to the lining of the esophagus.
Foods That Fight Acid Reflux And Heartburn
You are using an outdated browser. Please upgrade your browser to improve your experience.
Heartburn can do more damage than just making you feel bad. These tips can help you fight heartburn.
The symptoms of acid reflux and heartburn can range from mild to severe. One person may experience belching and discomfort. Someone else can experience chest pain, regurgitation, and intense coughing. Of course, we all have access to antacids and over-the-counter medications, but those arent always a long-term solution. Some foods can help soothe and relieve the discomfort from heartburn and acid reflux.
Read Also: Surgical Management Of Ulcerative Colitis Ppt
Drinking In Moderation Is Fine If You Have Uc
If you like to have a glass of wine or beer with family and friends over a heated fall football match or a festive holiday dinner, you probably dont need to worry about your UC symptoms flaring. Theres no evidence that alcohol increases UC flares, Dr. Hong says . If boozing is a trigger for you, stick to alcohol-free versions of your top tipples.
Fatigue Is A Normal Part Of Ulcerative Colitis
I learned, most importantly, that I should accept feeling tired as a normal part of life. The sentiment that I need to always be productive is unrealistic. In the past, I drank caffeinated beverages to try and reach that impractical standard.
After quitting caffeine, I learned to listen to my bodys natural energy cycle and plan accordingly. For example, I usually reach an afternoon lull after lunch. I now plan less busy tasks around that time of day, knowing that I will not be at peak performance.
What about you all? Do you find yourself extra sensitive to caffeine after being diagnosed with UC or IBD? What alternatives do you have to stay awake and keep reliable energy levels?
Also Check: Liver Disease Associated With Ulcerative Colitis
What Is The Outlook For Someone With Ulcerative Colitis
Ulcerative colitis can be managed with treatment. It generally wont alter the life expectancy of most people.
Most people with UC experience acute flares of symptoms during their lifetime. But with treatment, the disease can enter remission, during which symptoms go away.
Remission may last for weeks or even years. The longer the period of remission, the better a persons general health becomes.
Dr. Saurabh Sethi is a board certified physician specializing in gastroenterology, hepatology, and advanced interventional endoscopy. In 2014, Dr. Sethi completed his gastroenterology and hepatology fellowship at Beth Israel Deaconess Medical Center at Harvard Medical School. Soon after, he completed his advanced endoscopy fellowship at Stanford University in 2015. Dr. Sethi has been involved with multiple books and research publications, including over 30 peer-reviewed publications. Dr. Sethis interests include reading, blogging, traveling, and public health advocacy.
Your First Line Of Treatment Unprocessed Foods And Probiotics
Ultimately, the answer to heartburn and acid indigestion is to restore your natural gastric balance and function. Eating large amounts of processed foods and sugars is a surefire way to exacerbate acid reflux as it will upset the bacterial balance in your stomach and intestine. Instead, youll want to eat a lot of vegetables and other high-quality, ideally organic, unprocessed foods. Also, eliminate food triggers from your diet. Common culprits here include caffeine, alcohol, and nicotine products.
Next, you need to make sure youre getting enough beneficial bacteria from your diet. This will help balance your bowel flora, which can help eliminate H. pylori bacteria naturally without resorting to antibiotics. It will also aid in proper digestion and assimilation of your food. Ideally, youll want to get your probiotics from fermented foods. If you arent eating fermented foods, you most likely need to supplement with a probiotic on a regular basis. Ideally, youll want to include a variety of cultured foods and beverages in your diet, as each food will inoculate your gut with a variety of different microorganisms. you can easily make at home include:
- Fermented vegetables
Recommended Reading: Can Excedrin Cause Stomach Ulcers
Inflammatory Bowel Disease Treatment
There is currently no known cure for either ulcerative colitis or Crohns disease. Treatments involve medications to relieve symptoms and dietary changes to prevent the problems from returning.
About one in five people with ulcerative colitis may require surgery to remove any badly affected section of the colon. People with Crohns disease will often need surgical procedures to alleviate the damage caused to their digestive system.
Book an appointment for private inflammatory bowel disease treatment at Digestive Health UK.
What Are The Symptoms Of Ulcerative Colitis
Although the cause of ulcerative colitis is unknown, the effects of ulcerative colitis on the body are becoming better understood. In ulcerative colitis, the body’s own immune system is overactive and results in inflammation in the colon. This may be a response to the bacteria normally found in the colon, or “gut flora.” The persistent inflammation results in the damage and ultimately the symptoms of ulcerative colitis. Most medications for ulcerative colitis work by decreasing or “turning down,” the immune system to reduce the inflammation and damage in the colon. More recent medications target very specific molecules to decrease inflammation. There is currently one medication FDA approved to target a molecule called tumor necrosis factor to treat ulcerative colitis. For more information on the medications for ulcerative colitis, see Medications.
The most common symptoms of ulcerative colitis relate to inflammation in the colon, such as diarrhea, bloody stools, and abdominal pain. These symptoms may also be seen in other medical conditions and are not diagnostic of ulcerative colitis. Most patients can have at least partial if not complete relief of these symptoms with medications, which we call “remission.” However patients may have symptoms return periodically, or “flare,” over time even if they are taking their medications.
Don’t Miss: Foods That Make Ulcerative Colitis Worse
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Can Acid Reflux Cause Nerve Pain
Acid reflux symptoms can be typical or atypical in nature. Tingling limbs and nerve pain are considered rare and atypical acid reflux symptoms.
Dr. Mark Babyatsky, a former department chairman at Mount Sinai School of Medicine in New York, explained that inflammation from acid reflux can reach the lungs and trigger pneumonia.
As a result, the diaphragm can become inflamed, affecting the phrenic nerve, which is a nerve connecting the neck, lung, heart, and diaphragm. In this scenario, a patient can feel referred pain in the limbs, specifically the arms and shoulders.
Alternatively, nerve-related issues may be caused by pre-existing neuropathic conditions, leading to acid reflux. An example of this is gastroparesis. Gastroparesis is a form of diabetic peripheral neuropathy characterized by slow digestion. This leads to bloating, heartburn, and vomiting of undigested food.
If youre experiencing acid reflux symptoms with nerve pain, theres a high chance that your nerve pain is not reflux-related, especially if you are experiencing temporary reflux. Get in touch with a medical professional to find a separate diagnosis concerning your nerve pain.
Recommended Reading: How To Slim Your Stomach In 3 Days
Also Check: Horse Stomach Ulcers Natural Remedies
What To Eat For Acid Reflux
Whether its a chronic condition or a newfound symptom of stressful days, heartburn happens! Avoiding spicy, acidic and fried foods as well as cutting back on alcohol and chocolate can help douse the flames and there are some foods you should gravitate towards to help reduce the discomfort. Heres what you can eat to help keep heartburn symptoms from being too upsetting.
Stomach And Back Pain At The Same Time
For most of us, its not uncommon to have an occasional stomachache or acute back pain. But what does it mean if both are happening at the same time? This could be a coincidence, but it may also be concerning to notice two disconnected symptoms. The combination of pains may make daily activities difficult or be distracting. If the pain reaches this level, it may be a good idea to visit an Atlanta MRI center to rule out any serious conditions that could cause both problems at the same time.
If your stomach ulcers caused by a Helicobacter pylori bacterial infection, youll be given:
- a course of antibiotics
- a medication called a proton pump inhibitor
This is also recommended if its thought your stomach ulcers caused by a combination of an H. pylori infection and non-steroidal anti-inflammatory drugs .
Donât Miss: Milk Of Magnesia For Mouth Ulcers
Read Also: What Can I Do For Mouth Ulcers
The Problem With Pills
So why not just take the medications that neutralize stomach acid or restrict its production? The problem is, except for the most serious cases of GERD, these drugs are not meant for long-term or continual use. Over time, they can have negative side effects. Antacids can eventually upset the digestive tract and lead to diarrhea or constipation. Proton pump inhibitors like Prevacid and Prilosec, which are used to reduce the production of stomach acid, have been linked to increased risk of osteoporosis , pneumonia, and negative drug interactions.
And unfortunately, the many pills now available to treat acid reflux have done little to curtail its incidence. Approximately 40% of adult Americans now suffer from acid reflux. And shockingly, rates of esophageal cancer in the U.S. have increased 500% since the 1970s. Research, particularly a recent study from Denmark following more than 9, 800 GERD sufferers, has linked proton pump inhibitors with increase risk of esophageal cancer.
Damage To Your Esophagus
When the acid flows back up, it enters the esophagus, a tube that connects your mouth to your stomach. This can set the stage for:
- Esophagitis: Stomach acid irritates the lining of the esophagus, causing it to swell. This inflammation is called esophagitis, which can lead to painful swallowing.
- Esophageal ulcers: GERD is the top cause of ulcers, or sores in the lining of the esophagus. Symptoms include painful swallowing, nausea, and chest pain. Your doctor will prescribe medicine to control your GERD and treat the ulcer.
- Esophageal stricture: Over time, the damage caused by stomach acid can scar the lining of the esophagus. When this scar tissue builds up, it makes the esophagus narrow. Called strictures, these narrow spots make it hard to swallow food and drinks, which can lead to weight loss and dehydration.Strictures are treated with a procedure that gently stretches your esophagus.
- Barrettâs esophagus: About 5% to 10% of people with GERD develop this condition, where stomach acid causes precancerous changes in cells.The good news is that only 1% of people with Barrettâs esophagus will get esophageal cancer. Doctors can remove the abnormal cells when they diagnose you early on. Because the condition doesnât cause any obvious symptoms, you should see your doctor if you have GERD. They may do a procedure called an endoscopy, where a thin, flexible tube with a camera is inserted into your esophagus.
Read Also: How To Heal Venous Ulcers
Also Check: How To Prevent Skin Ulcers
Signs Of Possible Colitis
General signs of colitis can include:
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.
The Worst Foods For Those With Ulcerative Colitis
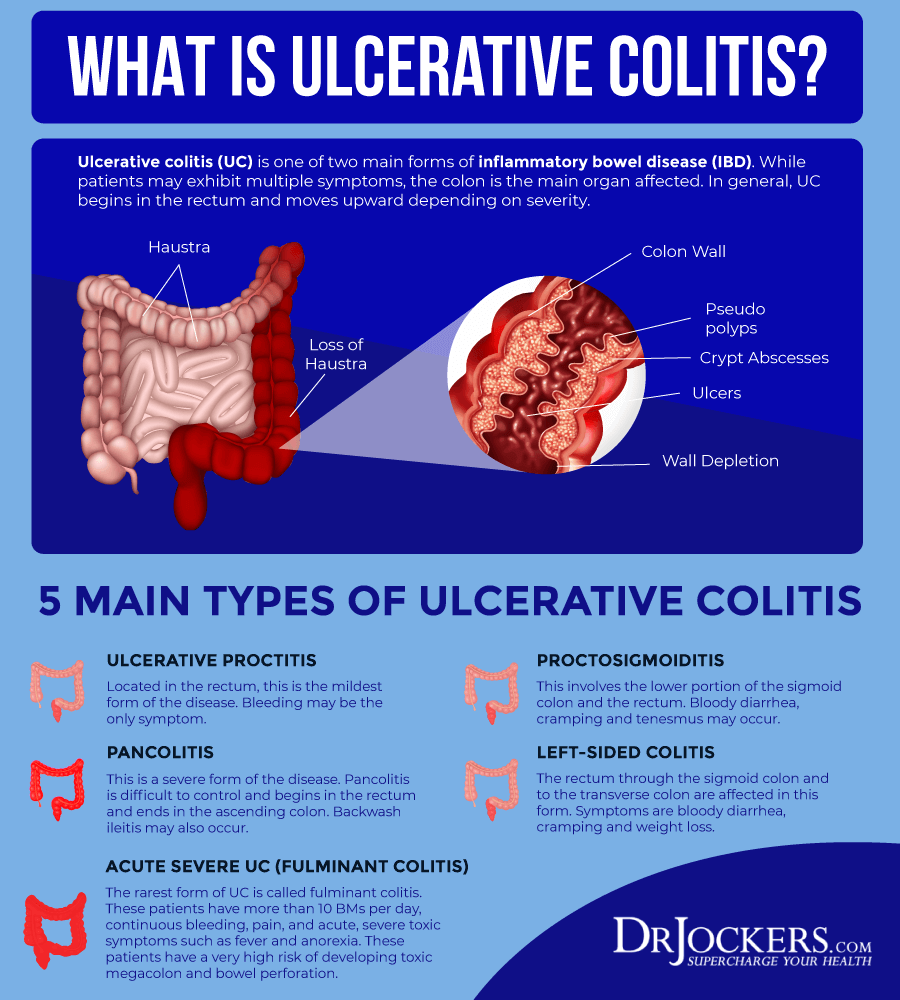
Ulcerative colitis is an inflammatory chronic disease of the colon and rectum where ulcers develop inside the lining of the large intestine. It is an inflammatory bowel disease along with Crohns Disease which causes a multitude of painful and unpleasant symptoms. Since dietary habits can contribute to ulcerative colitis symptoms, lets look at the worst foods for those with ulcerative colitis.
Don’t Miss: Dr Reckeweg Medicine For Ulcerative Colitis