What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Complications Of Crohn’s Disease
Several complications of Crohn’s disease have already been mentioned, including nutritional deficiencies, loss of weight, anemia, growth retardation, and delayed puberty. Two more serious complications also mentioned previously are strictures or narrowing of the intestine due to scarring and the formation of fistulas. Massive intestinal bleeding and perforation are unusual.
Can Peptic Ulcers Be Prevented
Doctors arent sure how H. pylori bacteria spread from person to person. The bacteria have been found in saliva , so kissing may be one way. They also may spread through food, water, or contact with vomit thats infected with the bacteria.
Regular use of NSAIDs can cause gastrointestinal problems and bleeding in some people. Acetaminophen does not cause stomach ulcers and is a good alternative to NSAIDs.
As with many infections, washing your hands well and often is an important part of ulcer prevention. This is extra important after you use the bathroom and before you eat. And take good care of your body by exercising regularly and not smoking or drinking.
Don’t Miss: Possible Causes Of Ulcerative Colitis
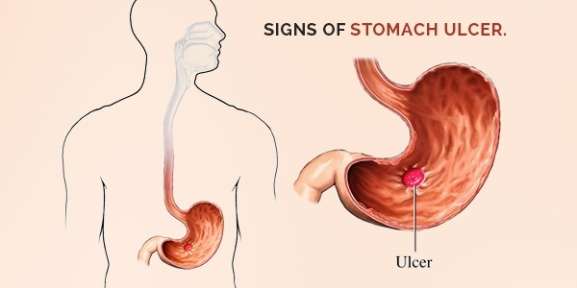
What Are The Symptoms Of Peptic Ulcers
Each persons symptoms may vary. In some cases ulcers dont cause any symptoms.
The most common ulcer symptom is a dull or burning pain in your belly between your breastbone and your belly button . This pain often occurs around meal times and may wake you up at night. It can last from a few minutes to a few hours.
Less common ulcer symptoms may include:
- Feeling full after eating a small amount of food
- Burping
- Bloody or black stool
- Vomiting blood
Peptic ulcer symptoms may look like other health problems. Always see your healthcare provider to be sure.
What Causes Stomach Ulcers
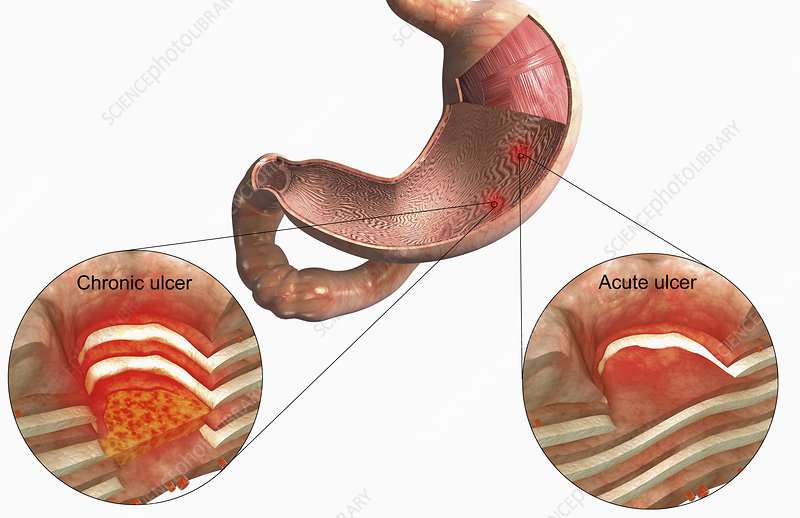
Stomach ulcers occur when the layer that protects the stomach lining from stomach acid breaks down, which allows the stomach lining to become damaged.
This is usually a result of:
- an infection with Helicobacter pylori bacteria
- taking non-steroidal anti-inflammatory drugs , such as ibuprofen or aspirin particularly if they’re taken for a long time or at high doses
It used to be thought that stress or certain foods might cause stomach ulcers, but there’s little evidence to suggest this is the case.
Read more about the causes of stomach ulcers.
Read Also: What Is Ulcer Pain Like
What Are The Causes Of Colon Cancer Vs Ulcerative Colitis
Colon Cancer Causes
Most colorectal cancers arise from adenomatous polyps. Such polyps are comprised of excess numbers of both normal and abnormal appearing cells in the glands covering the inner wall of the colon. Over time, these abnormal growths enlarge and ultimately degenerate to become adenocarcinomas.
People with certain genetic abnormalities develop what are known as familial adenomatous polyposis syndromes. Such people have a greater-than-normal risk of colorectal cancer. In these conditions, numerous adenomatous polyps develop in the colon, ultimately leading to colon cancer. There are specific genetic abnormalities found in the two main forms of familial adenomatous polyposis.
Adenomatous polyposis syndromes tend to run in families, which are referred to as familial adenomatous polyposis . Celecoxib has been FDA approved for familial adenomatous polyposis. After six months, celecoxib reduced the mean number of rectal and colon polyps by 28% compared to placebo 5%.
Other risk factors for developing colon cancer include:
- Ulcerative colitis or Crohn’s disease
- Breast, uterine, or ovarian cancer now or in the past
- A family history of colon cancer
- Colon cancer usually occurs before age 40 years.
Ulcerative Colitis Causes
Emotional stress or food sensitivities do not cause ulcerative colitis however, these factors may trigger symptoms in some people.
Risk factors for inflammatory bowel disease include:
What Is The Cause
Normally the lining of the intestine normally keeps the intestine from being hurt by stomach acid and digestive juices. If this protective layer breaks down, stomach acids can damage the walls of the intestine and cause an ulcer. You may get an ulcer when:
- You have bacteria called Helicobacter pylori . These bacteria cause most duodenal ulcers. When H. pylori bacteria infect the intestine, the infection can weaken the lining of the intestine.
- You regularly take nonsteroidal anti-inflammatory drugs , such as aspirin, ibuprofen, naproxen, or ketoprofen. These medicines irritate the lining of the stomach and upper intestine, making it easier for stomach acid to damage the lining.
- Your stomach makes too much acid.
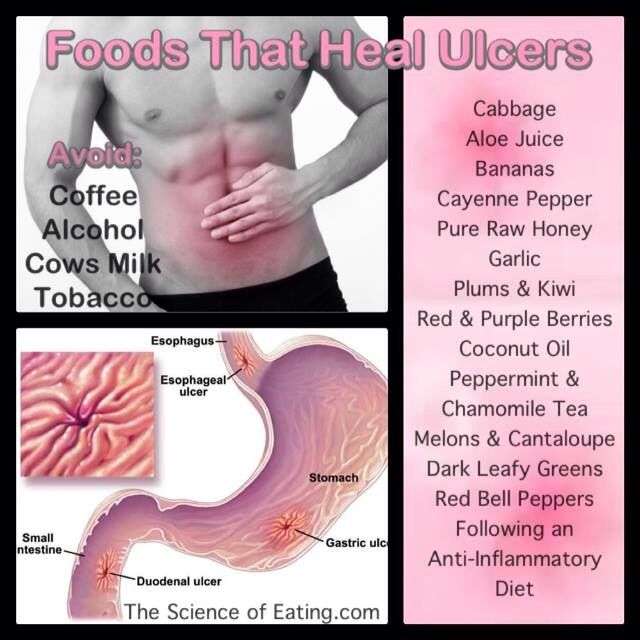
While they may not cause ulcers, some things may make ulcers worse, increase pain, or slow ulcer healing, such as:
- Smoking cigarettes or chewing tobacco
- Drinking alcohol
- Eating foods with a high acid content, such as oranges or tomatoes
- Drinking coffee and colas
- Stress
You are more likely to get a duodenal ulcer if you have a family history of ulcers. Overall, the problem is more common in men than women. Most ulcers first happen between ages 40 and 50.
Recommended Reading: Wound Care Treatment For Diabetic Foot Ulcer
You May Like: Best Cure For Mouth Ulcers
Youve Had Unexplained Vomiting
From time to time, the nausea brought on by ulcers may become so intense that it could actually cause you to vomit. Frequent vomiting is never a fun experience, but whatever you do, stay away from medications like ibuprofen and aspirin when treating the condition and other ulcer symptoms. According to Dr. Sengupta, these over-the-counter pain medications actually put you at a higher risk of developing ulcers, and can make your current ulcers worse.
Research And Statistics: How Many People Have Ulcerative Colitis
People of European descent have a higher risk of developing ulcerative colitis than do those of African or Hispanic descent.
People of European Jewish descent have an especially high risk.
Ulcerative colitis tends to run in families, affecting men and women equally overall. But older men are more likely to develop it than older women, according to the Crohns and Colitis Foundation.
Read Also: How Long Do Ulcerative Colitis Flare Ups Last
How Is Ulcerative Colitis Diagnosed
A thorough physical exam and a series of tests may be required to diagnose ulcerative colitis.
Blood tests may be done to check for anemia, which could indicate bleeding in the colon or rectum. Blood tests may also uncover a high white blood cell count, which is a sign of inflammation somewhere in the body. By testing a stool sample, the doctor can detect bleeding or infection in the colon or rectum.
The doctor may do a colonoscopy or sigmoidoscopy. For either test, the doctor inserts an endoscopea long, flexible, lighted tube connected to a computer and TV monitorinto the anus to see the inside of the colon and rectum. The doctor will be able to see any inflammation, bleeding, or ulcers on the colon wall. During the exam, the doctor may do a biopsy, which involves taking a sample of tissue from the lining of the colon to view with a microscope. A barium enema x-ray of the colon may also be required. This procedure involves filling the colon with barium, a chalky white solution. The barium shows up white on x-ray film, allowing the doctor a clear view of the colon, including any ulcers or other abnormalities that might be there.
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Also Check: Stage Iv Sacral Decubitus Ulcer
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
You Bleed When You Use The Bathroom
Blood coming from the gastrointestinal tract can signal a variety of underlying health issues, but Dr. Sengupta says when this bleeding is combined with upper abdominal pain, hes highly suspicious that its one of the signs of an ulcer. Many patients notice this blood either when vomiting, or when using the bathroom, as their stools may appear black. If you notice youre suffering from a bleeding GI tract, along with nausea and pain in the stomach or chest, Dr. Sengupta says doctors will often perform a blood test or an upper endoscopywhere they use a camera to look into the stomach itselfto check if an ulcer is the culprit. Blood in your stool can also be due to hemorrhoids or a symptom of colon cancer, so its a good idea to get checked out by your doctor.
Read Also: What To Do When You Have An Ulcer
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
When Should You Call Or See A Doctor
If you think you have a stomach ulcer, call your doctor. Together you can discuss your symptoms and treatment options. If you dont already have a physician, you can use the Healthline FindCare tool to find a provider near you.
Its important to get a stomach ulcer taken care of because without treatment, ulcers and H. pylori can cause:
- bleeding from the ulcer site that can become life-threatening
- penetration, which occurs when the ulcer goes through the wall of the digestive tract and into another organ, such as the pancreas
- perforation, which occurs when the ulcer creates a hole in the wall of the digestive tract
- obstruction in the digestive tract, which is due to swelling of inflamed tissues
- stomach cancer, specifically
Symptoms of these complications can include those listed below. If you have any of these symptoms, be sure to call you doctor right away:
- weakness
You May Like: How Do You Test For An Ulcer In The Stomach
How Do H Pylori Cause A Peptic Ulcer And Peptic Ulcer Disease
H. pylori are spiral-shaped bacteria that can cause peptic ulcer disease by damaging the mucous coating that protects the lining of the stomach and duodenum. Once H. pylori have damaged the mucous coating, powerful stomach acid can get through to the sensitive lining. Together, the stomach acid and H. pylori irritate the lining of the stomach or duodenum and cause a peptic ulcer.
What Other Conditions Are Related To Ulcerative Colitis
Ulcerative colitis is a type of inflammatory bowel disease , but it’s not the same as irritable bowel syndrome .
Although the disorders share some of the same symptoms, such as abdominal pain and diarrhea, inflammation and ulcers do not occur with IBS.
Another disease often mentioned alongside ulcerative colitis is Crohns disease. Ulcerative colitis and Crohns are different types of IBDs that affect the digestive tract in different ways.
There are some common symptoms between the two conditions, but the overall pattern of symptoms tends to be different for each.
While diarrhea and rectal bleeding are more common in ulcerative colitis, Crohns disease more often causes severe abdominal pain, nausea, weight loss, and vomiting.
Ulcerative colitis is limited to the lining of the large intestine , whereas Crohns disease can affect the entire digestive tract from your mouth to your anus and isnt limited to the inner part of the intestines.
Don’t Miss: How Severe Is Ulcerative Colitis
Ileal Pouch For Ulcerative Colitis
There is one surgical technique that can cure ulcerative colitis without the need for a colostomy or ileostomy bag.
The Ileal Pouch technique is a surgical procedure which removes the entire colon, from the point of its attachment at the small intestine to the point of its attachment at the anus. The anal sphincter muscles and the anus are left intact. The last 10 inches of the small intestine are then used to make a U-shaped sac which is attached to the anus at the anal opening.
This pouch acts as a new rectum. The anal sphincter is left in place so that the person can still control his bowel movements. A person generally moves his bowels 4 to 8 times per day following this operation. However, he has reasonably good control, and no longer has any symptoms of the colitis.
The ileal pouch procedure requires two operations. During the first operation, the surgeon removes the entire colon, creates the pouch and hooks it to the anus. He makes an ileostomy, which means that the person must temporarily wear a bag on the abdomen to collect stool. This prevents bowel contents from entering the pouch until it is healed. After about three months, the surgeon removes the ileostomy. The pouch then begins to function as a rectum, and the person no longer needs the ileostomy bag.
Symptoms Of A Duodenal Ulcer
If you have a duodenal ulcer, you might:
- have pain in the stomach or abdomen
- have indigestion
Very occasionally, an ulcer can cause serious complications. Go to the emergency department if:
- you have a sharp pain in your stomach that doesnt go away
- your vomit or stools look bloody or a black colour
If you are concerned about symptoms, you can use healthdirects online Symptom Checker to get advice on the next appropriate healthcare steps and when to seek medical attention.
You May Like: Do Ulcers Cause Weight Loss
Read Also: Is Ulcerative Colitis And Colitis The Same Thing
Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.
Complications Of Ulcerative Colitis
UC increases your risk of developing colon cancer. The longer you have the disease, the higher your risk of this cancer.
Because of this increased risk, your doctor will perform a colonoscopy and check for cancer when you receive your diagnosis.
Repeat screenings are recommended thereafter, according to the American Cancer Society. Regular screenings help lower your risk of colon cancer. Follow-up screenings can detect precancerous cells early.
Other complications of UC include:
- thickening of the intestinal wall
- intestinal bleeding
Don’t Miss: Good Foods To Eat With An Ulcer
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.