Pressure Ulcers: What To Look For And Document About A Deep Tissue Injury
The professional staff at nursing homes and hospitals must conduct a comprehensive head-to-toe skin assessment on patients most at risk for developing decubitus ulcers. The skin may be compromised, requiring daily skin care to promote health.
Any detected bedsore should be fully documented in the residents healthcare plan to ensure they receive the best care for healing.
Documentation identifying a detectable pressure sore should include:
- The sores location
- The stage of the ulcer
- Pressure ulcers size, including its width, depth, and length, measured in centimeters
- Any identifiable sinus tract, tunneling, or undermining
- The presence of exudate , including its location, amount, and color
- The appearance and size of the wound bed, including a description of visible tissue
- A description of the sores edges, including any evidence of redness, rolled edges, maceration , or induration
- A description of the area surrounding the sore
- The absence or presence of pain
- The absence or presence of any foul odor
The nursing home team must ensure that patients most at risk for developing bedsores are moved at least once every 2 hours. If the patient is sitting in a wheelchair, chair, or recliner, they should readjust their body weight at least once every 15 minutes.
People highly susceptible to developing pressure sores need assistance from nurses, nursing aides, and licensed practical nurses to minimize the potential of falling and causing injury.
What Type Of Ulcer Is A Diabetic Ulcer
What Is a Diabetic Foot Ulcer? A diabetic foot ulcer is an open sore or wound that occurs in approximately 15 percent of patients with diabetes, and is commonly located on the bottom of the foot. Of those who develop a foot ulcer, six percent will be hospitalized due to infection or other ulcer-related complication.
Good Mouth Care And Mouth Rinses
Good mouth care is key to help reduce the risk or severity of mouth sores. Using a soft toothbrush or foam swab can help keep the mouth clean and reduce the risk of injuring your gums and lining of the mouth. If you use dental floss, ask your doctor if you should stop or if you can continue to floss.
Certain types of rinses can help to keep your mouth clean and can help soothe discomfort. Ask your doctor which type of rinse may be best for your situation. For example, baking soda, salt water, or saline rinses might be recommended. Mouth rinses with antibiotic agents or steroids might be recommended, depending on how severe the mouth sores are.
Benzydamine may help prevent mouth sores in people getting radiation treatment to the mouth or throat. Morphine rinses may help relieve pain from mouth sores in this same group of people. Dexamethasone has been used in mouth rinses to help with cleansing and discomfort.
Another type of mouth rinse, often referred to as magic mouthwash might be recommended by your doctor. Magic mouthwash is a mixed medication mouthwash that combines a few different medicines. But, there is not one single combination thats used by all doctors, and some experts dont recommend a combination. Some common ingredients of magic mouthwash include diphenhydramine, viscous lidocaine, aluminum hydroxide, nystatin, and corticosteroids.
You May Like: Worst Foods To Eat With An Ulcer
What To Expect After Treatment With Cvm
At the Center for Vascular Medicine, our mission is to help patients with their vascular diseases in a cost-effective and compassionate manner. We specialize in the diagnosis and treatment of venous and arterial diseases in the legs, feet, and pelvis. Our world-class providers are the most experienced in the specialty and work with patients to develop a treatment plan that is custom-tailored to their unique situation.
Typically, this process involves an initial consultation and ultrasound scan at one of our accredited facilities. After reviewing the results of your scan and obtaining a thorough medical history, our providers will discuss the results with you and help you decide on the next steps.
Our health care providers use several diagnostic tests to help determine what vascular diseases may be causing your symptoms. Our initial evaluations utilize ultrasound because this non-invasive imaging modality helps us verify our suspicions on whether your symptoms are caused by underlying vascular disease.
Foot Ulcer that will not heal Foot ulcer that healed for the first time after the procedure
The venous stent procedure was conducted by Dr. Satwah, physician for the Center for Vascular Medicine.
Read Also: Ways To Prevent Pressure Ulcers In Hospitals
Other Causes Of Peptic Ulcers

- Genetics: A significant number of individuals with peptic ulcers have close relatives with the same problem, suggesting that genetic factors may be involved.
- Smoking: People who regularly smoke tobacco are more likely to develop peptic ulcers when compared with non-smokers.
- Alcohol consumption: Regular heavy drinkers of alcohol have a higher risk of developing peptic ulcers.
- Corticosteroid use: People on large or chronic doses of corticosteroids are also at greater risk.
- Mental stress: This stress has not been linked to the development of new peptic ulcers, but symptoms appear to be more severe in people with ulcers who are experiencing ongoing mental stress.
A patientâs description of symptoms will normally cause a doctor to suspect a peptic ulcer.
Tests that can confirm a diagnosis include:
- a blood test to check for H. pylori, though a positive test does not always mean there is an active infection
- a breath test, using a radioactive carbon atom to detect H. pylori
- a stool antigen test to detect H. pylori in the feces
- an upper gastrointestinal X-ray to identify ulcers
An endoscopy may also be used. This involves a long, narrow tube with a camera attached to the end is threaded down the patientâs throat and into the stomach and duodenum. This is the best diagnostic test.
Recommended Reading: Alternative Medicine For Ulcerative Colitis
Treatment For Diabetic Ulcers
When someone identifies an ulcer, they should seek medical care to prevent its progression. The primary goal of treatment is to promote healing as soon as possible. Treatment will often depend on the grade of the ulcer.
If an infection is present, a doctor will likely prescribe antibiotics. They may require a tissue sample to identify the cause of the infection. The antibiotic type and dosage a doctor suggests will depend on the infection organism and the severity of the infection.
In some cases, surgical options may be necessary to help encourage healing, relieve pressure on the area, and prevent further complications. These options may include:
- education on foot care and control of blood sugar levels
- medications for blood sugar control
- offloading pressure from the ulcer by using crutches, a wheelchair, or a non-removable cast to promote healing
- medicines to help improve blood circulation
- topical medications and dressings
Stage 4 Bedsore Treatment
Stage 4 bedsores should be treated as soon as possible, as they put a nursing home patient at high risk of deadly health problems.
Stage 4 pressure ulcer treatment may include:
-
Removing any damaged, infected, or dead tissue from the bedsore
- Skin Grafts
Covering the affected area with healthy skin
It can take anywhere from 3 months to 2 years for an advanced stage 4 bedsore to heal, according to the Model Systems Knowledge Translation Center .
You May Like: Hiv Ulcers In Mouth Pictures
How Is Venous Insufficiency Diagnosed
Your doctor will want to do a physical examination and take a complete medical history to figure out if you have venous insufficiency. They may also order some imaging tests to pinpoint the source of the problem. These tests may include a venogram or a duplex ultrasound.
Venogram. Your doctor will put an intravenous contrast dye into your veins. Contrast dye causes the blood vessels to appear opaque on the X-ray image, which helps the doctor see them on the image. This dye will provide your doctor with a clearer x-ray picture of your blood vessels.
Duplex ultrasound. A type of test called a duplex ultrasound may be used to test the speed and direction of blood flow in the veins. A technician will place gel on the skin and then press a small hand-held device against your skin. The transducer uses sound waves that bounce back to a computer and produce the images of blood flow.
Mixed Red And White Patches
A mixture of red and white patches in your mouth, called erythroleukoplakia, is an abnormal cell growth thats more likely to become cancerous. If red and white patches last more than two weeks, you should see your dentist. You may see these mouth abnormalities before you feel them. In the early stages, mouth cancer may cause no pain.
Bright red patches in your mouth that look and feel velvety are called erythroplakia. They are often precancerous.
You May Like: What Desserts Can I Eat With Ulcerative Colitis
Recommended Reading: Is Imodium Safe For Ulcerative Colitis
Treatment For Buruli Ulcer
Most Buruli ulcers can be treated with a course of specific oral antibiotics. Surgery is sometimes used in combination with antibiotic therapy. If surgery is required, a small amount of surrounding healthy tissue is also cut out to make sure the infection is completely removed. Depending on the extent of surgery, skin grafts may be needed to close the wound. Sometimes the ulcer can return after surgery, requiring another course of antibiotics or an operation . As the ulcer gets bigger with time, early diagnosis and prompt treatment can minimise skin loss.
Symptoms Of Skin Ulcers Which Are Infected Include:
- Pus draining from the skin
- Skin tenderness
- Red streaks in the skin Lymphangitis of the arm and Lymphangitis of the back of the legs
At the start of the formation of an ulcer of the skin, the cells in the area of the body begin to break down and slough away, leaving the area red. Without treatment of the underlying reason for the skin degradation, the erosion of cells may eventually form a blister or bubble of fluid, just beneath the skin. This then breaks open and creates a crater. This crater is the actual skin ulcer and is generally characterized by a perimeter of skin which is surrounding a shiny, depressed center, which can be red, green or yellow depending on how much skin has deteriorated and whether or not an infection has developed.
You May Like: Nutritionist Specializing In Ulcerative Colitis
You May Like: What Do You Do For A Bleeding Ulcer
How Is A Stage 1 Pressure Ulcer Treated
For a stage I sore, you can wash the area gently with mild soap and water. If needed, use a moisture barrier to protect the area from bodily fluids. Ask your provider what type of moisturizer to use. Stage II pressure sores should be cleaned with a salt water rinse to remove loose, dead tissue.
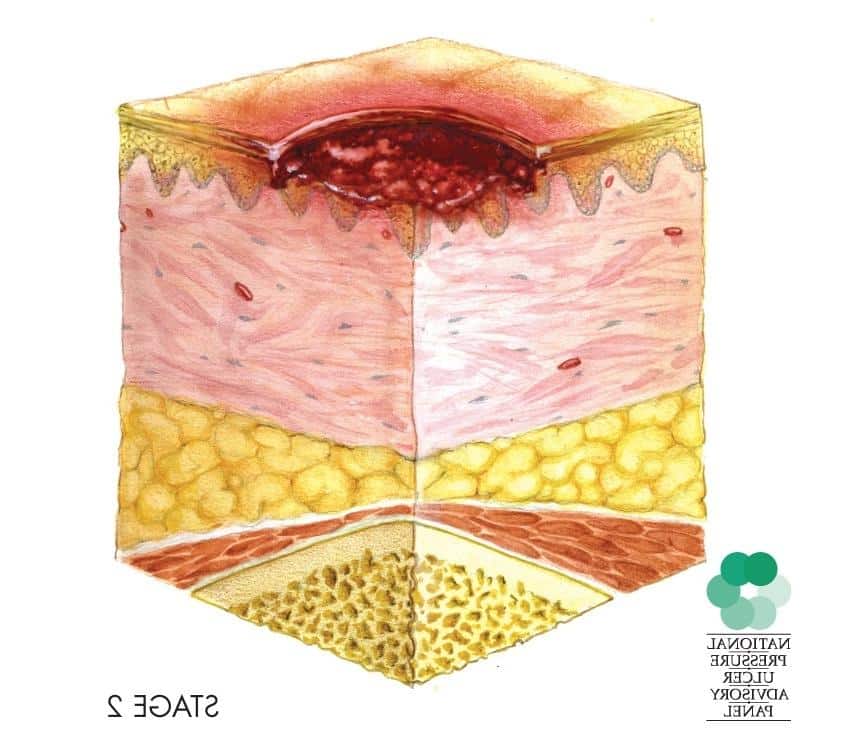
What is a grade 2 pressure ulcer?
Grade 2: partial thickness skin loss involving epidermis, dermis, or both. The ulcer is superficial and presents clinically as an abrasion or blister. Grade 3: full thickness skin loss involving damage to or necrosis of subcutaneous tissue that may extend down to, but not through underlying fascia.
What do Stage 1 bed sores look like?
A stage 1 bedsore has not broken the surface of the skin yet, and it can be identified as a spot that feels and looks different from surrounding skin. A stage 1 bedsore can differ from other skin by being: Red or discolored. Harder or softer.
Stage 3 Pressure Injury: Full
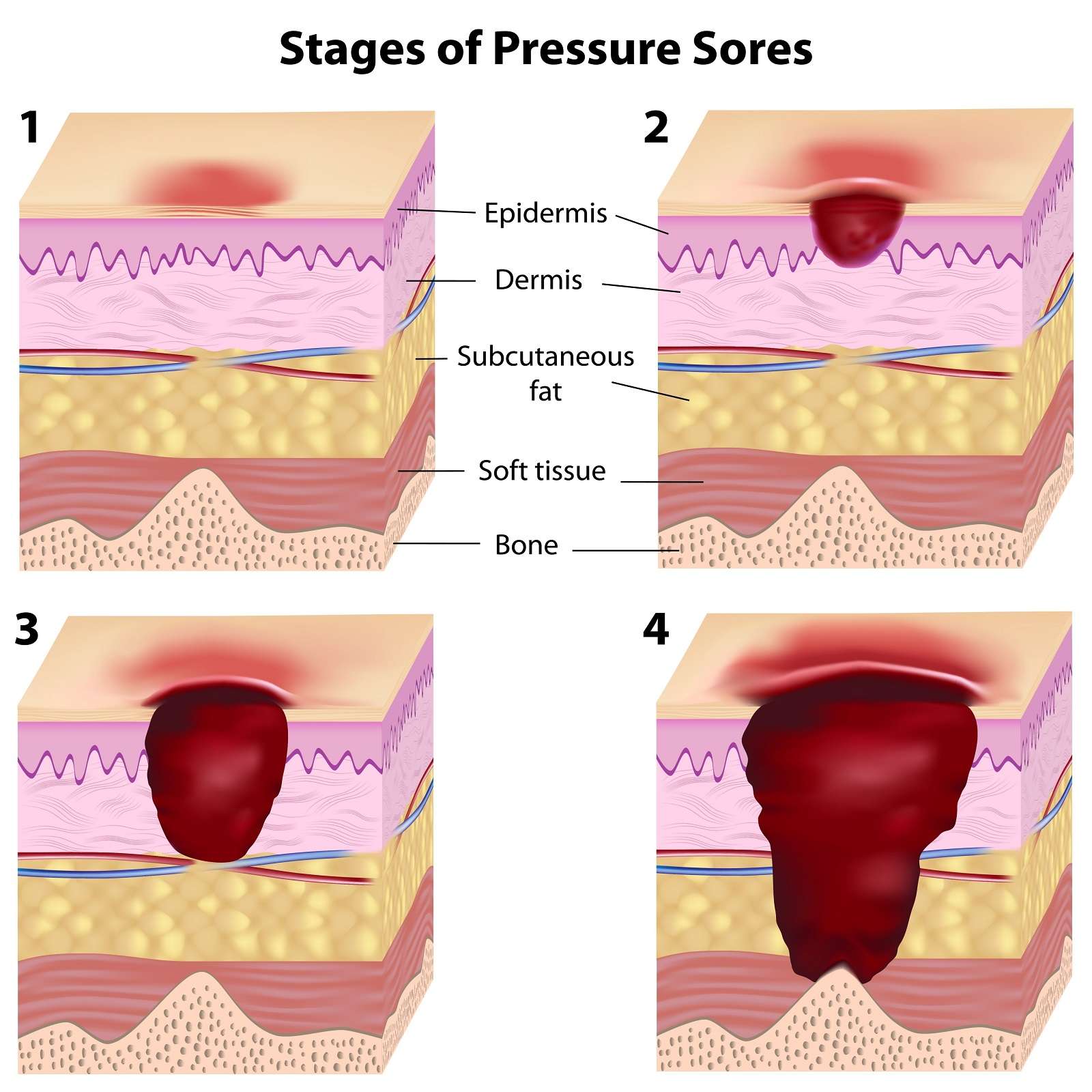
Stage 3 pressure injuries involve full-thickness loss of skin, where fat tissue is visible and granulation tissue, rolled wound edges , and eschar may also be present. However, fascia, muscle, tendon, ligament, cartilage, and bone are not exposed. The depth of tissue damage may vary by anatomical location areas with significant amounts of fat are at risk of developing deeper wounds. For visual reference, see illustrations of pressure injuries from the NPUAP here.
You May Like: Can You Develop Ulcerative Colitis
What Are The Signs Of Diabetic Feet
The main signs of a diabetes-related foot condition are the physical irregularities described above.
These signs will vary from person to person but may also include:
- Feeling excessively warm or cold to the touch
- A lack of sensation in the foot
- Pain or tingling in one or both feet
- Swelling of the foot
- Fever, chills or shaking if a diabetic foot becomes infected
- Uncontrollable changes in blood sugar level
Who Is At Risk For A Decubitus Ulcer
Individuals with limited mobility and who remain for long periods of time sitting or lying in the same position are vulnerable to developing pressure ulcers. Older individuals with more fragile skin are also at risk. Other risk factors include:
- Poor diet with insufficient nutrients for skin health.
- Not drinking enough water to hydrate skin.
- Medical conditions such as diabetes which causes poor blood circulation to skin tissue.
You May Like: Foods That Flare Up Ulcerative Colitis
Other Causes And Factors
Other causes are rare. For example, some viral infections can cause a stomach ulcer. Crohns disease may cause a stomach ulcer in addition to other problems of the gut.
Stomach cancer may at first look similar to an ulcer. Stomach cancer is uncommon but may need to be ruled out if you are found to have a stomach ulcer.
Read Also: What Is A Duodenal Ulcer And How Is It Caused
Signs And Symptoms Of Venous Ulcers
Symptoms may show up even before an ulcer forms, such as:
- Swelling, heaviness or cramping in the legs
- Hardening or thickening of the skin
- Dark red, purple or brown discoloration
Signs and symptoms of venous ulcers include:
- Sore on the inside of the leg or just above the ankle. The base of the wound is red and is sometimes covered by yellow tissue. The edges of the ulcer may be unevenly shaped.
- Skin around the wound is shiny, warm or hot, tight and discolored.
- Pain in the leg.
Also Check: Is Kimchi Good For Ulcerative Colitis
Don’t Miss: Diet For Stomach Ulcers Mayo Clinic
Locations Of Buruli Ulcer Outbreaks
Buruli ulcer has been reported in 33 countries around the world. Affected areas include rural West Africa, Central Africa, New Guinea, Latin America and tropical regions of Asia.
In Australia, Buruli ulcer most commonly occurs in localised coastal areas of Victoria.
There are three recognised levels of risk in the areas where Buruli ulcer is endemic in Victoria:
- The highest risk is associated with the active transmission areas of Rye, Sorrento, Blairgowrie and Tootgarook on the Mornington Peninsula.
- There is a moderate risk associated with areas in the Bellarine Peninsula , and the Frankston and Seaford areas.
- There is a low risk associated with the rest of the Bellarine and Mornington Peninsula, the South Eastern Bayside suburbs and East Gippsland.
Recent cases from Aireys Inlet on the Surf Coast and the Geelong suburb of Belmont, as well as Essendon, Moonee Ponds and Brunswick West in inner Melbourne, suggest that these are emerging areas of local transmission. Two cases were identified in residents in Aireys Inlet and two in Belmont during 2019, with no known travel to an endemic area. The risk of transmission in these areas is considered low.
Stage One Pressure Injury
The skin may be swollen, red, and feel warm due to a prolonged reduction of blood circulation. A stage 1 pressure sore may be painful, but it doesnt not penetrate below the skin surface.
For those with tan, brown, or black skin, the area may not look red. Instead the patient will exhibit patches of darker skin. Stage 1 bedsores may either feel firmer or softer than the skin that surrounds the pressure injury.
What Does a Stage 1 Pressure Injury Look Like?
The area around stage 1 pressure injuries is red and feels warm. It may have a blue or purple tint on dark-skinned patients. A person with stage 1 pressure sores may experience itching, burning, or pain.
Also Check: Ulcerative Colitis Pain In Legs
Signs You May Have An Ulcer
Did you know that stomach ulcers also called peptic ulcers affect at least 1 in 10 Americans over the course of their lives? And while stomach ulcers can be treated easily when caught early, lack of medical care can lead to serious complications.
Understanding the signs of stomach ulcers is important in helping you get the treatment you need. At Prima Medicine in Fairfax and South Riding, Virginia, our care team has the experience and knowledge to diagnose and treat stomach ulcers. Weve curated this guide to help you recognize the warning signs of an ulcer and understand what you can do about it.
Venous Ulcer Diagnosis And Treatment
Doctors at Vascular surgeons at UPMCs Heart and Vascular Institute use duplex ultrasound, a noninvasive test, to diagnose abnormal veins that cause venous ulcers. Part of the UPMC difference is that we actively look for the causes of the ulceration to treat venous pathology and keep the ulcer healed.
After an evaluation of your veins, we recommend a treatment plan based on your needs:
- Compression of the leg is vital to healing venous wounds.
- Compression stockings are most commonly used for this treatment.
- The pressure from the compression dressing counteracts the pressure from the veins of the leg and allows skin to heal.
Also Check: What Causes Diabetic Foot Ulcers
Also Check: How To Fix Ulcerative Colitis Flare