The Challenge With Ibd Isnt Just Physical
Inflammatory bowel disease takes a toll. Physically, Hausman and Gaul both have struggled to just be well enough to work and live. Mentally, too, it can be a struggle to get up every day with a disease you know youll have for the rest of your life.
Hausman and Gaul have found support through their doctors and nursing staff, who take the time to listen and treat them like more than just the next patient on their schedule for the day.
Help also has come from their families, who so many times have been able to do nothing but watch their loved one get sick and exhausted and, at times, unable to participate in life.
Gaul has leaned on his wife and kids, as well as his mom, who is a retired nurse.
Hausman said of her husband, Nick, who takes her to the emergency room and sits with her in the hospital: He basically is my caretaker when I was really sick, and he didnt sign up for this.
“Its hard to watch somebody suffer and also try to be the person to help fix it, and its not immediate sometimes.”Dr. Brett Baloun
Before his ulcerative colitis got under control, Gaul had to be hospitalized twice, for five days each. His students were concerned, so he ended up spelling out for them and his colleagues what was going on why he hadnt been in class, and why he might have to suddenly leave the classroom.
While patients can face steep mental challenges, doctors arent immune to them, either.
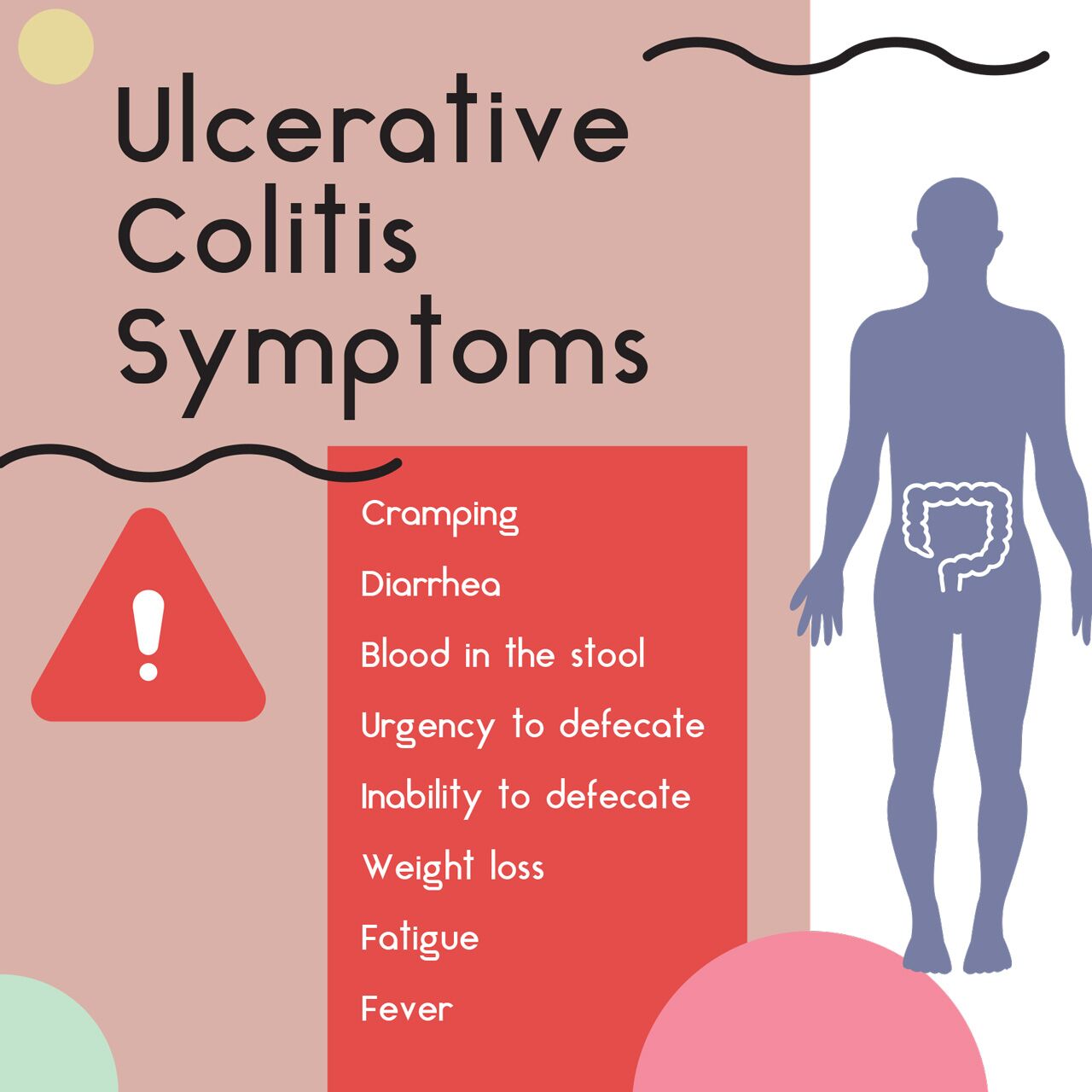
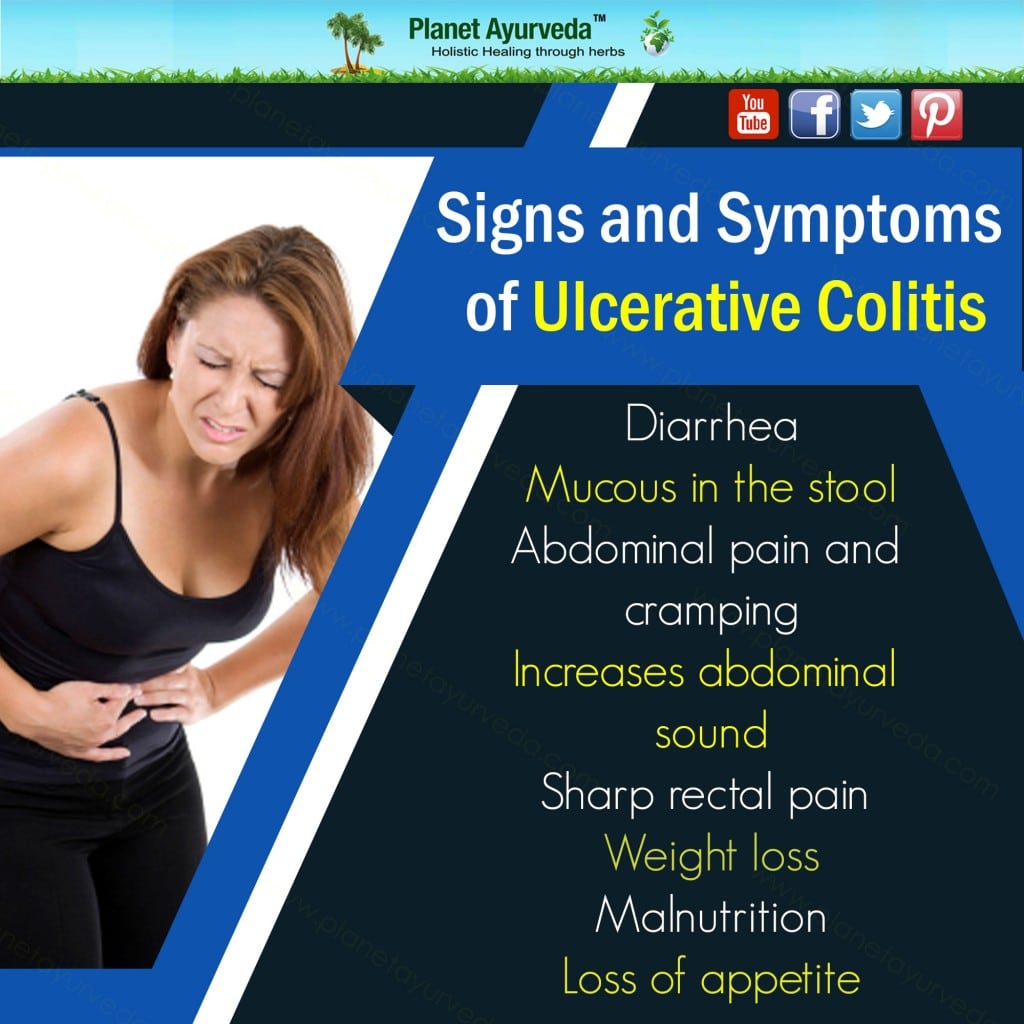
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Keep An Emergency Kit On Hand
Megan says never knowing when a flare-up will start is one of the hardest aspects of managing ulcerative colitis. I might be feeling okay when I go out, but a bowel movement could hit at any time, she says. If I cant get to the bathroom quickly, Im going to have an accident and the whole night is going to turn around.
Thats why Megan keeps a clean-up kit handy, which was crucial in her early 20s when her symptoms were at their worst. Before I was in deep remission, Id always have a clean-up kit with me that had wipes, hand sanitizer, and underwear. Id keep a whole extra pair of pants in my car, she says. Just knowing that she has whatever she needs for a worst-case scenario makes her feel more confident about making plans.
Related:
Recommended Reading: What To Take For Stomach Ulcer Pain
Research The Bathroom Situation
Wondering if you can use a bathroom when you need to is a significant barrier when it comes to making plans. Theres a lot to consider: Does the venue have public bathrooms? Are multiple stalls available so you dont have to wait for one to open up? To ease her mind, Katie tries to find out that information ahead of time.
If Im going out to someplace new where I feel uncertain about the restroom situation, Ill read through the venues reviews on Facebook and Google to see what people say about the restrooms, she says. I also use the We Cant Wait app from the Crohns & Colitis Foundation to find restrooms when I am out. You can search for public restrooms on the app as well as establishments that allow people to use employee-only bathrooms, according to the foundations website. Flush is another app that lists public restrooms, but its only available on iPhones.
Whitney A., 36, who was diagnosed with ulcerative colitis when she was 16 years old, says its hard to go anywhere that requires long car rides. Planning ahead is crucial. I work to determine where bathrooms are located all along my intended route ahead of time, Whitney tells SELF.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Don’t Miss: What Medicine To Take For Ulcer Pain
Common Medications Used To Treat Uc
The first course of action in treating UC is often amino salicylates. Also referred to as 5-ASAs, the NHS reports that these medications lower colon inflammation and allow your GI tract to heal. If 5-ASAs don’t improve your symptoms, the NHS recommends adding a short-term dose of corticosteroids. Medical professionals at The Crohn’s & Colitis Foundation explain that these drugs work by restraining your immune system. However, long-term use of corticosteroids can cause your body to reduce or stop making its cortisol, making it difficult for you to stop taking them without relapsing.
According to Healthline, many doctors turn to immunomodulators when 5-ASAs and corticosteroids fail to improve your situation. Also called immunosuppressants, these drugs target your body’s immune response and reduce inflammation. However, though studies show they’re effective, these drugs are prescribed off-label when given for the treatment of UC. Additionally, it can take several months for you to feel relief.
Medical professionals at The Crohn’s & Colitis Foundation state that the next step for those with symptoms that don’t respond to immunomodulators is to try biologics. Made out of organic material, these medications work by stopping the proteins responsible for inflammation. For those that other medications have failed or who need fast symptom relief, doctors prescribe Janus kinase inhibitors, which work by blocking inflammation signals given off by your immune system .
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Don’t Miss: I Have Ulcerative Colitis And Diverticulitis
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
I Put It Off For Too Long
Retta Hausman is that woman who had to stop for a restroom break on the way to her bachelorette party. But thats almost a lighthearted view of Crohns disease compared to what it put her through just two weeks before her wedding in the summer of 2016.
Hausman had struggled for more than two years by then with unrelenting, uncontrolled inflammatory bowel disease.
Shed first started having bloody diarrhea in January 2014, but she hesitated and didnt see a doctor until that August.
I was unsure of what it was. I was nervous, Hausman remembered.
One of the reasons why I didnt go in soon enough was that I was really embarrassed to talk about it. I put it off for too long.
In August, she saw a specialist at the Sanford Center for Digestive Health. There, a colonoscopy led to her initial diagnosis of ulcerative colitis, which is typically an inflammation of the colon in the gastrointestinal tract.
Finding out that she had a lifelong disease, in her 20s and looking forward to forming a family, was a shock.
Its a lot to take in at first. I didnt really know what it was or how it was going to affect me, Hausman said.
But she learned. It affects you every day of your life for the rest of your life, because there is no cure, she said.
Also Check: How To Lose Weight With Ulcerative Colitis
Skipping Or Forgetting To Take Your Uc Medication
UC causes inflammation and ulcers in the colon. If left untreated, this condition can lead to life threatening complications, such as:
- bowel perforation
- colorectal cancer
- toxic megacolon
A doctor will likely prescribe medication, such as an anti-inflammatory or immunosuppressant drug, to help reduce inflammation.
These medications can help ease symptoms of UC and also function as maintenance therapy to keep you in remission. Symptoms could return if you do not take your medication as directed.
At some point, the doctor may discuss slowly tapering off the medication. However, you should never decrease your dosage or stop taking your medication without speaking with your prescribing doctor first.
Will Ulcerative Colitis Affect Me Over Time
The effects of ulcerative colitis vary considerably from person to person, based on the nature and severity of their disease. In many cases, the condition does not have much impact on daily life, the ability to work or to enjoy an active social life but does take some getting used to. When it is at an active stage, symptoms such as diarrhoea and abdominal pain often require time away from work, college etc. and can make it difficult to cope going out or even being at home. However, treatment usually makes the symptoms better within days or weeks so normal quality of life can be restored quite quickly. Some severe cases of ulcerative colitis, however, can have a significant impact on peoples lives. This can be due to a weak response to treatment which makes symptom-free remission difficult to achieve and can involve frequent flare ups.
Also Check: Booties To Prevent Pressure Ulcers
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs like aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This does not mean you should stop taking antibiotics or pain medications, but you should speak with a doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to address possible side effects or a probiotic to help regrow your gut bacteria.
If you have pain that requires an over-the-counter pain reliever, the doctor may suggest using acetaminophen to reduce pain instead of an NSAID.
Adapting To The Ileostomy
Back home and under the care of Dr. Baloun, who still collaborates with Mayo about her care plan, Hausman started a new medication regimen and adapted her diet to her ileostomy.
With her colon on an extended vacation, her small intestine is not just responsible for doing its own job of digesting food. It also has taken over the colons job of absorbing water. Tasked with so much now, the small intestine may have trouble doing either job really well something Hausman has noticed.
Certain foods like nuts and seeds and some raw vegetables, they just dont break down. So I do have to avoid those foods so I dont get a blockage, Hausman said.
You basically have to chew the food until its like mush before you swallow, she added.
Its also easy to get dehydrated without a functioning colon. Hausman drinks a lot of water to help compensate, but she still has ended up in the hospital for dehydration. Some medications used to treat IBD can weaken the immune system as well, contributing to hospitalization.
Hausman spent time in the hospital twice last fall. One stay lasted five days, when she had C. diff, E. coli and norovirus infections all at the same time. The other stay was two days during a Thanksgiving trip to Denver, when she caught a virus and became dehydrated. So, like many people with weakened immune systems, she tries to avoid people who are sick, and she washes her hands frequently.
Recommended Reading: Do Stomach Ulcers Cause Diarrhea
What Counts As Frequent Urination
How much urination is normal? The answer varies from person to person. It may also vary from day to day, depending on how much you drink each day. However, the Mayo Clinic defines frequent urination as needing to pee more often than what feels normal for you.
Sometimes, frequent urination occurs with other related symptoms. Some people also experience urinary urgency , painful urination, trouble starting urinating, or urinary incontinence .
Members have reported several different changes to their regular urination habits. I always have to pee! Even thinking about peeing means I have to go pee, wrote one member. Another member with UC said, I normally pee four to five times at night and 10 or more times during the day. Its frustrating.
I have frequent urination, virtually every hour on the hour, commented a different member. At night its a real pain. It is also very hard to get it out and feels like I havent finished.
In people with IBD, urinary patterns may change based on their disease activity. I urinate way more often during flare-ups, wrote one member.
There are several possible reasons why urination may be affected by UC. For instance, UC can cause many conditions that increase the risk of urinary problems.
Side Effect: Risk Of Osteoporosis
According to the IBD Help Center, up to 60% of those with UC have decreased bone density, with those that take long-term corticosteroids showing similar statistics. However, few symptoms appear until breakage occurs. At that point, hip fractures result in nearly half of patients dying or being confined to a nursing facility within a year . Another common injury is vertebral fractures, which often result in disability. Furthermore, the more bones you break, the more likely you are to break a bone and become disabled.
Long-term corticosteroid use interferes with your bones’ ability to absorb calcium, reduces the amount of bone-forming cells your body produces, and increases the creation of cells that break down your bones . Additionally, these medications also lower the amount of estrogen your body generates. These effects all occur while the inflammation that results from the disease causes your body to form chemicals, known as cytokines, that interfere with bone metabolism.
However, Dr. Miguel Regueiro, Chair of the Digestive Disease & Surgery Institute at Cleveland Clinic, shares that in a study conducted by him and his colleagues, those who took biologics for UC were “significantly less likely” to develop osteoporosis. The researchers attribute this to the medications lowering your body’s production of cytokines.
Don’t Miss: What To Do For Leg Ulcers
Demographics Symptoms And Treatment
Demographic and clinical characteristics, including symptom frequency and treatments, are reported in Table 1 . The mean age was 39.8 years, and 55.5% of participants were female. The mean disease duration was 7.6 years, and almost half of participants had total colitis. Of the 501 subjects evaluated, 28 had undergone surgery for ulcerative colitis. The most common drug treatment used was oral in 448 participants, followed by topical in 210 .
Table 1.
Subject demographic and clinical characteristics
Stool frequency score was 0 in the majority of participants , but 10.8% had a score of 3 . Similarly, most patients had a rectal bleeding score of 0 . Of patients who had rectal bleeding , 140/231 had a subscore of 1 , 75/231 had a score of 2 , and 16/231 had a score of 3 .
Bowel urgency was assessed in Q13 and bowel incontinence in Q14 . Figure 1a and b show the responses to Q13 and Q14, respectively, with 281/501 participants experiencing some level of bowel urgency and 144/501 experiencing some level of bowel incontinence.
Fig. 1.
Incidence of bowel urgency or bowel incontinence . a Bowel urgency. Q13: How frequently did you feel anxious about not making it to a toilet in time in the past 2 weeks? b Bowel incontinence. Q14: How frequently did you experience underwear soiling in the past 2 weeks? .
In response to Q15 , most participants answered not at all or rarely .
Should You See A Doctor
In general, its a good idea to talk to your doctor any time you notice any health changes. You may want to mention frequent urination at your next appointment, especially if you have other symptoms or if trips to the bathroom are starting to disrupt your everyday life.
In some cases, frequent urination may be a sign of a more serious health problem. Get in touch with your doctor right away if you experience:
- Urine that looks red or dark brown
- Difficulties starting a stream of urine
- Pain during urination
- A feeling like your bladder isnt completely empty after you urinate
- Abdominal pain or back pain
- Loss of bladder control
You May Like: What Can I Do For Mouth Ulcers
Even On Good Days Take Your Meds
It can be easy to forget to take your medicines when you feel good. Or you might think it’s OK to skip them because you feel fine. But you need to stick with the plan your doctor prescribed to keep up those benefits.
You and your doctor will work together to decide if you need to stay on medicines to control your UC. The type of medicine will depend on how severe your UC is.