What Are The Stages Of A Pressure Sore
Pressure sores, also known commonly as bedsores or decubitus ulcers, are injuries to the body caused by sustained pressure. Their severity can be categorized according to four main phasesfrom a stage one ulcer where the skin is just beginning to show damage, to a stage four ulcer with open wounds, sores and signs of infection. Whatever the stage, all should be taken seriously and treated with urgency. Here are the four stages of a pressure sore.
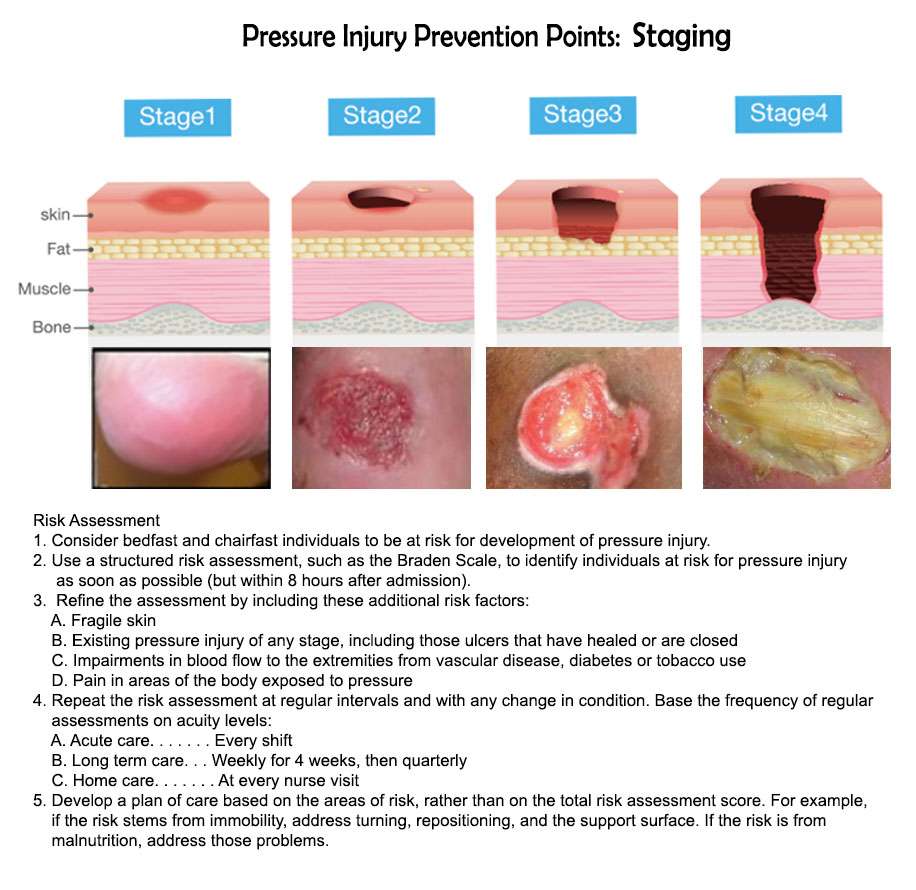
Stage 1 Pressure Sores and Ulcers: Early on in pressure ulcer development, the skin is developing injury. While no open sores or broken skin are present yet, skin may appear redder, warmer or firmer than usual. Known as a non-blanchable erythema of intact skin, the color change may indicate the beginnings of a serious injury to the deep tissue.
Stage 2 Pressure Sores and Ulcers: This is where the true sore, or ulcer, develops as a break in the skin and an open sore. It is often very painful, and can create serious damage within the skin. Known as partial-thickness skin loss with exposed dermis, these bed wounds can quickly become something worse and may even present as a blood filled blister.
Stage 3 Pressure Sores and Ulcers: In stage three, the pressure ulcer has developed into the soft tissue underneath the skin. Known as full-thickness skin loss, this stage may show a deep wound, especially in an area with more adipose tissue.
Stage 2 Bedsore Treatment
The Model Systems Knowledge Translation Center encourages people with stage 2 bedsores to see a health care provider as soon as possible.
Treatment for stage 2 bedsore typically involves:
- Bandaging: Bandages help keep bedsores dry and reduce the risk of infection.
- Cleaning: Doctors may use a saltwater solution called saline to clean the open wound when bandages are changed.
- Debriding: The Mayo Clinic notes that damaged and dead tissue must be removed so the bedsore can heal properly. This process is known as debridement.
- Getting Good Nutrition: The MSKTC recommends a diet rich in vitamin A and C, protein, zinc, and iron as part of a stage 2 bedsore treatment plan. Drinking enough water is also important. Johns Hopkins Medicine found that bedsores wont properly heal without these dietary changes.
- Reducing Pressure: Taking pressure off the bedsore will prevent it from getting worse and allow the skin to start repairing itself.
Seek medical advice from trusted doctors or nurses to learn more about treating pressure sores.
Symptoms Of Pressure Ulcers
The parts of the body most at risk of developing pressure ulcers are those that are not covered by a large amount of body fat and are in direct contact with a supporting surface, such as a bed or a wheelchair.
For example, if you are unable to get out of bed, you are at risk of developing pressure ulcers on your:
- shoulders or shoulder blades
If you are a wheelchair user, you are at risk of developing pressure ulcers on:
- the back of your arms and legs
- the back of your hip bone
Recommended Reading: Is Ulcerative Colitis A Gastrointestinal Disease
Stage 4 Bedsore Prevention
The best way to prevent a stage 4 bedsore is by being proactive. If your loved one is at risk for bedsores, you can help them take the following precautions.
To prevent stage 4 bedsores, you can:
- Avoid buttons on clothes and wrinkles in bedding
- Avoid doughnut cushions, as they can add pressure to surrounding areas
- Change bedding and clothing on a regular basis
- Check skin daily
You May Like: Ulcerative Colitis Surgery Recovery Time
Appendix 2 Glossary Of Nma Terms
Armspecific outcomes/armlevel data: raw outcome data or risk) for each arm of the trial .
Assumptions for NMA: in common with all metaanalysis, the true treatment effect across trials is assumed to be described by a fixedeffect or randomeffects model. Additionally, transitivity is assumed and, concurrently, exchangeability and consistency.
Baseline risk: the absolute risk of the outcome in the ‘control’ group. This is affected by the presence of prognostic factors. Some authors have used the baseline risk as a proxy effect modifier, but in general the effect estimate is independent of the baseline risk on the other hand, the absolute risk difference depends on baseline risk.
Bayesian approach: the explicit quantitative use of external evidence in the design, monitoring, analysis, interpretation of a healthcare evaluation. In the Bayesian paradigm, prior beliefs about parameters in the models are specified and factored into the estimation. Posterior distributions of model parameters are then derived from the prior information and the observed data. In NMA, it is common to use noninformative priors for effect estimates.
Coherence/consistency: the direct effect estimate is the same as the sum of the indirect effect estimates.
Contrast/comparison/studylevel data: outcome data for the comparison .
Credible interval : the 95% credible interval is the range within which the mean value lies with posterior probability of 95%.
Studylevel data: see contrast.
Analysis
Recommended Reading: How To Treat Ulcers In The Colon
Who Is At Risk For A Stage 2 Bedsore
Nursing home residents that rely on staff members to help them move are at a higher risk of stage 2 bedsores. Other factors, described below, can also put seniors at risk of bedsores.
Certain Medical ConditionsJohns Hopkins Medicine notes that elders with circulation issues and diabetes are more likely to suffer from bedsores.
IncontinenceThe U.S. National Library of Medicine notes that incontinence can make skin problems more likely. Feces and urine can make nearby skin moist, increasing the risk of irritation. Further, adult diapers can trap waste, allowing them to damage skin unless they are quickly changed.
MalnourishmentMalnourishment reduces overall health and weight two factors that make bedsores more likely. It also may take longer for someone to heal from a bedsore if theyre malnourished and underweight.
Bedsores Caused By Neglect
Bedsores are also called pressure sores because they are usually caused by prolonged pressure on a specific area of the body. Other factors that can put nursing home residents at risk are malnutrition, dehydration, and excessive friction on the skin. These causes are almost always preventable and in some cases are signs of serious neglect or abuse.
Many stage 2 bedsores could have been prevented with better care, more movement, or more frequent skin checks. Sometimes nursing homes fail to notice stage 1 sores or improperly treat them, allowing them to develop into stage 2 sores.
Families trust nursing homes to properly care for their loved ones. A nursing home is responsible for keeping their residents safe, healthy, and happy. Caretakers in nursing homes should monitor the nutrition, hydration, and skin health of their residents.
You may need to take legal action if you believe your loved ones bedsores were caused by neglect or abuse at a nursing home. If your loved one is not receiving proper care at their nursing home, please contact us for a free case evaluation.
Navigate This Page
Read Also: Best Supplement For Horses With Ulcers
How Are Bedsores Treated
Specific treatment of a bedsore is discussed with you by your healthcare provider and wound care team and based on the severity of the condition. Treatment may be more difficult once the skin is broken, and may include the following:
- Removing pressure on the affected area
- Protecting the wound with medicated gauze or other special dressings
- Keeping the wound clean
- Removing the damaged, infected, or dead tissue
- Transplanting healthy skin to the wound area
- Negative pressure wound therapy
Healthcare professionals will watch the bedsore closely. They will document size, depth, and response to treatment
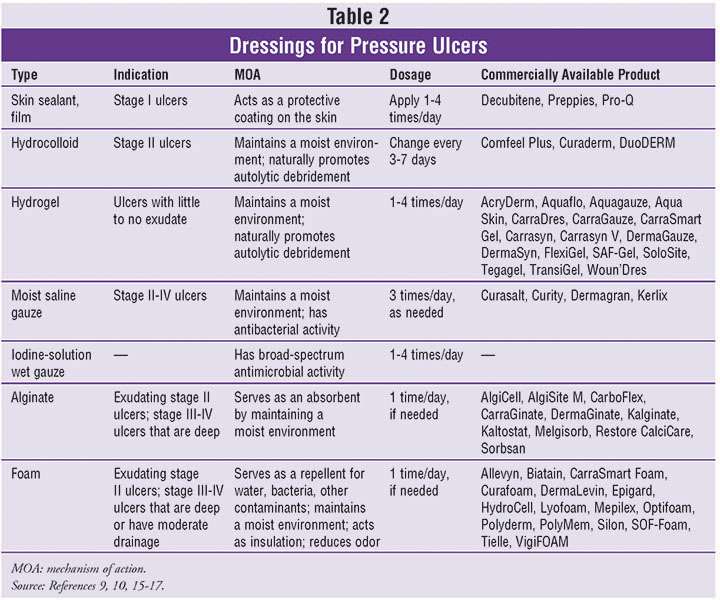
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation |
|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
You May Like: Black Tarry Stools Ulcerative Colitis
Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here’s how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should move or be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn’t rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can’t see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
How Do I Get Rid Of An Ulcer On My Butt
Caring for a Pressure Sore
Recommended Reading: Ulcer On White Of Eye
How To Prevent Pressure Ulcers On The Buttocks
The first article in this series identified what a pressure ulcer is and explained how pressure ulcers can form when pressure is applied to an area of the body over a long period of time. This pressure restricts the blood flow through the skin and tissue, starving the bodys cells of oxygen and causing them die and causing the skin and tissue around the area to break down.
The prevention and treatment of pressure ulcers is essential as they can range in severity from patches of discoloured skin to open wounds that expose the underlying bone or muscle and they can be painful, debilitating and life threatening.
Causes Of Itchy Bumps On Buttocks
What causes water blisters on buttocks? There is an array of causes that might be causing you the bumps or the painful blister on buttocks. The symptoms in terms of how severe itching or pain is will depend on what the underlying cause of the blisters is.
Some causes might be mild and clear on their own without any medical treatment. For some causes, due to their infectious nature, urgent treatment to limit its spread is highly recommended. Some of the common cause of blister on buttocks might include the following.
Read Also: How To Manage Ulcerative Colitis Pain
Also Check: Infected Leg Ulcers In The Elderly
Diagnosis Of A Decubitus Ulcer
Wound care physicians and nurses experienced in pressure ulcers are often consulted for decubitus ulcer diagnosis. Medical personnel may take samples of the pressure ulcer tissue and fluid to look for bacteria or cancer. They may also do blood cultures, bone scans or other tests depending on the seriousness of the ulcer. In addition, they will evaluate the condition of the ulcer according to:
- The size of the decubitus ulcer and depth of the crater
- What kind of tissue is affected by the ulcer: skin, bone, or muscle
- The color of the ulcer and skin around it
- The tissue death caused by the ulcer
- The presence of infection, bleeding or foul odor
Sores On Buttocks Cheek
The buttocks cheek is prone to skin infections that may be difficult to notice. Infection of the hair follicles also called folliculitis are common. Such infection will in most cases heal on their own without treatment. They may also spread causing boils which will require antibiotics to cure.
Sores on buttock cheek are likely to affect people who are bed bound. The sores can become quite severe leading to ulceration and a significant loss of skin around the buttocks. A number of causes that could lead to sores on buttocks include:
- Skin conditions such as rashes
Below are the pictures of how sores on buttocks look like
Don’t Miss: Do You Still Have Ulcerative Colitis After Colectomy
Stages Of Pressure Ulcers And Treatment
Pressure ulcers can progress in four stages based on the level of tissue damage. These stages help doctors determine the best course of treatment for a speedy recovery.
If caught very early and treated properly, these sores can heal in a matter of days. If left untreated, severe bedsores may require years to heal.
Agreements And Disagreements With Other Studies Or Reviews
We have been unable to identify any network metaanalyses directed at healing pressure ulcers and incorporating both dressings and topical agents. The AHRQ guideline reviewed the evidence for dressings in a series of pairwise comparisons and stated that overall, they did not find substantial evidence to support certain local wound applications over others . The most recent NICE guideline on the prevention and management of pressure ulcers considered all RCT evidence on dressings and separately all RCT evidence on topical agents. NICE recommendations are to not use saline gauze dressings and for the health professional and adult to discuss the type of dressing to use, taking into account pain and tolerance, position of the ulcer, amount of exudate and frequency of dressing change. These recommendations rely heavily on consensus decisions, weakly supported by the evidence, and as such, agree with the findings of this review.
Donât Miss: Diabetic Foot Ulcer Treatment Guidelines
Recommended Reading: Acute Severe Ulcerative Colitis Guidelines
Failure Of Reactive Hyperaemia Cycle
It is a known fact that tissue distortion causes ischaemia that in turn stimulates protective movements to relieve pressure and circulatory activity to restore normal blood flow in the affected areas. These protective movements are often reflexes as the person is unaware of making them. However, if these prompt actions prove insufficient to relieve ischaemia, the central nervous system is stimulated by constant signals of discomfort and pain to make sure that the pressure is relieved before any permanent damage occurs. Once the pressure is relieved, and the circulation restored, local capillaries begin to dilate and increased blood flow takes place, referred to as reactive hyperaemia. As a result, a bright pink transitory patch appears on the skin, often called blanching erythema because it blanches on pressure unlike the dull red non-blanching erythema that indicates tissue damage . Reactive hyperaemia ensures a rapid restoration of oxygen and carbon dioxide balance it also flushes out waste products. Erythema subsides as soon as tissues are restored to their resting state.
Various grading of pressure ulcer . A very severe trochanteric pressure ulcer where destruction is so severe that the femoral head dislocated and came out
Bone And Joint Infection
Infection can also spread from a pressure ulcer into underlying joints and bones .
Both of these infections can damage the cartilage, tissue and bone. They may also affect the joints and limbs.
Antibiotics are required to treat bone and joint infections. In the most serious of cases, infected bones and joints may need to be surgically removed.
Also Check: Things Not To Eat If You Have An Ulcer
Positioning And Support Surfaces
Preamble: Pressure and compression to soft tissue play a role in the etiology of pressure ulcers. Patient positioning and methods to reduce pressure-related tissue damage are recognized as important treatment components. While there are limited definitive studies, the best current evidence and expert opinion suggest the following guidelines.
Guideline #1.1: Establish a repositioning schedule and avoid positioning patients on a pressure ulcer.
Principle: Pressure ulcers are thought to result from compression of soft tissues against a bony prominence. It is reasonable to assume that pressure on an ulcer can result in delayed healing. Patients should be repositioned to relieve pressure over bony prominences. The exact turning interval is not known and is derived empirically. Reductions in pressure incidence have been achieved, but positioning is not universally effective.
Evidence: