How Does Ulcerative Colitis Affect Colorectal Cancer Risk
Were about to get into the more nerve-wracking information here, so before we do, lets be really clear: Having ulcerative colitis is in no way a guarantee that youll get colorectal cancer. But the condition does increase your risk of developing cancer in your colon and rectum . To make things less confusing, even though ulcerative colitis increases your risk of both colon cancer and colorectal cancer, well refer to colorectal cancer throughout since its more encompassing.
Now, lets talk about that increased risk. Overall, people who have chronic IBD are nearly twice as likely to develop colorectal cancer than the general population, according to the American Cancer Society Colorectal Cancer Facts & Figures 2017-2019 Report. Its important to recognize that the risk varies tremendously based on the type, severity, and location of the colitis, Paul Oberstein, M.D., director of the Gastrointestinal Medical Oncology Program at NYU Langones Perlmutter Cancer Center, tells SELF.
People with colitis affecting the entire colon are at greater risk of these cancers, Dr. Oberstein says. On the other hand, people with colitis on only certain portions, like the left side, are generally considered to be at moderate risk, and those who have colitis only in the rectum are at lower risk, possibly similar to that of people without ulcerative colitis, according to some studies.
Colorectal Cancer Risk Remains Despite Modern Treatment For Ulcerative Colitis
Patients with the inflammatory bowel disease ulcerative colitis have a higher risk of dying from colorectal cancer, despite modern therapy, even though the risk has declined in recent years. This is according to a new study published in the scientific journal The Lancet by a team of Swedish and Danish researchers.
Previous research has shown that patients with ulcerative colitis have an increased risk of colorectal cancer. Screening recommendations are therefore in place for this patient group. But to what extent have new therapeutic methods helped to reduce this risk? This much-debated question has now found new answers. A large study involving 96,000 patients diagnosed with ulcerative colitis between the years 1969 and 2017 has now shown that these patients run a higher risk of developing and dying of colorectal cancer.
The risk of colorectal cancer has dropped substantially over the past 30 years, but in spite of this patients who have had access to modern treatments for ulcerative colitis and screening for colorectal cancer still have a significantly elevated risk, says Ola Olén, senior researcher at the Department of Medicine in Solna at Karolinska Institutet in Sweden.
Visiting Your Doctor Regularly
Seeing your doctor at least once a year, even when your Crohns or Colitis is in remission, can ensure you remain on the most appropriate treatment, and that you have regular checks for any sign of cancer. Of course, if you have anychanges in symptoms at any time, it is best to speak to your doctor as soon as you can.
Read Also: How To Prevent Ulcers In The Stomach
Never Skip A Regular Screening
People who have ulcerative colitis that extends past the sigmoid colon should start annual colonoscopiesa test where doctors use a long, flexible tube with a camera attached to inspect the inside of the colonno later than eight years after symptoms appear, says Dr. Ehrlich.
Your doctor may also take a biopsy during your screening, especially if he or she notices dysplasia or cells that look cancerous.
If youve previously had dysplasia or a bile duct inflammation called primary sclerosing cholangitis, your physician may spray a blue dye onto the colon walls to spot cancerous areas more easily.
Risk Factors For Colorectal Cancer In Ulcerative Colitis
The most important risk factors for UC-associated CRC are disease duration and extent. The possible mechanisms include chronic inflammation and as the duration of chronic bowel inflammation increases, so does the risk for colorectal dysplasia and CRC. In some studies, this annual risk rises exponentially with a duration beyond 30 years. This has led some guidelines to recommend surveillance colonoscopy every 1 year to 3 years between years 8 and 20 and every 1 year to 2 years thereafter. In contrast, some of the recently published population-based studies could not demonstrate a clear-cut relation in UC duration,and cancer risk or the gradual increase of the risk was much lower.
In the landmark trial by Ekbom et al, more than 3000 UC patients were followed up and the risk for CRC increased gradually from 1.7-fold in proctitis and 2.8-fold in left-sided colitis to 14.8-fold in pancolitis, compared to the general population. Most studies including the meta-analysis by Eaden et al, have come to similar conclusions. The overall prevalence of CRC among patients with UC in all 116 studies was 3.7%, but when restricted to the 35 studies that stratified their analyses by extent of UC, the prevalence of CRC among patients with extensive involvement rose to 5.4%.
You May Like: How Do You Die From Ulcerative Colitis
Big Difference Between Patient Groups
An important result of the study is that the risks are indeed elevated but there are major differences from one patient group to another, says Olén.
At particularly high risk of developing colorectal cancer are the patients with extensive colitis, primary sclerosing cholangitis , heredity for colorectal cancer susceptibility or childhood onset ulcerative colitis.
According to co-author and Professor Jonas F Ludvigsson at the Department of Medical Epidemiology and Biostatistics, the study indicates a need to develop the care provided for these patients even further.
Our study shows that screening and treatment of these patients can likely be further improved, since patients with ulcerative colitis are still more likely to die of colon cancer, he says.
Doctors Who Treat Ulcerative Colitis
Cleveland Clinic recommends beginning UC treatment with your usual doctor. If more testing is needed, theyll refer you to a gastroenterologist or colorectal surgeon for a colonoscopy. A gastroenterologist treats digestive issues. Colorectal surgeons conduct colon and rectum procedures. GIs manage UC treatment.
Other doctors will also help. A nutritionist will ensure you eat things your body can handle and obtain enough nutrientsa dermatologist for skin disorders and a rheumatologist for joint difficulties. Living with a chronic ailment is difficult therefore, physicians suggest visiting a psychologist for depression or anxiety. A third of UC patients require colorectal surgery.
You May Also Like
The Crohns & Colitis Foundation advises choosing a UC specialist carefully. Check that the doctor accepts your insurance, is nearby, and has a good bedside manner.
Don’t Miss: What Can I Take For Ulcerative Colitis
Why Regular Colorectal Cancer Screenings Are So Important
Colorectal cancer is curable, especially in the early stages. The best chance of complete remission comes with finding polyps early that need to be removed before they turn into cancer. This makes the entire process easier on you, less invasive, reduces the chance of it spreading to other organs, and is less expensive than late-stage cancer treatment.
To find colorectal cancer early, you need to stick with a regular cancer screening schedule. If you have ulcerative colitis or other medical conditions that put you at risk for colorectal cancer, your primary care doctor may recommend starting cancer screenings younger than the average age of 45. Screening for colon and rectal cancer can be done with an at-home stool test using a test such as a colonoscopy or a sigmoidoscopy. The right test for you, based on the severity of the UC, will be determined by your physician.
Colorectal Cancer Risk Factors
A risk factor is anything that raises your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a persons age or family history, cant be changed.
But having a risk factor, or even many, does not mean that you will get the disease. And some people who get the disease may not have any known risk factors.
Researchers have found several risk factors that might increase a persons chance of developing colorectal polyps or colorectal cancer.
Don’t Miss: Signs You Have Ulcerative Colitis
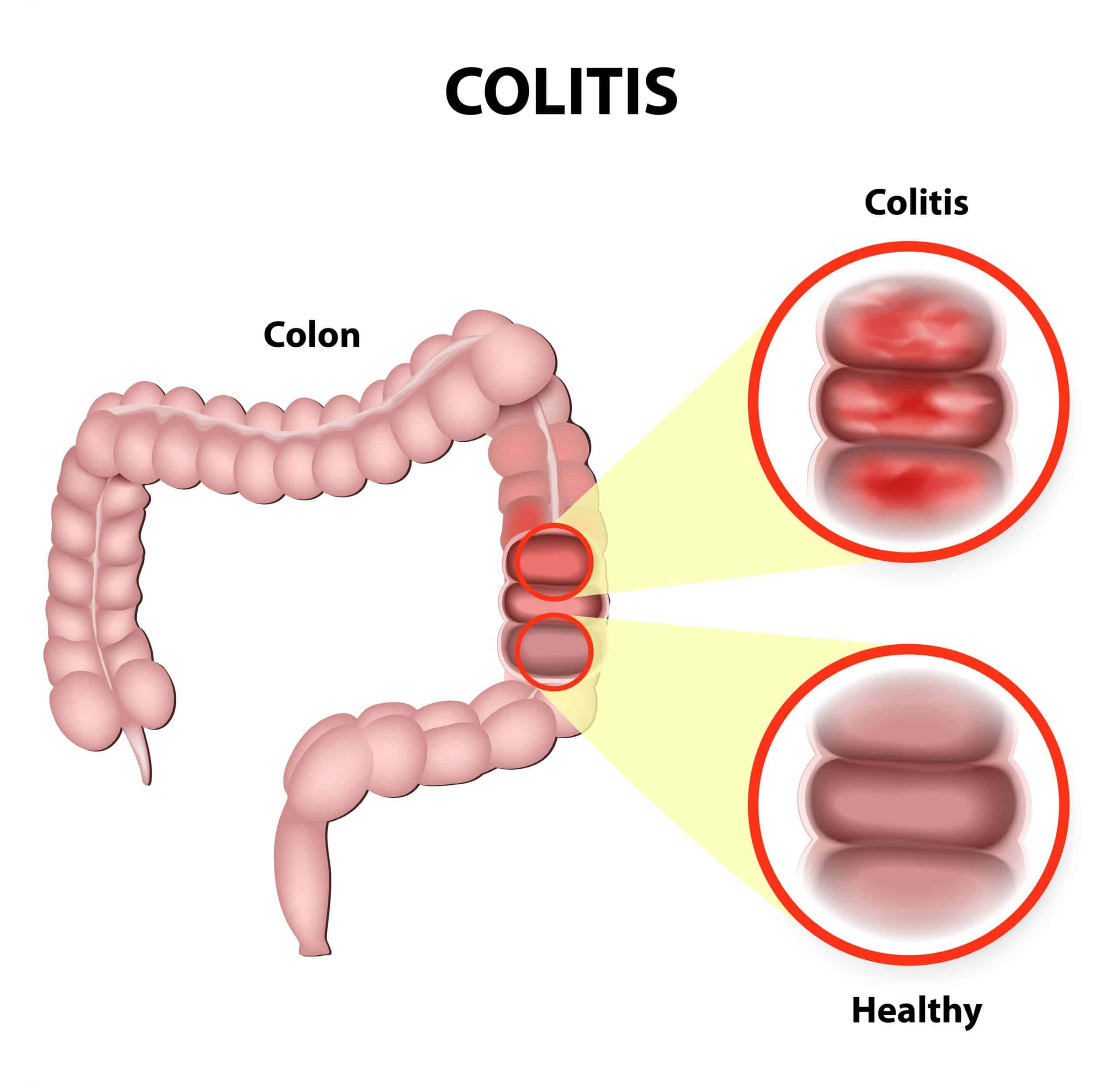
Chronic Inflammation In The Colon From Ulcerative Colitis
UC causes chronic inflammation that affects the cells lining the large intestine . Chronic inflammation, like that caused by ulcerative colitis, is an ongoing issue. And when left untreated it can lead to the development of cancer in the colon or rectum.
Chronic inflammation is known to:
- Damage your colon lining and destroy cells that repair other cells. Without repairs, damage can occur to DNA in your colon cells, contributing to ulcer development.
- Increase the level of molecules that promote cancerous tumor growth.
- Make you more susceptible to infections, which help cancer cells grow and multiply.
Evolutionary Biomarkers: A Novel Approach Merging Biology And Mathematics
The stochastic nature of evolutionary changes requires adequate time for carcinogenesis to progress normal cell phenotype to malignancy in the human body. Using mathematical models, we can formulate mathematical expressions describing these evolutionary changes, and use the expressions to relate these evolutionary parameters to age-dependent epidemiological cancer incidence curves . In addition to the chronological age of the patient as an initial biomarker of CRC risk, biological aging of the colitic bowel itself may be considered as a potential marker of progression to neoplasia due to its prominence in the pathogenesis of IBD carcinogenesis explained above. The concept is based on measuring both the extent and speed of genetic evolution as a proxy of how close to cancer the cells have become . Tissue age is difficult to measure in vivo, but can be estimated with computational methods like Bayesian inference that have been used in molecular clocks applied to somatic epigenetic and genomic data from non-dysplastic Barrett’s esophagus, a precursor of esophageal adenocarcinoma that is characterized by intestinal metaplasia, driven by chronic acid- induced inflammation .
Recommended Reading: Low Dose Naltrexone Ulcerative Colitis
Colorectal Carcinogenesis In Ibd Is Driven By Accelerated Cell Turnover And Premature Colonic Aging
Studies using Ki67, a cellular marker expressed during the active phases of the cell cycle, demonstrate an expanded proliferative zone in crypts from both regenerating IBD epithelium and early dysplasia when compared to normal colonic crypts . The precise stem cell population responsible for regenerating the human colonic epithelium in IBD is uncertain, with evidence from murine studies suggesting dynamic contributions during the inflammation and regeneration phases. LGR5+ expression drops dramatically during the acute stages of colitis but increases dramatically during regeneration other studies confirm that LGR5+ expressing stem cells may be very sensitive to intestinal injury but nonetheless crucial to crypt regeneration . Inflammation has been shown to recruit long-lived and hitherto quiescent DCLK1+ tuft cells from the crypt wall that can acquire stem cell properties in the absence of LGR5+ stem cells, reconstituting the entire crypt, including the LGR5+ stem cell niche. Interestingly, these DCLK1+ cells did not proliferate or initiate neoplastic progression following conditional APC knockdown without the addition of an inflammatory stimulus .
Having An Inherited Syndrome
About 5% of people who develop colorectal cancer have inherited gene changes that cause family cancer syndromes and can lead to them getting the disease.
The most common inherited syndromes linked with colorectal cancers are Lynch syndrome and familial adenomatous polyposis , but other rarer syndromes can increase colorectal cancer risk, too.
Lynch syndrome
Lynch syndrome is the most common hereditary colorectal cancer syndrome. It accounts for about 2% to 4% of all colorectal cancers. In most cases, this disorder is caused by an inherited defect in either the MLH1, MSH2 or MSH6 gene, but changes in other genes can also cause Lynch syndrome. These genes normally help repair DNA that has been damaged.
The cancers linked to this syndrome tend to develop when people are relatively young. People with Lynch syndrome can have polyps, but they tend to only have a few. The lifetime risk of colorectal cancer in people with this condition may be as high as 50% , but this depends on which gene is affected.
Women with this condition also have a very high risk of developing cancer of the endometrium . Other cancers linked with Lynch syndrome include cancer of the ovary, stomach, small intestine, pancreas, kidney, prostate, breast, ureters , and bile duct. People with Turcot syndrome who have a defect in one of the Lynch syndrome genes are at a higher risk of colorectal cancer as well as a specific type of brain cancer called glioblastoma.
Familial adenomatous polyposis
Don’t Miss: How To Heal Duodenal Ulcer
From Colitis To Cancer: Translational Implications Of Utilizing An Evolutionary Approach
Pathogenic genomic alterations are known to occur in phenotypically normal epithelium many years before a cancer forms . Enumeration of these mutations may aid in risk stratifying patients who will more likely progress to IBD-CRC for more aggressive surveillance and treatment, while reducing surveillance requirements for lower risk patients. By using the aforementioned evolutionary approach, we envisage a more personalized approach to cancer risk assessment that combines patient demographic details and endoscopic features with genomic assays.
Quantification of immune-epithelial cell co-evolution is an important area for future research. Both cell populations can be described quantitatively by complex system models with marked plasticity, resulting in a near infinite possible set of permutations , and a susceptibility to sustained external selection pressures that can promote and fix clinically deleterious traits . As the selfish drive of the individual colon cancer cell to expand comes at the expense of the multicellular human host, so the same approach can be used to understand and model the conditions driving the selfish activation and/or expansion of aberrant immune cell populations.
Living With Ulcerative Colitis
Ulcerative colitis, a disease that causes inflammation and sores in the digestive tract, affects everyone in a different way. About 10% of people get better after one attack, but it’s more likely that you’ll have flares that come and go throughout your life.
You may go weeks or years without any symptoms. That’s called remission. The longer you go without a flare, the better your overall health will be.
Your doctor will likely give you medicine to control inflammation and other symptoms.
If you don’t feel like your UC is under control, talk to your doctor. They may want to change your medicine dose or switch you to a different drug. If that doesn’t work, you may need surgery.
Don’t Miss: Diabetic Foot Ulcer Early Signs
Diagnostic Et Traitement De La Colite Ulcreuse
Il n’y a pas de remède contre la colite ulcéreuse, mais des changements de mode de vie et des médicaments peuvent aider à gérer les poussées. Pour confirmer un diagnostic de colite ulcéreuse et exclure d’autres affections présentant des symptômes similaires, un patient peut subir un ou plusieurs des tests suivants :
- Prise de sang : Un test sanguin peut être utilisé pour vérifier l’anémie ou des signes d’infection.
- Test d’échantillon de selles : Un test de laboratoire d’un échantillon de selles d’un patient peut vérifier l’inflammation du côlon et exclure une infection causée par une bactérie, un parasite ou un virus.
- Coloscopie: Dans ce test, un médecin utilise un tube mince et éclairé pour examiner la muqueuse du côlon afin de rechercher des ulcères, des saignements ou des excroissances anormales.
- Biopsie: Une biopsie peut être effectuée dans le cadre d’une procédure d’endoscopie ou de coloscopie pour examiner un échantillon de tissu.
- Tests d’imagerie: Une radiographie ou un scanner peuvent être recommandés pour exclure d’autres conditions et vérifier l’inflammation du côlon.
Un certain nombre de médicaments peuvent aider à traiter la colite ulcéreuse. Ceux-ci inclus:
- Médicaments anti-inflammatoires
- Médicaments anti-diarrhéiques
- Pilules antispasmodiques, qui réduisent les crampes
Certaines modifications du mode de vie peuvent aider à atténuer les symptômes de la colite ulcéreuse, telles que :
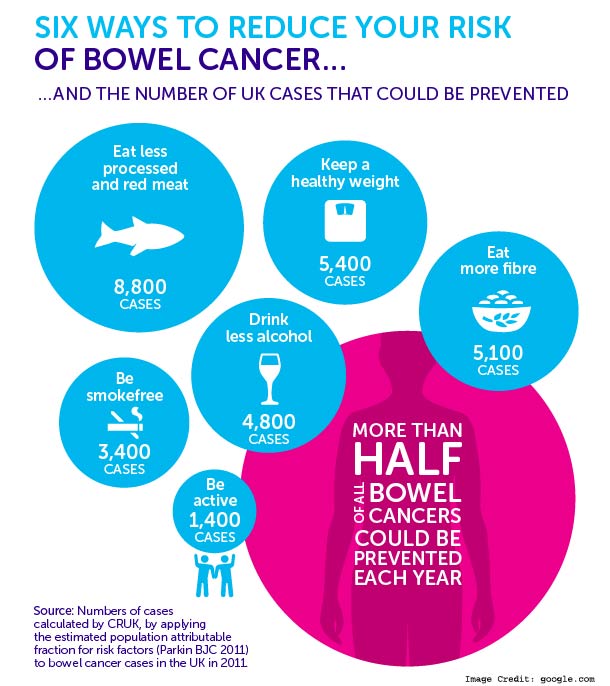
Reducing How Much Processed And Red Meat You Eat
A diet high in saturated fats and red meat may increase the risk of bowel cancer. If you eat more than 90g of red or processed meat a day, its recommended that you reduce your intake to 70g a day.Red meat includes: deli meats such as salami pates canned meat such as corned beef sliced luncheon meats, including those made from chicken or turkey.You can find more information on sizes and cutting down on red and processed meat on the NHS website.There is more information about diet in our food section.
You May Like: How To Prevent Hospital Acquired Pressure Ulcers
You Need To Know Your Family History
Among those with ulcerative colitis, not all cancer risk is the same.
A family history of colorectal cancer doubles your odds of getting the disease, according to a study in the World Journal of Gastroenterology, as compared to patients without a family history.
Tell your doctor if you have a family history of colorectal cancer familial adenomatous polyposis, a condition in which the intestine is lined with benign polyps or Lynch syndrome, a genetic disorder characterized by polyps in the colon.
All raise your cancer risk.
Colon Cancer Risk Factors You Cant Control
Some colon cancer risk factors are not under your control. This list includes:
Age While there are a growing number of people being diagnosed with early-onset colorectal cancer, the majority of people with the disease are older than 50.
Personal or family history If you have had colorectal polyps , you are more likely to develop colorectal cancer. This is especially true if the polyps are big, appear in multiples, or contain cells with noncancerous abnormalities .
A family history of colorectal cancer is another risk factor. One out of three people diagnosed with colon cancer or rectal cancer have family members with the disease.
Having had colorectal cancer makes you more likely to get it again, even if you were successfully treated the first time.
A personal history of inflammatory bowel disease Inflammatory bowel disease, which includes Crohns disease and ulcerative colitis, causes chronic inflammation of the colon. This can lead to dysplasia, which may eventually become cancer.
African-American or Eastern European Jewish heritage African-Americans have one of the highest rates of colorectal cancer of any racial group. The American College of Gastroenterology suggests that African-Americans begin colorectal screening at age 45, five years earlier than nonAfrican-Americans at average risk.
Jews of Eastern European descent, called Ashkenazi Jews, are also at high risk compared with other ethnic groups.
Recommended Reading: Crohn’s Disease Vs Ulcerative Colitis