Psychological Comorbidities Work Productivity And Health
The prevalence of comorbid psychiatric illnesses, defined as a HADS score 8, among the patients was 33.7% for anxiety and 41.8% for depression . Of these, significant mood disorders requiring psychological interventions, defined by a HADS score 11, were identified in 16.7% and 20.6% of patients. There was no significant difference in the mean HADS score according to disease severity .
Distribution of the study population according to the Hospital Anxiety and Depression Scale .
Your Mental Health And Ulcerative Colitis
Living with UC can be stressful and often comes with periods of deep frustration and sadness. But if you find yourself anxious or depressed most of the time for several weeks or longer, its important to seek help from a mental health professional.
Rates of depression are higher in people with UC than the general population, and anxiety is also common in people with UC, according to the Crohns & Colitis Foundation. Its important to address these issues as seriously as you would any other symptom or complication of UC.
For more information on UC and mental health:
- Practicing yoga or tai chi
- Spending quality time with friends or family
- Participating in any activities that you enjoy
Your Family Friendships And Ulcerative Colitis
Talking to your friends about UC may not come naturally with every single person. Not everyone will truly understand why youve been canceling plans, and they may think youre simply not interested in them anymore, especially if you dont look obviously ill.
For tips for talking to friends and family about UC:
Recommended Reading: Worst Foods To Eat With An Ulcer
Alicias Story Ulcerative Colitis
“I remember being on the bus back from college one day and felt the most excruciating pain Id ever had in my stomach. I was 17, terrified and in pain”Alicia’s story from diagnosis of Ulcerative Colitis to sharing her story and experiences with thousands as she travels the globe.
My first memory of Ulcerative colitis was seeing blood in the toilet. I googled it and thought the worst. But I thought itd pass. Days turned to weeks and months, each time I went the toilet more and more blood appeared. Clots. I remember being on the bus back from college one day and felt the most excruciating pain Id ever had in my stomach that I needed to sit down and get off at the next stop. Even this wasnt enough for me to raise my concerns, I was 17, terrified and in pain.
Aged 18, I was diagnosed with Ulcerative Proctitis.
It was a bizarre sensation, I was partly relieved there was an answer to feeling so rubbish but also scared at the information given, confused the specialist addressed the condition like there was no cure. Looking back it took a really long time to comprehend this was my forever.
The next two years was a rollercoaster of one month being OK, the next not so fine, blood, mouth ulcers, fevers, aching joints, abdominal pains & weight loss.
This meant a new treatment plan immunosuppressant Azathioprine. The first few weeks taking this medication made flares seem like a walk in the park. After persevering though, I slowly started to gain my normality back.
A Case Of Newly Diagnosed Ulcerative Colitis
Accepted:Received:Doi:Cite Code:
Alnt Kodu:Satlm M. ve ark. Yeni tan alan bir ülseratif kolit olgusu.Jour Turk Fam Phy 2020 11 : 204-208. Doi: 10.15511/tjtfp.20.00404.
Ulcerative Colitis is an inflammatory bowel disease that is frequently encountered in young people, with an attack and can be diagnosed only with pathology. It is not among the first diagnoses that come to mind because of the low frequency of occurrence even in the presence of related symptoms in primary health care services. In our case, we presented a patient who was admitted to our Family Medicine Outpatient Clinic and was diagnosed after ulcerative colitis.
Recommended Reading: Stage 1 Vs Stage 2 Pressure Ulcer
Diet & Lifestyle Changes
Date Written: 09-2020
This information is intended for educational purposes and is not intended to replace recommendations that have been provided by your Physician and Health Care Team. Healthy eating objectives for IBD include managing symptoms, ensuring and optimizing adequate intake, promoting healing, reducing complications and meeting other relevant personal needs.
There is no miracle cure for Crohns and ulcerative colitis, through a special diet, food combinations, or exclusions of select foods or nutrients. Individuals with IBD, including Crohns disease and ulcerative colitis may feel well, or ill during a flare-up, leading to variations in appetite and nutritional intake depending on the state of their IBD.
During a flare-up and even when feeling well, it is important to be well-nourished to support healing, build strength, reduce inflammation and optimize nutritional intake. If you feel ill during a flare-up, making effective changes to diet may potentially help you to manage symptoms.
You may find some improvements or worsening in your symptoms based on certain foods. Keep a diary, it is worth tracking food intake to try and determine possible symptom triggers. However, it is important to assess whether other factors like stress, hormones, level of sleep and physical activity contribute to worsening of symptoms rather than merely foods as the cause.
Consume adequate amounts of fluid intake to move wastes through your system and prevent dehydration.
Do You Need To Avoid Any Food Groups Gluten Or Lactose
Unless you have symptoms to specific foods, do not remove them from your diet. Everyone is different, and what causes issues for one person may not have the same reaction for others. If you remove foods from the diet, make sure to check your tolerance to these foods from time to time, as symptoms can vary over time. Also, restricting foods can lead to extensive lists of foods excluded from the diet, which can increase the risk of nutrient deficiencies.
Don’t Miss: Why Do I Keep Getting Mouth Ulcers
When You’re Ready Let Others Know
- It Takes Guts to talk about Crohns and Colitis, but weve got the words to help you break the ice. Create your own personalised talking toolkit and start your conversation today.
- Our information on Employment has tips on informing your boss and colleagues about how your condition may affect you.
- Your friends and family may find our information on how to support someone with Crohns or Colitis helpful in understanding what youre going through. They can also take part in our immersive In My Shoes app, which allows anyone to experience 24 hours of what its like to live with Crohns or Colitis.
- – were always looking for people who are willing to share experiences which help us provide support and representation to everyone affected by Crohn’s and Colitis.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
You May Like: Best Way To Heal Stomach Ulcers
Your Child With Inflammatory Bowel Disease: A Family Guide For Caregiving
Its natural to worry about how your child will cope with things like school and sports, especially when theyre living with IBD.
This book answers questions about managing your childs UC. Written by a team of UC experts who work with children and their families, it provides details on treatments and medications used for children and teens.
The tone is knowledgeable and empathetic, and the information is presented clearly. It answers many questions parents and caregivers have about caring for their child.
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
You May Like: Can Diet Help Ulcerative Colitis
Abdominal And Rectal Pain
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
What Caused My Disease
The short answer: You didnt, so please dont blame yourself. The exact cause of ulcerative colitis isnt known, but there are a few theories about what could cause the disease. One is an immune system malfunction, meaning that when your immune system tries to fend off a virus or bacteria, it reacts in an abnormal way by targeting the cells in your digestive tract too, the Mayo Clinic says.
Genetics may play a role as well. Ulcerative colitis is more common in people who have family members with the disease, the Mayo Clinic says. With that said, its not an overwhelmingly strong connectionmost people with ulcerative colitis dont have a family history of the disease. However, knowing that you have it can help put the symptoms of the disease on the radar of your loved ones just in case, Ashish Atreja, M.D., an associate professor of gastroenterology at the Icahn School of Medicine at Mount Sinai, tells SELF.
Keep in mind, though, that your loved ones should only be tested if they’re symptomatic, Megha Kothari, M.D., a hepatologist and gastroenterologist at NewYork-Presbyterian Medical Group Brooklyn, tells SELF. Theres no need for them to get preemptive testing just because you have the condition.
Also, while there arent definitive answers in terms of ulcerative colitis causes, some people have found that things like stress and various foods and drinks can make their symptoms worse, the Mayo Clinic says.
Recommended Reading: Fmt Treatment For Ulcerative Colitis Uk
Ibd & Me Activity Book
This is a great free resource available on the Crohns & Colitis Foundation website. Its targeted to kids and teens who are navigating the world of IBD.
It includes ideas about how to talk to friends and teachers about IBD. It also has tips for dealing with sports, school, field trips, parties, and all sorts of other typical kid things.
These titles arent specific to UC but can be enjoyable books. Theyre great for anyone keen to learn more about the digestive tract and gut microbiome, and they can help you better understand how your body works.
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Don’t Miss: New Medicine For Ulcerative Colitis
Family Planning With Ulcerative Colitis
Planning for a pregnancy can be more difficult when you have UC. Youll want to be in the best possible physical condition, which means staying in remission if possible and this may mean deciding to keep taking medications for UC during your pregnancy.
But you may need to switch to a safer or more effective drug for your UC if you plan on becoming pregnant, so its essential to talk with your doctor ahead of time to map out a treatment strategy. And even if you do this, its possible that youll experience UC-related pregnancy complications or a pregnancy-related flare of your UC.
For more information about UC and pregnancy:
The Race Went Well But Symptoms Worsened
Gaul, now 42, of Marshall, Minnesota, had run marathons a couple of decades ago, but he wanted to improve on his time. He had done well running in more recent half-marathons, so he decided to train for the Sioux Falls Marathon, with the goal of a more competitive time.
The day of the marathon, I felt good, Gaul said. He felt as prepared as a person could be while dealing with his condition.
But I did wake up that morning, and I did have a loose bowel movement, so I thought, I need to be careful here because I dont want to have an accident during the Sioux Falls Marathon. So I did take some anti-diarrheal pills that morning, he said.
The race went well. Like many people, I struggled once I got to about mile 18, and I hit the wall, as they say, so I slowed down. I didnt finish as fast as I would have liked. Nevertheless, Gaul finished with a personal record that was more than a half-hour under his previous time.
Once the September marathon was over, Gaul cut back on training and thought he would feel better less tired. But his symptoms worsened further, and his first appointment with a specialist at Sanford Health, gastroenterologist Jorge Gilbert, wasnt until November.
Gaul thought he could make it, but in October he was experiencing personal records of a different kind: bowel movements. They were increasing up to 10 a day, with 15 on one particular day. They were waking him during the night.
Don’t Miss: What Is A Gastric Ulcer And What Is Its Cause
Dont Handle This Alone
It can be overwhelming to face flare-ups, so be sure to have family or friends you can talk to when you donât feel well. Or find a support group of other people who have UC.
Even if you arenât outgoing, reaching out to get support is key. This is a sign of strength, because youâre actively taking care of yourself.
âHaving a chronic disease adds a layer of difficulty and stress to life,â Streett says. Sharing what youâre going through gives people who care about you, and people who understand what youâre going through based on their own experiences, a chance to give you perspective and strength.
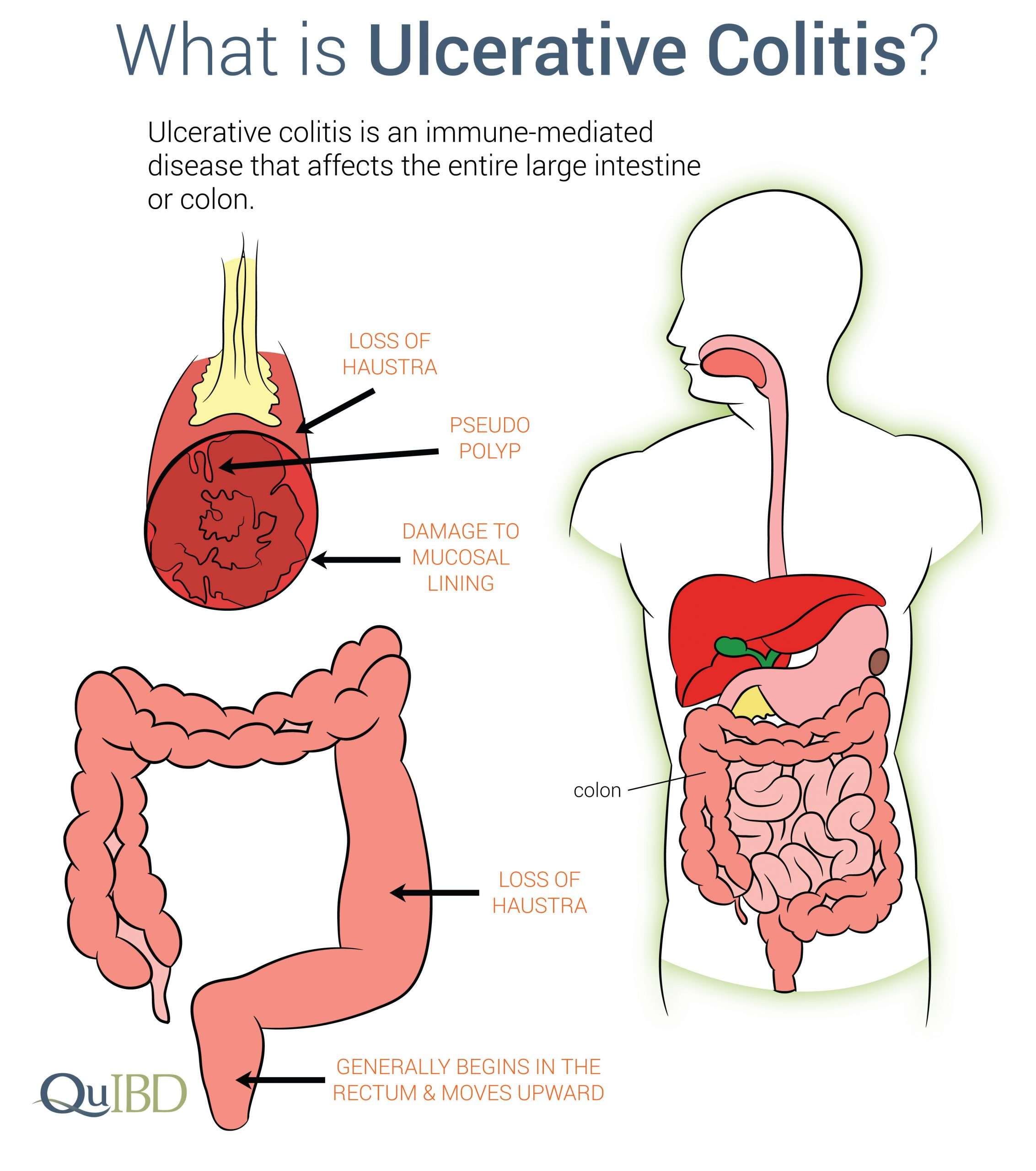
Ulcerative Colitis Causes And Risk Factors
Ulcerative colitis happens when your immune system makes a mistake. Normally, it attacks invaders in your body, like the common cold. But when you have UC, your immune system thinks food, good gut bacteria, and the cells that line your colon are the intruders. White blood cells that usually protect you attack the lining of your colon instead. They cause the inflammation and ulcers.
Doctors arenât sure why people get the condition. Your genes may play a role the disease sometimes runs in families. Other things in the world around you may make a difference, too.
Things that can affect your risk of getting ulcerative colitis include:
- Age. Itâs most likely if youâre between 15 and 30 years old or older than 60.
- Ethnicity. The risk is highest in people of Ashkenazi Jewish descent.
- Family history. Your risk could be up to 30% higher if you have a close relative with the condition.
Food and stress donât cause it, but they can trigger a flare of symptoms.
Also Check: Is Beer Bad For Ulcerative Colitis
Improving Remission Rates In Newly Diagnosed Paediatric Ulcerative Colitis
- Department of Paediatric Gastroenterology, Southampton Children’s Hospital, Southampton SO16 6YD, UKDepartment of Human Genetics and Genomics, University of Southampton, Southampton, UK
J Pediatr Gastroenterol Nutr.
The Lancet Gastroenterology & Hepatology
Lancet Gastroenterol Hepatol.
Gastroenterology.