Be Experimental With Fiber
Fibers are of two types soluble fibers and insoluble fibers. People with ulcerative colitis find that soluble fibers are better for them in helping them with their symptoms of the condition, while insoluble fibers tend to exasperate their conditions.
Soluble fibers can easily be found in many fresh foods like vegetables and fruits and more. Since fibers have a different effect on people with ulcerative colitis, your body may be able to handle a very small quantity of fiber at a time. Therefore, you must experiment with fiber and set your quota.
Reintroducing Your Usual Diet
Your IBD team and dietitian will give you information about returning to your usual diet after youve finished enteral nutrition. They may suggest reintroducing foods slowly so you can see if any foods affect your symptoms and to help you feel more confident about eating again. There are three ways of doing this:
- the elimination diet after excluding all foods, they are reintroduced one by one every few days, to see if they cause problems
- the Royal Free method this is similar to the elimination diet but foods are reintroduced more quickly, over a period of days rather than weeks
- the LOFFLEX diet this excludes foods high in fat and fibre.
There isnt much evidence to show how well these diets work, or whether one works better than another. Your dietitian will explain the benefits and risks of all your options.
Ive found that you have to be very careful on the internet as there are many websites claiming to cure IBD through untested diets and supplements which are not properly regulated and could be harmful and also expensive.
Zaineb
This is an extreme form of low carbohydrate diet that limits:
Read Also: Over The Counter For Ulcer Pain
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
Also Check: Most Common Symptoms Of Ulcerative Colitis
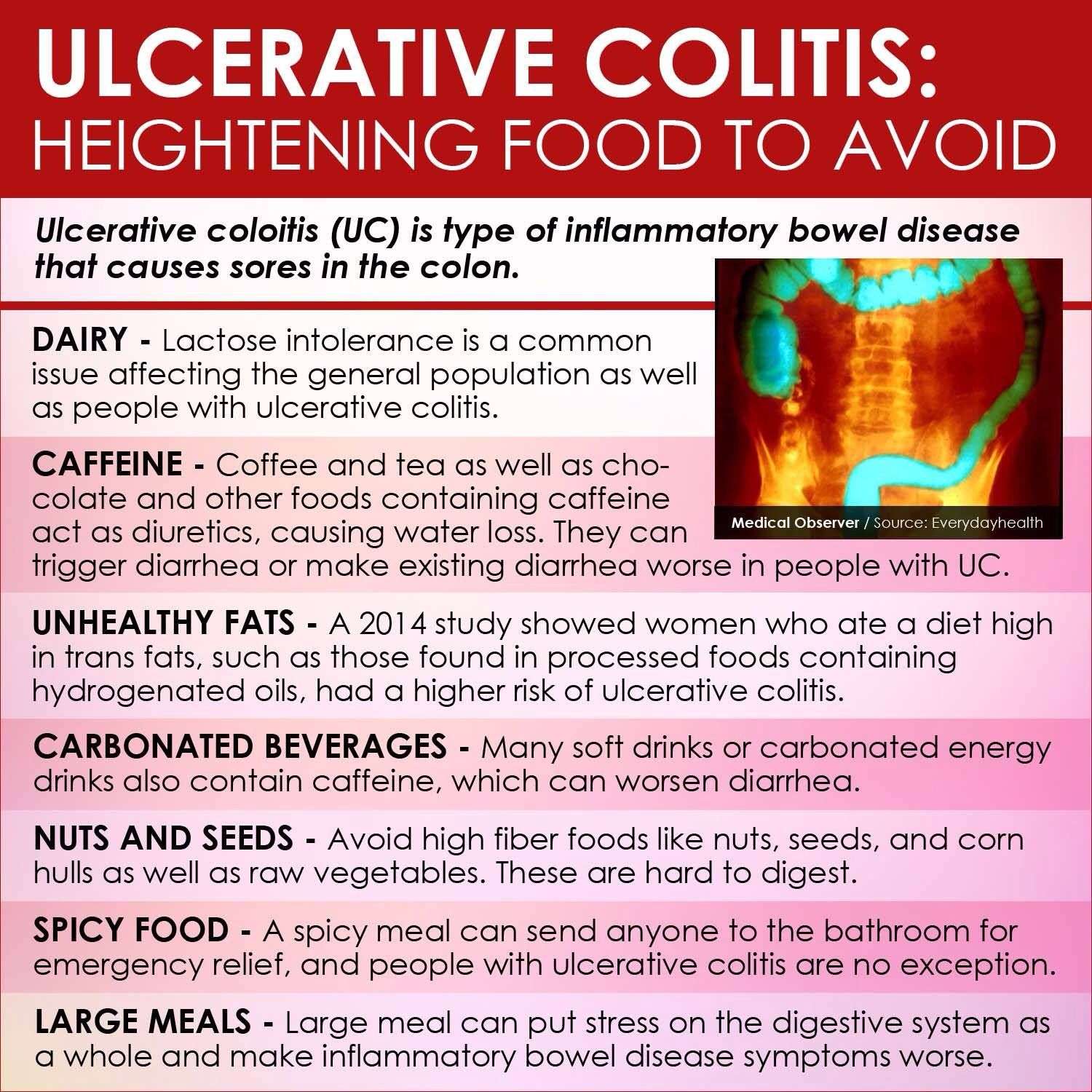
Foods To Avoid With Ulcerative Colitis
- Added sugars and hyper-processed foods
Our North American love affair with low fibre, high sugar and high fat hyper-processed food is associated with our risk of ulcerative colitis. It is this type of eating that is thought to drive gut dysbiosis or the overgrowth of more pro-inflammatory gut bacteria that can harm gut barrier integrity leading to leaky gut and inflammation. In laboratory studies, this type of diet can decrease the number or acetate and butyrate producing bacteria and increase the risk of colitis.
Another issue with hyper-processed foods is that they contain emulsifiers like xanthan gum and carrageenan which may alter gut barrier integrity. While their true impact on gut health is still hotly debated, in one double-blinded trial, people with ulcerative colitis on a carrageenan free diet had lower relapse rates than those given two capsules of carrageenan. For me, this would not be the first place I look when adjusting someones diet instead, it would be a refinement only after taking more global steps towards a more whole foods, plant-based approach.
- Meat, particularly red meat
If you arent a huge fan of red meat, ditch it entirely. If you truly love red meat, try to limit yourself to one 3-4 ounce portion every week or two, no more.
Dairy could be impacting symptoms for a few reasons:
- Omega 6-rich cooking oils like soy, corn and safflower oils
Can Surgery Affect Nutritional Status
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Don’t Miss: Do Enemas Help Ulcerative Colitis
Would You Like More Information On How To Start A Low Fodmap Diet For Ulcerative Colitis
Tap the blue button below to download our Eat This, Not That list as well as additional resources for IBS and colitis
SEND ME THE LIST
About Kimberly Yawitz
Kim Yawitz is a registered dietitian and nutritionist in St. Louis, Missouri.
She currently works with sports nutrition and weight management clients for a private practice. Prior to that Kim worked as an inpatient clinical dietitian, developing nutrition care plans for patients with health concerns ranging from autoimmune disease to critical illness.
Learn more about her on the About page.
Joe Leech, Dietitian
Recent Posts
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Read Also: Ulcerative Colitis And Inflammatory Bowel Disease
What Is Ulcerative Colitis
Ulcerative colitis is a chronic type of inflammatory bowel disease , like Crohns disease and microscopic colitis that affects the colon .
Recent studies estimate that IBD affects 2 million people worldwide .
Ulcerative colitis causes inflammation and sores in the inner lining of the colon. Inflammation often begins in the rectum, but it can spread throughout the large intestine.
Summary: Ulcerative colitis is a type of inflammatory bowel disease that causes inflammation and sores in the colon.
Bottom Line: Is The Carnivore Diet Good For Ulcerative Colitis
There is no cure for UC so when we read social media posts or headlines that try to say the opposite, we must be wary. It has been well established that fiber from carbohydrates and plant foods are health promoting, particularly for Ulcerative Colitis and the IBD community. For more on what to eat for IBD, we have plenty of free resources and blog posts.
If you are confused about what to eat and are ready for a higher level of support from a specialist, schedule a free discovery call to explore ways we can help you. We have many different levels and ways to support your IBD journey!
Dont Miss: How To Get Rid Of Ulcers In My Mouth
Also Check: Ulcerative Colitis And Yeast Infection
Do Any Medications Have Nutritional Side Effects
Moderate to severe flares of IBD are often treated with corticosteroids , cholestyramine and 5-ASA compounds . These medications have nutritional side effects that should be addressed. If you use any of these medications, talk to your doctor or registered dietitian for treatment advice.
- Prednisone causes decreased absorption of calcium and phosphorus from the small intestine. It also causes increased losses of calcium, zinc, potassium and vitamin C. With continual use of high doses of prednisone, the result may be bone loss and development of bone disease. People on prednisone may need up to 1200 milligrams a day. Protein needs also are increased for people taking prednisone because it increases protein breakdown in the body.
- Cholestyramine decreases absorption of fat-soluble vitamins , as well as folate, vitamin B-12, calcium and iron.
- Sulfasalazine interferes with folate absorption. People taking this drug also should take a 1 milligram folate supplement each day.
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Don’t Miss: Causes Of Ulcers In Horses
What To Eat During Remission
Increase fiber and reintroduce whole grains — Slowly incorporate foods higher in fiber when gastrointestinal symptoms lessen.
Consume omega-3 fatty acids — Consider eating more fresh or canned fatty fish or taking a fish or flaxseed oil supplement.
Focus on wholesome foods in their natural state — This includes foods with minimal processing and minimum ingredients.
Dairy and lactose products will be better tolerated — If you have a lactose intolerance, avoid dairy or eat low-lactose or lactose-free products.
Added fats will be better tolerated — Continue to focus on using oils, such as olive oil or canola oil, instead of solid fats.
Continue to focus on protein foods — Consume beef, eggs, poultry and other lean meats or plant-based proteins, such as soy products.
Be sure to drink plenty of water — Drink water instead of fruit juices, soft drinks, alcohol and caffeinated beverages such as coffee or tea.
Ulcerative Colitis Diet: Food Preparation And Meal Planning

While the idea of an elimination diet or restricting your intake of fiber, fat or other trigger foods may seem daunting, meal planning and preparing your food ahead of time can take some of the stress out of eating in a flare up. If your appetite is impacted as well, you can batch cook and eat what you want of a larger pre-prepared meal when you feel like eating, rather than preparing yourself a whole new meal from scratch.
The Crohns and Colitis Foundation indicates that rates of depression and anxiety are higher in those with IBD, so anything that can reduce stress for those with ulcerative colitis might be helpful for managing mental health. As such, pre-planned meals based around particular dietary needs can make the day-to-day experience of ulcerative colitis slightly less stressful, and may make the experience of a flare up more bearable.
This article is for informational purposes only and is not meant to offer medical advice.
Read Also: How To Cure Ulcer Naturally At Home In Tamil
Don’t Miss: What Is Ulcerative Colitis And How Is It Treated
How Does Diet Affect Ulcerative Colitis
Lifestyle factors that include consuming red meat and alcohol and overeating protein and sulfur-rich foods can increase the risk of a flare-up of ulcerative colitis. This can worsen the condition and cause unpleasant symptoms.
How do you cope with ulcerative colitis?
Managing flare-ups
What bread is best for ulcerative colitis?
Potato or sourdough bread is usually easier to tolerate for people with ulcerative colitis. Top with scrambled eggs for a good source of protein.
How A Professional Can Help
Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
Recommended Reading: Things To Eat With Stomach Ulcer
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Read Also: Can Stomach Ulcers Cause Heartburn
Ulcerative Colitis: An Inflammatory Bowel Disease
Clinically reviewed by Jenilee Matz, MPHFeb 09, 2021 7 min
What is ulcerative colitis? Ulcerative colitis is a type of inflammatory bowel disease.
It causes inflammation and sores, called ulcers, to develop on the inner lining of the large intestine . The inflammation and ulcerations lead to unpleasant symptoms, such as abdominal discomfort and diarrhea. While this chronic, lifelong condition has no known cure, treatment can usually keep the symptoms well-controlled.
Ulcerative Colitis Diet: What To Eat In A Flare Up
A low residue diet is often recommended to manage symptoms of ulcerative colitis. The Canadian Society of Intestinal Research outlines residue as the solid contents that stay in the bowel after digestion, with the goal of reducing the number of bowel movements that happen in a day. Residue includes fiber, which is limited to 10-15g per day, but the low residue diet differs from the low fiber diet by including foods that may stimulate frequent bowel movement, such as dairy, caffeine, alcohol and gristly or fatty meat.
Dr Deborah Lee, of Dr Fox Online Pharmacy, recommends the following foods for a low residue diet:
- Low fiber fruit and veg such as melon and bananas, as well as stewed fruit
- Lean protein such as white meat, eggs and tofu
- Refined grains such as white bread, white pasta and oatmeal
- Cooked seedless and skinless vegetables such as cucumber, potato and squash.
Cooking your food may also break down some of the dietary fiber to make it more digestible, as seen in a study in the journal of Plant Foods for Human Nutrition , which indicates that the process of cooking decreases the amount of insoluble dietary fiber in some vegetables.
- Related: 4 dairy free diet benefits
Read Also: Humira Not Working For Ulcerative Colitis
Nutrition Recommendations During Remission
- Aim to eat balanced meals and snacks with a combination of protein, fat, and complex carbohydrates. Check out the plate method in the updated 2019 Canadas Food Guide to see what this could look like.
- Choose a variety of healthy and whole foods and limit the intake of ultra-processed foods, artificial sweeteners, and trans fats.
- Do not limit your intake of foods high in fibre unless they trigger symptoms for you and/or if you have stricturing Crohns disease. Most people have no trouble digesting fibre while in remission, while some people may still find certain foods high in insoluble fibre, such as raw vegetables and kale, hard to digest. Fibre is incredibly important for promoting mucosal healing, stimulating sodium and water intake in the colon, and the growth of beneficial bacteria.
- Take vitamin D3 supplements . Vitamin D3 has anti-inflammatory properties and having low levels of vitamin D might increase your risk of a flare.
- Avoid low carbohydrate diets, such as the specific carbohydrate diet, with the goal of preventing relapse, as they are not effective and major healthcare societies do not recommend them. They can be very restrictive and lead to nutrient deficiencies.
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Recommended Reading: What Is Peptic Ulcer Pain Like
More Information About Ulcerative Colitis
According to George Washington University, colitis is a chronic digestive disease characterized by inflammation of the inner lining of the colon. Infection, loss of blood supply in the colon, Inflammatory Bowel Disease and invasion of the colon wall with collagen or lymphocytic white blood cells are all possible causes of an inflamed colon.
The following diseases fall into the colitis/IBD category they all can be treated with a combination of medication and improvements to your eating habits: