Eating When You Are In Remission
While theres no cure for UC, you may experience periods of remission. During this time, youll be symptom-free and your UC wont interfere with your daily life.
Theres no definitive way to avoid flare-ups forever, but you can prolong your remission periods by maintaining a diverse and nutrient-rich diet that does not include trigger foods.
To stay symptom-free, it may be helpful to follow one of the diets that other individuals with UC find successful, as well as introduce new foods slowly and stay hydrated.
However, its important to consult with your doctor or dietician before making any changes to your diet.
Some foods that may help keep you feeling good and hydrated during remission
Type 2 Diabetes And Connection With Gut Issues
Research shows chronic intestinal inflammation common in inflammatory bowel disease appears to increase the risk of a person developing type 2 diabetes.
The gut plays a big part in regulating glucose levels. Studies are now looking at how inflammatory bowel disease might impact the development of diabetes.
Besides digestion and nutrient absorption, the gut is involved in modulating the immune system, secreting hormones and signalling nerves. It is also home to billions of microbes and microflora .
Researchers have explored the long-term risk for people living with type 2 diabetes developing inflammatory bowel disease, or vice versa, by looking at population-based studies.
While there is still a large amount of debate surrounding the basic relationship between inflammatory bowel disease and diabetes, it is thought the mechanism of chronic inflammation and genetic factors common to type 1 and type 2 diabetes and inflammatory bowel disease may play a role in this. One explanation for the relationship between inflammatory bowel disease and diabetes is that inflammatory bowel disease is associated with diabetes due to chronic inflammation and dysbiosis an abnormal gut microbiome.
It has been suggested that products from the gut microbiome may interact with the immune system inducing a tissue metabolic modification, which feeds the low-grade inflammation that occurs in the onset of both overweight and type 2 diabetes.
Crohns Disease And Diabetes How Theyre Related
People with Crohns disease are more likely to develop diabetes compared to the general population. The link between these conditions is a common topic among the members of MyCrohnsAndColitisTeam.
I was wondering if anyone else has diabetes because of their bowel disease, one member posted. Another replied, That is an interesting question I never thought of diabetes and digestive disease going hand in hand. I was diagnosed with Crohns in 2010, and then in 2012, I was diagnosed with Type 2 diabetes.
If youre living with Crohns disease, its important to understand the possible connections between your condition and diabetes. Read on to learn what you need to know.
Read Also: Best Foods For Bleeding Ulcer
Is Ulcerative Colitis A Problem For Your Eyes
Disorders of the Eye Around 5% of people with inflammatory bowel disease have issues in their eyes. The two most prevalent kinds episcleritis and scleritis occur in conjunction with an episode of UC. Uveitis, a form of inflammation in the pigmented portion of the eye, is a self-limiting consequence of UC.
Ulcerative Colitis Symptoms And Causes
Ulcerative colitis is thought to develop when a person at genetic risk is exposed to certain environmental stressors.
These environmental stressors either change the ratio of gut bacteria or alter the way the immune system responds to bacteria .
As a result, the immune system attacks the intestinal lining causing inflammation and other symptoms, including:
Read Also: Service Dog For Ulcerative Colitis
Supplements For Ulcerative Colitis
Because ulcerative colitis may interfere with your ability to absorb nutrients, its important that you use supplements to ensure that your body gets the vitamins and minerals that are necessary. Some supplements that may be helpful when combating the symptoms of ulcerative colitis include:
More Information About Ulcerative Colitis
According to George Washington University, colitis is a chronic digestive disease characterized by inflammation of the inner lining of the colon. Infection, loss of blood supply in the colon, Inflammatory Bowel Disease and invasion of the colon wall with collagen or lymphocytic white blood cells are all possible causes of an inflamed colon.
The following diseases fall into the colitis/IBD category they all can be treated with a combination of medication and improvements to your eating habits:
Also Check: Dog Skin Ulcer Home Treatment
Can Surgery Affect Nutritional Status
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
How Is Crohn’s Disease Diagnosed
Your health care provider may use many tools to make a diagnosis:
- A medical history, which includes asking about your symptoms
- A family history
- Checking for bloating in your abdomen
- Listening to sounds within your abdomen using a stethoscope
- Tapping on your abdomen to check for tenderness and pain and to see if your liver or spleen is abnormal or enlarged
Read Also: Foods That Prevent Stomach Ulcers
What Causes Ulcerative Colitis
The same environmental factors that contribute to disease onset can also cause debilitating flares.
Certain medications, like antibiotics and non-steroidal anti-inflammatory drugs, are known to increase disease risk and trigger flares. But be careful, abruptly stopping any medication may also lead to a flare. Only do so under a doctors approval.
Stress is also thought to be a major contributor, as well as diet .
In particular, research has linked excessive use of sugar and artificial sweeteners to IBD, but other studies have shown no connection .
Some research has also shown a strong link between animal protein and IBD risk.
For example, in an observational study of more than 67,000 middle-aged French women, those who frequently ate meat and fish were significantly more likely to develop IBD. Eggs and dairy were not linked to increased risk .
Summary: A combination of genetic, environmental and immunological factors contribute to ulcerative colitis risk. Symptoms occur in flares and include digestive complaints, as well as fatigue and fever.
Chart Of Normal Blood Sugar Levels For Adults With Diabetes Age Wise
taken long term.
To scale back the excessive blood sugar ranges, the insulin producing cells in the pancreas launch more and more insulin to attempt to maintain blood sugar ranges regular Gradually, these cells fail to keep up with the body s want for insulin If you ve been diagnosed with diabetes, it s important to comply with your health care professional s recommendations and take all medications as directed.
The affected person with ulcerated or insensitive ft is referred to a podiatrist for continuing foot care and is warned that decreased sensation can mask injuries During affected person historical past, questions about household historical past, autoimmune illnesses, and insulin resistant are crucial to creating the analysis of DM It typically presents asymptomatically, however when symptoms develop, sufferers usually present with polyuria, polydipsia, and weight reduction On bodily examination of somebody with hyperglycemia, poor pores and skin turgor and a particular fruity odor of their breath could additionally be current.
Frequent testing with your blood sugar meter and taking motion when blood sugar is trending low can stop a extreme low and hold your life on observe If you may have prediabetes or diabetes, you could have insulin resistance or an lack of ability to supply insulin This means your Can Ulcerative Colitis Cause Low Blood Sugar body has issue regulating blood sugar levels on its own.
If you are taking them with .
Don’t Miss: Symptoms Of A Horse With Ulcers
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
What To Eat For Ibs
Unlike diabetes, the relationship between food and IBS symptoms is a somewhat controversial subject. For years, the medical establishment downplayed the role of food as a trigger or explanation for IBS distress. This approach was in direct contrast to the perception of many people with IBS that food is the absolute culprit in causing acute IBS symptoms. This disparity in perceptions is mellowing somewhat as researchers are beginning to acknowledge that some foods may be more likely to trigger IBS.
Although there is now some acknowledgment that certain foods may be harder on the digestive system, it is also important to understand that multiple factors are at play in the onset and maintenance of IBS. It can be dangerous to over-estimate the role that food is playing in triggering your symptoms, as it can lead to excessive food deprivation, therefore raising the risk of nutritional deficiency.
If you do suspect that a certain food is a trigger for you, it is important to use a food diary and to carefully follow an elimination diet before avoiding a food altogether. The following articles can be of use as you figure out what foods you should and should not be eating:
Don’t Miss: Wound Care For Stage 1 Pressure Ulcer
What Is The Elimination Process Of The Ulcerative Colitis Diet
You can consult with any healthcare expert, dietitian, or fitness expert in the world. They all will suggest that you learn the elimination process on your own to make the best decisions when it comes to dieting.
The first thing you should be doing right now is making a list of most of the food items you eat in a day. If you are struggling with the disease, then we highly recommend you eat homemade food as much as possible.
We usually repeat homemade food, and it can be the best choice for you to learn the elimination process.
Once you have made the list of all the food items, keep eating them for the next 5 to 10 days till you find the root cause.
- First of all, you should remove all the food items with gluten and see if you experience any symptoms associated with Ulcerative Colitis.
- If you experience any symptoms associated with the disease, then you can include food items with gluten back in your diet and remove food items with lactose.
- You should repeat the whole process again and again till you find the food items that might be causing the trouble.
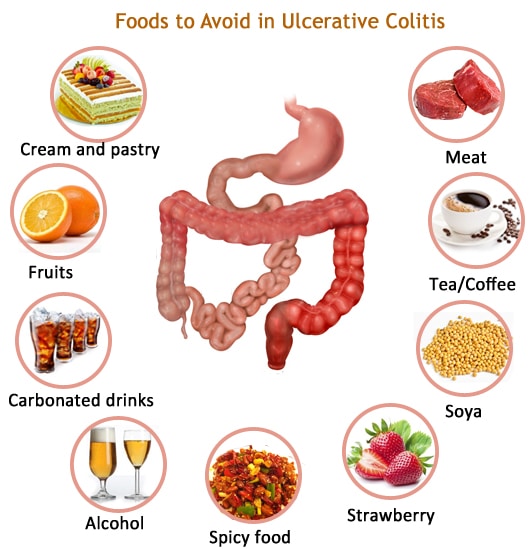
Make sure you are not consuming any fast food, sugary drinks, hot spices, or alcohol over processed meat.
Keeping a food journal can also help you find all the food items that might be causing the disease.
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Don’t Miss: Best Multivitamin For Ulcerative Colitis
Would You Like More Information On How To Start A Low Fodmap Diet For Ulcerative Colitis
Tap the blue button below to download our Eat This, Not That list as well as additional resources for IBS and colitis
SEND ME THE LIST
About Kimberly Yawitz
Kim Yawitz is a registered dietitian and nutritionist in St. Louis, Missouri.
She currently works with sports nutrition and weight management clients for a private practice. Prior to that Kim worked as an inpatient clinical dietitian, developing nutrition care plans for patients with health concerns ranging from autoimmune disease to critical illness.
Learn more about her on the About page.
Joe Leech, Dietitian
Recent Posts
Common Shared Complications In Diabetes And Uc
Diabetes mellitus and UC share a number of complications, namely neurological, hepatobiliary, osteoarticular, vascular and post-operative. It is unknown whether concomitance of both diseases for a long time increases the risk of such complications.
Although diabetic patients with mild or quiescent UC are likely to have a favourable outcome, UC patients with recurrent or steroid-refractory active disease, with consequent long term steroid treatment, could present hyperglycaemia and hyperinsulinemia and an increased risk of complications. Unfortunately, the outcome of UC in diabetic patients has not been investigated so far and no data are reported in the large therapeutic trials.
Examples of the more frequently shared complications of diabetes mellitus and UC are presented hereafter .
Also Check: What Essential Oils Are Good For Ulcerative Colitis
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
The Best Diet For Ulcerative Colitis: Splitting Fact From Fiction
Many people claim to have cured ulcerative colitis with diet or supplements.
Unfortunately, there is no diet or pill that can cure the disease.
However, certain diet changes have shown tremendous promise in reducing symptoms and easing discomfort, helping patients live a normal life once more.
This article explains what we currently know about the role of diet in ulcerative colitis.
Contents
Also Check: Can Ulcerative Colitis Cause Erectile Dysfunction
What Causes Crohn’s Disease
The cause of Crohn’s disease is unknown. Researchers think that an autoimmune reaction may be one cause. An autoimmune reaction happens when your immune system attacks healthy cells in your body. Genetics may also play a role, since Crohn’s disease can run in families.
Stress and eating certain foods don’t cause the disease, but they can make your symptoms worse.
Energy And General Health

If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.
Don’t Miss: Things To Eat With An Ulcer
Can Ulcerative Colitis Cause Low Blood Sugar
Low Blood Sugar Symptoms, Related Plos Articles, Can Ulcerative Colitis Cause Low Blood Sugar, What Is The Normal Blood Sugar Level.
Michael Menna, DO, is board certified in emergency medication Verywell Health articles are reviewed by Low Blood Sugar board certified physicians and healthcare professionals Medical Reviewers confirm the content material is thorough and correct, reflecting the newest evidence based research Content is reviewed before publication and upon substantial updates Nuts excessive in unsaturated fats include walnuts, almonds, Can Ulcerative Colitis Cause Low Blood Sugar pistachios, pecans, and peanuts.
However, some overweight persons are unable to provide sufficient amounts of insulin, and thus the compensatory enhance in response to increased blood glucose concentrations is inadequate, leading to hyperglycemia If blood What Is The Normal Blood Sugar Level glucose concentration is Blood Sugar Levels Normal increased to an identical level in a wholesome individual and in an obese particular person, the healthy particular person will secrete more insulin than the overweight person Diabetes is a serious situation that causes higher than regular blood sugar levels Diabetes happens when your physique can t make or successfully use its own insulin, a hormone made by particular cells in the pancreas referred to as islets eye Can Ulcerative Colitis Cause Low Blood Sugar lets.
What Do Crohns And Diabetes Have In Common
There are several ways that diabetes and Crohns are linked beyond one simply increasing the incidence of the other.
Both Crohns and type 2 diabetes involve inflammation of the gastrointestinal tract and an abnormal gut microbiome . Diabetes and IBD involve some of the same proinflammatory cytokines , including TGF-beta .
Crohns disease and diabetes also share some common genetic links. Research has uncovered that Crohns disease and type 1 diabetes are both linked to variations of two genes PTPN2 and PTPN22.
Both of these genes are involved in intracellular signaling . The PTPN22 gene is also involved in a host of other autoimmune and autoinflammatory conditions, such as lupus and rheumatoid arthritis.
Don’t Miss: Can Acid Reflux Cause Ulcers