Bone And Joint Infection
Infection can also spread from a pressure ulcer into underlying joints and bones .
Both of these infections can damage the cartilage, tissue and bone. They may also affect the joints and limbs.
Antibiotics are required to treat bone and joint infections. In the most serious of cases, infected bones and joints may need to be surgically removed.
Other Tips For Preventing Pressure Ulcer
1. Check the skin daily for any signs or symptoms of pressure ulcers. The patients can take the help of Bedside Wound Care Services for this. 2. Maintain a healthy and balanced diet that contains sufficient and enough protein with good sources of vitamins and minerals.3. Quit smoking. People who smoke are more prone to develop pressure ulcers due to the damage caused to blood circulation. 4. For repositioning, wheelchair push-ups are good where the person can raise their body off the seat by pushing on the arms of the chair. The use of cushions or special mattresses is also prescribed to release pressure and ensure a well-positioned body. Avoid doughnut cushions as they can put pressure on surrounding tissues.5. Ensure regular pressure ulcer dressings to avoid any type of infection and effective wound healing.
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
Recommended Reading: How Do They Check For Ulcers
Diet And Lifestyle Changes To Avoid Pressure Sores
Changes to avoid pressure sores include:
- Make sure you eat a healthy and nutritious diet. This includes a balanced diet and fluids/water. And if necessary,youre your doctor about vitamin and nutritional supplements .
- Low body weight or being overweight can cause pressure sores, so make sure you maintain heathy body weight
- If youre malnourished or at risk of malnutrition, protein, fluid and energy intake should be increased.
- Be aware of using good hygiene practices.
- Maintain activity levels, where appropriate.
- Make sure you quit smoking.
Peptic Ulcer Disease Symptoms Signs
Peptic Ulcer Disease Symptoms Signs. For the diagnosis, it is important to have information about the. Stomach pain alone may not be peptic ulcer disease. The most common symptom is a burning sensation or pain in the middle of your abdomen between your chest and belly button. The primary symptom of peptic ulcer is upper abdominal pain.
Less often, ulcers can cause serious signs and symptoms, including: Many people with peptic ulcers particularly complain of pain on an empty stomach. Pain radiating to the back burning or gnawing feeling similar to hunger pains
The primary symptom of peptic ulcer is upper abdominal pain. The most common symptom is a burning sensation or pain in the middle of your abdomen between your chest and belly button. Symptoms of peptic ulcer disease may be similar to other upper gastrointestinal conditions.
Beyond feeling nausea, some patients vomit as well, especially vomit that is bloody or resembles coffee grounds due to the peptic ulcer, so keep a watch out for these signs too. An aching in the middle of the night when the stomach is empty Bloating burping feeling sick to your stomach poor appetite vomiting weight loss
Ad reveal why these stomach ulcer signs are so important to know right now. Bloating, heartburn, nausea, pain, & more. Stomach pain alone may not be peptic ulcer disease.
Also Check: Is Ulcerative Colitis An Infection
Also Check: Vsl 3 And Ulcerative Colitis
Enhancing Healthcare Team Outcomes
The main goal is to prevent a decubitus ulcer by decreasing the pressure acting on the affected site. This goal requires an interprofessional team, including primary care providers, wound care specialists, surgeons, specialty-trained wound nurses, physical therapists, and nurses aides. Nurses provide care, monitor patients, and notify the team of issues. Nurses aides are often responsible for turning and repositioning patients. Air-fluidized or foam mattresses should be used, frequent postural changes, provision of adequate nutrition, and treatment of any underlying systemic illnesses. Debridement should take place to remove dead tissue that serves as the optimum medium for the growth of bacteria. Hydrogels or hydrocolloid dressing should be used, which aid in wound healing. Tissue cultures are necessary, so the most directed antibiotic can be administered, which can involve the pharmacist and the latest antibiogram data. The patient should be kept pain-free by giving analgesics. They should try to increase physical activity if possible, which a nurse’s aide, medical assistant, or rehab nurse can facilitate. Frequent follow-ups are an absolute necessity and a team approach to patient education and management involving the wound care nurse and wound care clinician will lead to the best results. These interprofessional activities can help drive better outcomes for patients with decubitus ulcers.
Who Is At Risk Of A Pressure Ulcer
People immobile due to illness or injury are at greatest risk of getting a pressure ulcer.
- They may be unable to change position without assistance eg, see Skin complications of paraplegia and tetraplegia.
- They may have nerve damage from injury or illness, such as spina bifida, diabetes or stroke, and are unable to sense pain or the signals that normally make people move.
- Older people are at greater risk because their skin is thinner and more fragile.
- A pressure ulcer may develop underneath a plaster of Paris or fibreglass plaster .
Recommended Reading: Foods You Can Eat With An Ulcer
Types Of Ulcerative Colitis
UC can be categorized according to the parts of the GI tract that it affects.
- Ulcerative proctitis. In ulcerative proctitis, only the rectum is inflamed. Its considered a mild form of UC.
- Left-sided colitis. Left-sided colitis causes inflammation in the area between the splenic flexure and the last section of the colon. The last section of the colon, known as the distal colon, includes the descending colon and sigmoid colon. Left-sided colitis is also known as distal ulcerative colitis.
- Proctosigmoiditis. Proctosigmoiditis is a form of left-sided colitis. It causes inflammation in the rectum and sigmoid colon.
Different tests can help a doctor diagnose UC. UC mimics other bowel diseases such as Crohns disease. A doctor will order multiple tests to rule out other conditions.
Tests to diagnose UC often include:
How Are Pressure Ulcers Diagnosed
The doctors will diagnose your ulcer by noting a few things about it like:1. The depth and size of your ulcer2. The skin colour that is a result of the sore3. Which tissue has been affected by the pressure ulcer4. The amount of skin damage and tissue death caused by the ulcer5. The present condition of the sore – whether it’s bleeding, has foul odour or is infected.
Treatment For Pressure Ulcers:
The treatment of the pressure ulcer depends on its stage it can require a surgery or medication or therapy. The treatment could include antibacterial medications if the ulcer is too infected as well as drugs can be given to the patient to relieve their discomfort.
Doctors can use a process called “debridement” to remove the dead tissues from the wound. It is very important to make sure that the wound remains away from dirt and dust it is very crucial for the wound to heal properly.
Changing the dressing of the ulcer wound regularly might be done by your doctor to maintain the hygiene and prevent any kind of infection.
You May Like: How To Get Remission In Ulcerative Colitis
When To Approach Wound Care Surgeons
If there are any signs of bedsores, the patients are recommended to change their positions to relieve the pressure on the area. If there is no improvement in the next 24 to 48 hours, contact Wound Care Surgeons.
Seek medical help if there is:
1. Any type of infection , such as fever , drainage from wounds , a sore that smells bad , or an increased redness or warmth as well as swelling around the pressure ulcer 2. Cold skin 4. Severe pain 5. High temperature etc.
In these above-mentioned conditions, seeking medical help from professional wound care services is necessary. These symptoms could be a sign of a severe infection that needs to be cured immediately.
How Do Nonsteroidal Anti
NSAIDS are a type of medication used often for headaches, period pains, and other pains. They can also help reduce fever and inflammation. Examples include aspirin and ibuprofen. Many NSAIDs are available without a prescription.
They lower the stomachs ability to make a protective layer of mucus. This it more susceptible to damage by stomach acid. NSAIDs can also affect the flow of blood to the stomach, reducing the bodys ability to repair cells.
You May Like: Can You Eat Pizza With Ulcerative Colitis
Early Warning Signs And Symptoms
Although a perforation may be the first indication of peptic ulcer disease, most people with this condition experience milder symptoms in the days or weeks leading up to the perforation. Pain between the breastbone and the navel may occur when the stomach is empty, and might be relieved with antacids. The pain may come and go, and is often worse at night. Dark, tarry bowel movements or vomiting material that resembles coffee grounds may signal bleeding from a peptic ulcer.
- Although a perforation may be the first indication of peptic ulcer disease, most people with this condition experience milder symptoms in the days or weeks leading up to the perforation.
- Pain between the breastbone and the navel may occur when the stomach is empty, and might be relieved with antacids.
Burning Pain In The Abdomen
Persistent burning pain in the abdomen is one of the first signs of a stomach ulcer. The sensation of pain occurs when juices in the stomach, which help in digestion, come into contact with an open sore in the stomach lining.
In most cases, the pain is felt from the breast bone to the navel, and it often worsens during the night. If you skip meals, particularly breakfast, you may also experience this burning sensation in the stomach during the daytime.
If the dull and burning ache of the ulcer often turns into a sharp, stabbing pain, it is a sign that your ulcer is acting up and you need medical help. It could mean that the ulcer has caused a more critical problem like a perforation in the wall of your stomach or intestine, or a blockage in your digestive tract, and it is triggering intense pain.
Read Also: What Is A Duodenal Ulcer And How Is It Caused
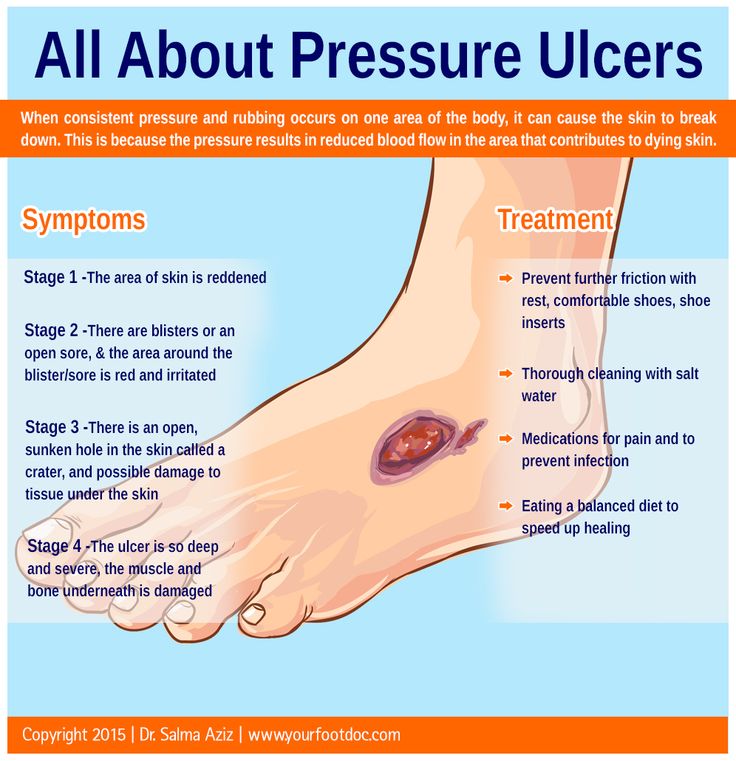
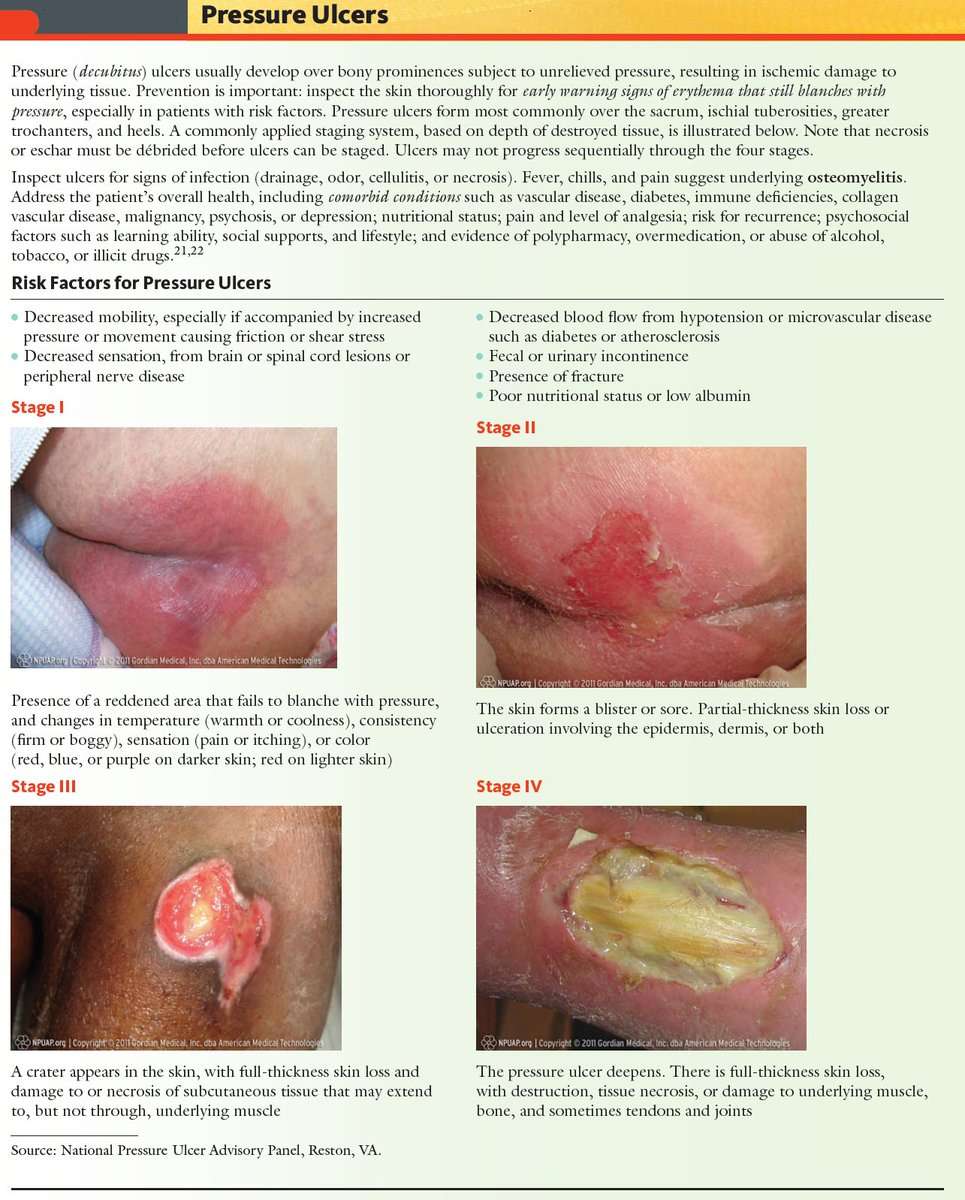
Grades Of Pressure Sores
If youve been bedridden for long enough, the areas of skin that are constantly in contact with the mattress or chair will start to discolour. This shows that the skin is in danger of ulcerating.
Pressure sores are graded to four levels, including:
- grade I skin discolouration, usually red, blue, purple or black
- grade II some skin loss or damage involving the top-most skin layers
- grade III necrosis or damage to the skin patch, limited to the skin layers
- grade IV necrosis or damage to the skin patch and underlying structures, such as tendon, joint or bone.
Treatment Of A Bleeding Peptic Ulcer
The initial treatment for a bleeding peptic ulcer is the same as a non-bleeding ulcer provided that the bleed is minor. Firstly the cause of the ulcers need to be removed. NSAIDs and other drugs that may be causing the peptic ulcers need to be discontinued or change to alternate medication that are less likely to affect the gut lining. Secondly peptic ulcer treatment needs to be initiated as soon as possible.
- Antibiotics to eradicate H.pylori bacteria.
- Antacids to neutralize stomach acid.
- Acid-suppressing medication to reduce stomach acid production.
- Ulcer-protecting drugs to assist ulcers to heal.
These measures should assist with the healing of the ulcer and the bleed may therefore cease. However, if there is a continuous minor bleed or massive blood loss from an ulcer then more invasive procedures are necessary. Endoscopic therapy where the site of the bleed is sealed is the first option. For acute bleeds, hemoclips may also be used during or after endotherapy to stop the bleed.
Read Also: Dog Skin Ulcer Home Treatment
What Causes Duodenal Ulcers
Your stomach makes a strong acid that helps you digest food and kills germs. The cells of the stomach and duodenum make a barrier from mucus, to protect themselves against this acid. If the mucus barrier is damaged, an ulcer can form.
The main cause of this damage is infection with bacteria called Helicobacter pylori, or H. pylori. The bacteria can cause the lining of your duodenum to become inflamed and an ulcer can form.
Some medications can also cause duodenal ulcers, particularly anti-inflammatory medicines such as ibuprofen and aspirin. It is rare that other medicines or medical conditions cause an ulcer.
There are some lifestyle factors that may make you more likely to get a duodenal ulcer, such as:
However, these things are less important than infection with H. pylori.
What Are The Risk Factors For Bedsores
Being bedridden, unconscious, unable to sense pain, or immobile increases the risk that a bedsore will develop. The risk increases if the person is not turned, positioned correctly, or provided with proper nutrition and skin care. People with diabetes, circulation problems and malnutrition are at higher risk.
Read Also: Bone Broth And Ulcerative Colitis
Evaluation Of Type Of Discharge And Pus
Amount and type of discharge and pus is noted. This is assessed along with signs of infection.
A swap is used to take a sample of the pus or exudate and this is placed on a glass slide. This is evaluated after staining with appropriate dyes and examining under the microscope for presence of microorganisms.
The samples of the exudate is also used for culture in the laboratory and assessment of sensitivity to various antibiotics that may be used in therapy.
Presence of a track of pus or fistula or sinus is noted. This is usually a recurrent and bothersome condition that is difficult to treat without surgery.
Treatment For Pressure Sores
There are a variety of treatments available to manage pressure sores and promote healing, depending on the severity of the pressure sore. These include:
- regular position changes
- special mattresses and beds that reduce pressure
- being aware of the importance of maintaining healthy diet and nutrition
- dressings to keep the sore moist and the surrounding skin dry. There is no advantage of one type of dressing over another.
- saline gauze dressing may be used if ointments or other dressings are unavailable.
- light packing of any empty skin spaces with dressings to help prevent infection
- regular cleaning with appropriate solutions, depending on the stage of the sore
- there is no advantage of one particular type of antiseptic or antibiotic treatment over another
- specific drugs and chemicals applied to the area, if an infection persists
- surgery to remove the damaged tissue that involves thorough debridement of the wound, the removal of underlying or exposed bone, and filling the empty space
- operations to close the wound, using skin grafts if necessary
- continuing supportive lifestyle habits such as eating a healthy and nutritious diet, as suggested by the nutritional staff.
Read Also: What Are Ulcers Caused From
How To Reduce Risks For Ulcer
The American Association of Equine Practitioners recommends the following management tips for ulcer-prone horses:
- Allow free-choice access to grass or hay
- Feed smaller, more frequent meals
Though some ulcers may spontaneously resolve on their own, most will need treatment in order to heal, especially when horses remain in performance or training. There are several different approaches to treating ulcers in horses, but the primary one is acid suppressive therapy.
The most commonly prescribed ulcer treatment is omeprazole, an FDA approved proton pump inhibiting drug that has been well studied. Other drugs may prescribed depending on the location and severity of your horses ulcers. Some of these treatments include histamine blockers, coating or binding agents, synthetic hormones, prokinetic agents, and antibiotics, and a combination of several therapies is used in some instances.
What Are The Symptoms Of Bedsores
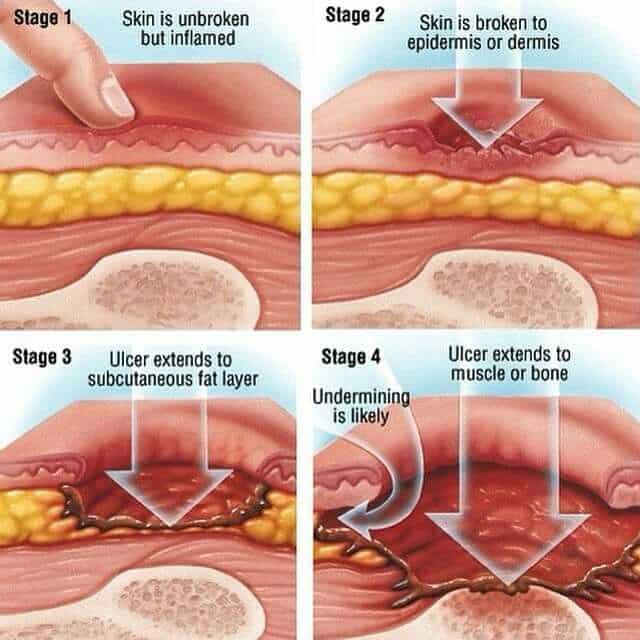
Bedsores are divided into 4 stages, from least severe to most severe. These are:
- Stage 1. The area looks red and feels warm to the touch. With darker skin, the area may have a blue or purple tint. The person may also complain that it burns, hurts, or itches.
- Stage 2. The area looks more damaged and may have an open sore, scrape, or blister. The person complains of significant pain and the skin around the wound may be discolored.
- Stage 3. The area has a crater-like appearance due to damage below the skin’s surface.
- Stage 4. The area is severely damaged and a large wound is present. Muscles, tendons, bones, and joints can be involved. Infection is a significant risk at this stage.
A wound is not assigned a stage when there is full-thickness tissue loss and the base of the ulcer is covered by slough or eschar is found in the wound bed. Slough may be tan, grey, green, brown, or yellow in color. Eschar is usually tan, brown or black.
You May Like: How Do You Treat A Bleeding Ulcer In The Stomach
Stages Of Pressure Ulcers And Treatment
Pressure ulcers can progress in four stages based on the level of tissue damage. These stages help doctors determine the best course of treatment for a speedy recovery.
If caught very early and treated properly, these sores can heal in a matter of days. If left untreated, severe bedsores may require years to heal.
When You Are In Bed
Use a foam mattress or one that is filled with gel or air. Place pads under your bottom to absorb wetness to help keep your skin dry.
Use a soft pillow or a piece of soft foam between parts of your body that press against each other or against your mattress.
When you are lying on your side, put a pillow or foam between your knees and ankles.
When you are lying on your back, put a pillow or foam:
- Under your heels. Or, place a pillow under your calves to lift up your heels, another way to relieve pressure on your heels.
- Under your tailbone area.
- Under your shoulders and shoulder blades.
- Under your elbows.
Other tips are:
- Do not put pillows under your knees. It puts pressure on your heels.
- Never drag yourself to change your position or get in or out of bed. Dragging causes skin breakdown. Get help if you need moving in bed or getting in or out of bed.
- If someone else moves you, they should lift you or use a draw sheet to move you.
- Change your position every 1 to 2 hours to keep the pressure off any one spot.
- Sheets and clothing should be dry and smooth, with no wrinkles.
- Remove any objects such as pins, pencils or pens, or coins from your bed.
- Do not raise the head of your bed to more than a 30 degree angle. Being flatter keeps your body from sliding down. Sliding may harm your skin.
- Check your skin often for any areas of skin breakdown.
Recommended Reading: How To Heal Venous Ulcers