Venous Leg Ulcer Treatment At Usa Vein Clinics
Our USA Vein Clinics specialists provide minimally invasive, office-based vein treatment at over 100 convenient locations nationwide. We also offer virtual doctor visits.
Most major health insurance plans cover treatment to resolve venous symptoms like varicose veins and venous ulcers. If you would like to discuss your coverage details or schedule an appointment, give us a call at .
Pain Management For Venous Ulcers
Venous ulcers are open skin sores that can affect any area of the body but most often occur on the legs. It is estimated that about 1% of Americans have venous ulcers. Theyre more common in older people, particularly women, and more likely to occur with people who have varicose veins. Other types of people who have an increased chance of getting a venous ulcer include:
- Those who have suffered previous leg injuries.
- Those who smoke.
- Those who are overweight or obese.
- Anyone with a circulation problem, such as blood clots or phlebitis .
Venous ulcers are sometimes called venous insufficiency ulcers, stasis leg ulcers, and venous leg ulcers.
In This Article:
What Are Venous Leg Ulcers
Venous leg ulcers, also known as venous stasis ulcers, are open, non-healing wounds that develop on the legs as a result of vein disease. Venous ulcers account for up to 80% of all leg ulcers. Cracked, dry, or reddened skin is often the first sign of a venous ulcer.
Common symptoms that often accompany venous leg ulcers include:
- Itchy, scaly, dry skin on the legs
- Hardened skin around the ulcer
- Heavy feeling in the legs
- Red, purple, or brown color on the skin
- Swollen and enlarged veins on the legs
- Cracked or dry skin that may open up
- Unpleasant and foul-smelling discharge from the ulcer
Unlike other types of wounds, venous leg ulcers do not heal on their own. However, treating underlying vein disease can promote their eventual healing, along with reducing your risk of developing additional leg ulcers and other venous issues.
Also Check: Common Symptoms Of Stomach Ulcer
How To Prevent Venous Leg Ulcers
Venous ulcers most often form around the ankles.
Venous ulcers typically occur because of damage to the valves inside the leg veins. These valves control the blood pressure inside the veins. They allow it to drop when you walk. If the blood pressure inside your leg veins doesnt fall as youre walking, the condition is called sustained venous hypertension. That increase in blood pressure causes ulcers to form on your ankles.
Venous ulcers may also be caused by other problems with your leg veins. These include:
-
Varicose veins. These are large, bulging leg veins. They occur when valves in the leg veins dont work well, allowing blood to collect in the lower leg.
-
Chronic venous insufficiency. Like varicose veins, this condition occurs when your leg veins cant pump blood back up to your heart. Blood then pools in your lower legs, causing your legs to swell. Since the blood cant flow well in your legs, the swelling may be extreme. This extreme swelling can put so much pressure on your skin that venous ulcers form.
Prevention Of Arterial Ulcers:
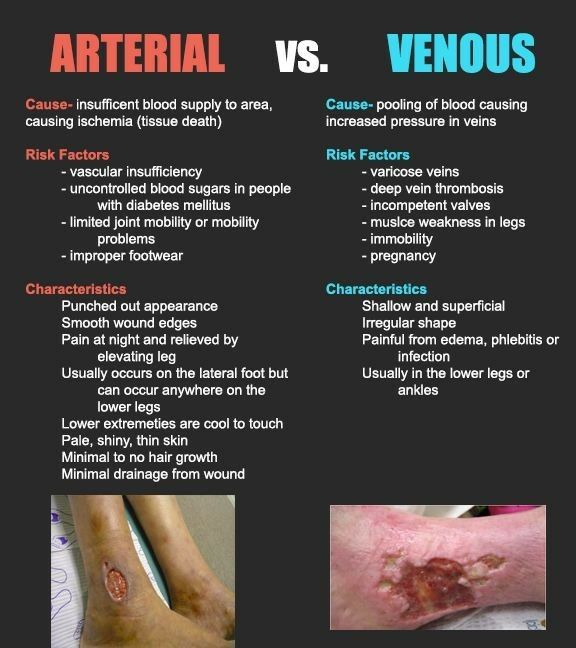
The lifestyle changes that the patient can adopt will contribute to improve peripheral circulation and help prevent arterial leg ulcers.
- Stop smoking: Smoking severely reduces the tissue perfusion and is one of aggravating factors for arterial leg ulcers.
- Healthy diet and weight loss: It Is important to reduce the intake of fat and to keep your cholesterol levels low. The patient should exercise as much as possible: this will help improve the blood circulation in your legs. If during exercising the patient feel some pain in his/her legs, it is normal. If the pain is more pronounced, or severe, it may be a sign that his/her arteries are seriously narrowed due to atherosclerosis. This needs to be addressed by a doctor.
- Take good care of patient’s feet: Advice shoes which fit correctly and are not too small Advice to keep feet warm avoiding feet and legs injuries Examinate feet and legs daily for any changes in color or developing sores Moisturizing the skin well to prevent skin damage which can develop ulcers.
You May Like: Signs Of An Ulcer In A Man
What Are Venous Ulcers
A venous skin ulcer is a sore on the leg that heals slowly, usually because of blood flow problems in the leg veins. When leg veins do not push blood back up to the heart as they should, the blood backs up , creating extra pressure in the veins. If the condition is not treated, the increased pressure and excess fluid in the affected area can cause an open sore to form.
Because of the continuous pressure, venous ulcers can linger anywhere from a few weeks to years and lead to more serious problems if untreated. Most venous ulcers occur on the lower leg, above the ankle.
Venous Leg Ulcers And Infection
The venous leg ulcer is the most common type of chronic leg wound, and it can be challenging to manage.1 VLUs account for up to 90% of all chronic leg ulcers.1 Proper diagnosis and treatment planning are key to wound healing outcomes. This fact is particularly true for older adults, who have an annual VLU prevalence of 1.7%.2
You May Like: What To Eat To Heal An Ulcer
Symptoms Of Venous Insufficiency Ulcers
Whe a venous ulcer begins to develop, stasis dermatitis may be present causing scaling and erythema of the lower extremities. Hemosiderin staining may also occur, causing the presence of brownish or yellow patches underneath the skin. Other skin changes may include the appearance of dark red or purple as a result of blood leaching into the surrounding tissue. Venous ulcers will present with shallow but large wounds with irregular margins that typically develop on the lower leg or ankle. The base of the ulcer is typically red, can result in a significant amount of exudate depending on the level of infection, and will ooze venous blood when manipulated. Typically the wound will be relatively painless, with any pain resulting from subsequent infection or edema. Often the entire leg will become swollen, and the skin will become more firm and reddish brown in color, otherwise known as stasis dermatitis. Elevation of the limb will help to relieve discomfort and swelling.
Figure 1: Venous ulcer with obesity as cofactorFigure 2: Large superficial venous ulcer
How To Help The Healing Process Along
To help the healing process along, follow these tips:
Do regular self-checks. Catching wounds early is the key to avoiding infections and complications. Make sure you do daily self-checks and look for new wounds, especially on your feet. Dont forget to check in between and under your toes.
Remove dead tissue. Necrosis and excess tissue often occur with diabetic wounds. This can promote bacteria and toxins and increase wound infection. It can also prevent you from being able to inspect the underlying tissue. Your doctor will often help you with the removal process.
Keep dressings fresh. Regularly changing dressings can help reduce bacteria and maintain appropriate moisture levels in the wound. Doctors often recommend special wound care dressings.
Keep pressure off the area. Pressure can cause wear and tear that damages the skin and leads to a deeper wound or ulcer.
If youre dealing with a foot wound, consider wearing white socks during the healing process. This will make it easier to see blood or other signs of drainage on your socks.
See your doctor if you experience any of the following:
Also Check: Are Eggs Bad For Ulcerative Colitis
Don’t Miss: What Happens When You Have A Stomach Ulcer
Faq: How Do You Treat Venous Leg Ulcers
Q. 1 What are the signs of venous leg ulcers?
Ans: There are many signs of venous leg ulcers. The most common symptom is pain and soreness around a vein in the lower leg. There may also be redness or swelling of the skin where the vein is located.
Other symptoms include heaviness or tiredness of the legs, especially after sitting for long periods of time or standing on your feet for an extended period of time feeling like you need to pop your ankles and move your foot up and down and having varicose veins that are visible on your skin.
Q. 2 How is a venous leg ulcer diagnosed?
Ans: Venous leg ulcers diagnosis doctors do by the following:
- A physical examination of the wound
- A blood test to measure the amount of oxygen in the blood
- An ultrasound scan to detect any abnormalities in the veins of the legs
- A duplex ultrasound scan to detect any abnormalities in the veins of the legs and examine for deep vein thrombosis
- Compression therapy of leg or limb, such as bandages and elastic stockings.
Q. 3 Is there a cure for venous leg ulcers?
Ans: There are many treatments for venous leg ulcers, and it is recommended to try them all before giving up. The most important thing is to keep the wound clean, dry and free from bacteria.
We should also avoid wearing any tight clothing or socks, which can put pressure on the wound and make it worse.
Q. 4 What do venous leg ulcers look like on a skin biopsy?
Q. 5 Are there any home remedies for treating venous leg ulcers?
Also Read This:
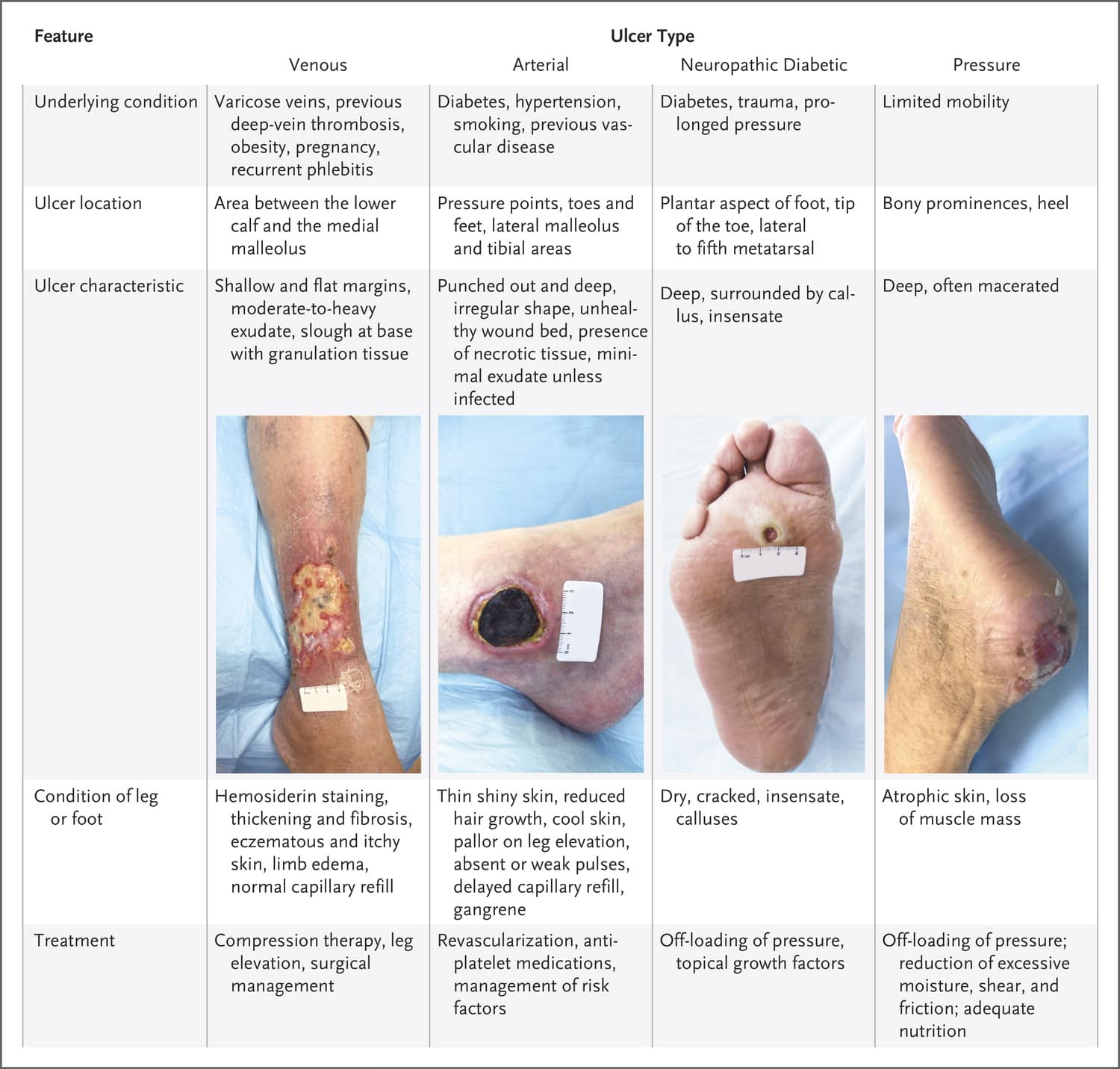
Venous And Arterial Leg Ulcers
A leg ulcer occurs when skin breaks down, usually on the lower leg area, just above the ankle.
The majority of leg ulcers are caused by venous disease , others can be of arterial or mixed origin. If not treated correctly, a leg ulcer can become a chronic wound which requires longer healing time, and they have a tendency to reoccur.
You May Like: How Do You Get Mouth Ulcers
How Are Stasis Ulcers Diagnosed
Stasis ulceration is usually a clinical diagnosis, made on the basis of the patientâs history and examination findings, and includes the presence of risk factors for venous stasis, that is, congestion and slowing of venous circulation, and the characteristic features of the wound and surrounding tissues.
- Duplex ultrasonography is used to confirm venous obstruction or valvular incompetence prior to saphenous vein ablation surgery
- Concomitant arterial disease is identified using the ankle-brachial index
Other investigations to evaluate venous insufficiency and provide haemodynamic information may include:
- Intravenous ultrasonography
- Haematological studies of the coagulation system.
Maintain A Healthy Weight
Having an elevated body mass index increases your likelihood of developing vein disease. Excess body weight strains tiny, one-way valves in your leg veins. Over time, this strain can cause veins to malfunction, leading to problems like varicose veins.
Weight loss and weight management are essential elements of venous ulcer prevention. Losing weight removes excess pressure on your veins, which can slow the progression of vein disease.
Recommended Reading: What To Take For Stomach Ulcers
How Can You Prevent Venous Ulcers
Improving your circulation and reducing pressure on your legs can help prevent venous ulcers. The following steps can help you avoid them:
- Improve your lifestyle by eating healthy foods and getting more sleep.
- Lose weight if you are overweight.
- Manage your blood pressure through stress management and/or medication.
- Raise your legs so that your feet are above your heart, several times a day.
- Wear compression stockings as often as your doctor recommends.
While most venous ulcers go away with time, some can cause serious complications, like infection. As always, prevention is the best medicine.
Controlling Pressure In The Leg Veins
Controlling swelling is essential for patients with venous leg ulcers. Leg elevation, with the feet at or above the level of the heart, several times throughout the day and while sleeping, can help reduce swelling. Compression wraps or bandages are often applied to the legs. These can be changed as often as multiple times a day or as infrequently as once a week, depending on the amount of fluid draining from the ulcer. Once the leg ulcer is smaller or nearly healed, elastic compression stockings may be recommended. Compression stockings are sized to fit the legs and are typically put on in the morning and worn throughout the day. A venous pump may be prescribed for patients with severe swelling.
Don’t Miss: Stomach Ulcer Foods To Eat
Is It Possible To Prevent Venous Ulcers
The first step in preventing venous ulcers is preventing vein problems. Healthy habits are essential to help maintain proper blood flow in the legs. There are various ways to help prevent venous ulcers through lifestyle changes, diet, and medication. The Lakeland vein clinic pain management doctors recommend:
- Quit smoking. Smoking is bad for blood vessels and contributes to blood clotting in the veins.
- Lose weight if youre overweight or obese.
- Maintain an ideal weight.
- Exercise as much as possible. Moving and staying active helps with blood flow. Check with your doctor about starting a walking program.
- Eat healthy foods and get plenty of sleep at night.
- Reduce the amount of salt in your diet.
- Control your blood cholesterol and triglyceride levels by making dietary changes and taking the medications your doctor prescribes.
- If you have diabetes, keep your blood sugar level under control to help you heal faster.
- Manage blood pressure and cholesterol levels.
- Talk to your doctor about taking aspirin to prevent blood clots.
- Avoid crossing legs while sitting.
- Avoid extreme temperatures.
- Avoid sitting or standing for extended periods of time.
- Avoid tight-fitting clothing and ensure that footwear is fitted correctly to avoid points of rubbing or pressure.
- Examine feet and legs daily for any unusual changes in color or the development of sores.
- Protect legs and feet from injury and infection.
- Raise your legs for a short time, especially if you stand for extended periods.
How Venous Leg Ulcers Are Treated
Most venous leg ulcers heal within 3 to 4 months if they’re treated by a healthcare professional trained in compression therapy for leg ulcers. However, some ulcers may take longer to heal, and a very small number never heal.
Treatment usually involves:
- cleaning and dressing the wound
- using compression, such as bandages or stockings, to improve the flow of blood in the legs
Antibiotics may also be used if the ulcer becomes infected, but they don’t help ulcers to heal.
However, unless the underlying cause of the ulcer is addressed, there’s a high risk of a venous leg ulcer recurring after treatment. Underlying causes could include immobility, obesity, previous DVT, or varicose veins.
Read Also: What Can I Eat With Ulcerative Colitis
Treating And Preventing Venous Ulcers
Venous ulcers are a rare complication of varicose veins and other chronic venous insufficiencies luckily, theyre relatively easy to prevent.
A venous ulcer is a shallow sore on the skin caused by an untreated venous insufficiency. These wounds most often develop on the lower legs and ankles, though they can occur anywhere. The most common symptoms include pain, inflammation, a sense of heaviness, and significant discoloration of the affected skin.
If left untreated, venous ulcers can emit an unpleasant odor and generate pus, causing patients significant distress and discomfort. Fortunately, they can be easily treated with some simple preventative measures. Well walk you through their most common cause and outline some measures you can take to treat and prevent them.
What Is The Best Treatment For Venous Ulcers
What is the recommended procedure for treating leg ulcers?
It depends on the cause. If the ulcers are due to varicose veins, then treatment of the varicosities can help significantly in conjunction with a wound care specialist. If due to deep venous reflux, compression stockings and wound care are the best choices.
It depends on the cause. If the ulcers are due to varicose veins, then treatment of the varicosities can help significantly in conjunction with a wound care specialist. If due to deep venous reflux, compression stockings and wound care are the best choices.
Correct any superficial venous reflux.
Correct any superficial venous reflux.
Venous stasis ulcers can be due to deep, superficial, and/ or perforatorvein incompetence deep vein thrombosis can also be involved in theetiology. Before recommending the best treatment, venous duplex scanning must be performed and acomprehensive history and physical must be taken by an expert in the field of complex venous disorders. Perforator vein surgery , superficial venous ablation, vein interruptions, or a combination of these treatments may be indicated.
The best treatment for venous ulcers consists of 2 parts, both applied assoon as possible. First, the underlying cause should be identified andtreated. Second, proper compression with edema reduction and specializedwound care is needed until the ulcer heals.
Donât Miss: Can You Donate Blood If You Have Ulcerative Colitis
Recommended Reading: Do Ulcers Make You Nauseous
Lead A Healthy Lifestyle
People who lead an unhealthy, sedentary lifestyle are far more likely to suffer from venous ulcers, as inactivity can impact circulation throughout your body, particularly your legs. As such, this can lead to blood pooling.
Also, weight gain is often associated with an unhealthy lifestyle, which puts more pressure on the veins in your legs. This can cause damage to the blood vessels, leading to issues like varicose veins and venous ulcers. By living a healthy lifestyle, you can prevent these issues from happening.
Progressive Resistance Exercise To Improve Calf Muscle Function

Majority of patients with venous ulcer disease have an impaired calf muscle pump. Poor calf muscle pump function in patients with chronic venous ulceration can be improved by physical exercise. There are evidences to support that enhancement of its ejecting ability with physical training results in improved hemodynamic parameters and promote ulcer healing. There are no RCTs or other forms of evidences that compared the recurrence rate of venous ulcers with and without progressive resistance exercise to prevent recurrence. One RCT compares 12 weeks progressive resistance exercise program in addition to compression with only compression. It was evident that significantly greater improvements in ejection fraction of the calf muscle in the exercise group. Isotonic exercises may also improve calf muscle’s ejecting ability and the global hemodynamic status in limbs with venous ulceration. Hence, it can be considered that limb exercise by its virtue of improving hemodynamic parameters of the affected limb is capable of preventing recurrences of venous leg ulcer.
Also Check: Low Fodmap Diet Ulcerative Colitis