Postoperative And Rehabilitation Care
Postoperative care of patients who have undergone reconstructive surgery is of utmost significance as these ulcers have high rates of recurrence. A study done on characteristics of recurrent pressure ulcers showed that patients who underwent reconstructive surgery and developed post-operative, had an 11% to 19% chance of recurrence. Those without any postoperative complications had recurrence as high as 61%.
When medical staff shift patients from the operating table to their air-fluid beds, they must avoid excessive shearing, and stretch on skin flaps. For the first four weeks, patients are positioned flat on their support surfaces, after which they can place themselves in a semi-sitting position. The patient starts to sit for 10 minutes only after six weeks of the surgical procedure. After these sitting periods, the flap should be examined for discoloration and wound edge separation. Over two weeks, the sitting periods will increase to 2 hours in 10-minute increments. Patients will also learn to lift for 10 seconds every 10 minutes to relieve pressure. Meticulous skincare is necessary.
Recommended Reading: Snack Ideas For Ulcerative Colitis
Q& a: Clarifying New Guidance For Pressure Ulcers Deep
Q: Our coding department was told there were changes made for fiscal year 2020 when it comes to reporting healed/healing pressure ulcers and pressure-induced deep tissue damage. Can you explain any recent updates?
A: You are right, there have been updates to guidance surrounding these diagnoses.
First, the FY 2020 ICD-10-CM Official Guidelines for Coding and Reporting have additional clarity on patients admitted with pressure ulcers documented as healed. The guidelines added the phrase at the time of admission. The guidelines now state that there is currently no code assignment for pressure ulcers that are completely healed at the time of admission.
In contrast, if the pressure ulcer is documented as healing but not yet healed, the coder is to code the pressure ulcer to the appropriate pressure ulcer stage at the time of admission. Meaning, if the pressure ulcer was to the bone but improves during the stay to only include the depth of the subcutaneous tissue , the pressure ulcer is to be reported as a stage 4 pressure ulcer, not a stage 3.
If a pressure ulcer was present on admission and is healed at the time of discharge, the site and stage of the pressure ulcer at the time of admission should be reported. Remember, healed at the time of admission is the only time a pressure ulcer would not be reported, because it no longer exists.
- L89.126, pressure-induced deep tissue damage of left upper back
- L89.156, pressure-induced deep tissue damage of sacral region
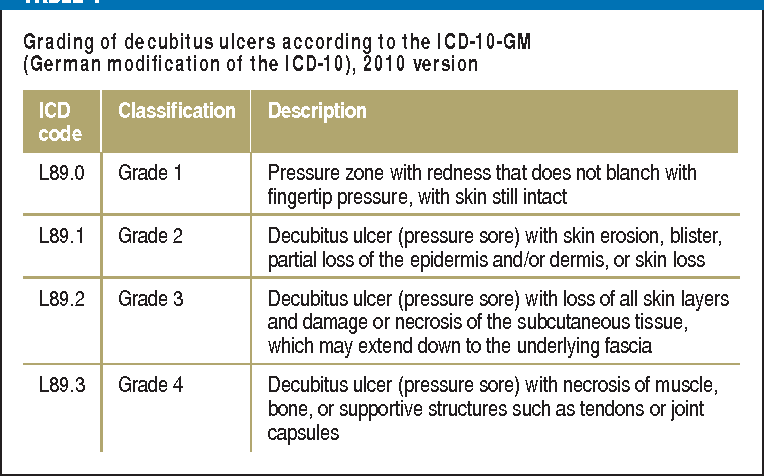
Classification And Differential Diagnosis
Pressure sores are coded under diseases of the skin and its appendages . This disease entity does not include decubitus ulcers of the uterine cervix . The term refers to a wound that develops in the upper layers of the skin as the result of sustained, externally applied pressure and then enlarges both radially and into the deeper tissue layers, unless specific measures are taken to counteract the process . Decubitus ulcers are usually accompanied by an inflammatory reaction, and often by local bacterial colonization or systemic infection. Exudation from large areas of damaged skin leads to fluid and protein loss. Since decubitus ulcers first arise in the upper layers of the skin, then extend outward and downward, their severity is classified according to the depth of extension . Persistent hypoperfusion and pressure injury of the upper layers of the skin result in a circumscribed area of erythema and induration. This erythema does not blanch when the area is depressed with a fingertip or glass spatula . The damage can be reversed by removing the excessive pressure that caused it, as long as there is no open wound. As soon as a grade 1 decubitus ulcer is found, pressure-reducing measures such as pressure-free positioning, frequent changes of position, and frequent inspections should be ordered and carried out.
You May Like: What Pain Reliever Is Safe For Stomach Ulcer
Lolita M Jones Mshs Rhia Ccs
Lolita M. Jones, MSHS, RHIA, CCS has provided Product Consultant services to a warehousing and analytics start-up that developed and marketed decision support software, health outcomes services, and regulatory compliance toolsets. Her goal is to combine her medical coding expertise with data mining-pattern recognition, to help improve data accuracy and compliance in medical coding and reimbursement . Ms. Jones also provides remote and on-site training/consulting in her newly developed Healthcare Data Mining Clinic educational series. She is currently pursuing a Graduate Certificate in Healthcare Data Analytics from a top university. Ms. Jones is based in New York and can be reached at
Pressure Ulcer Icd 10 Causes
The three most important factors that contribute to bedsores are:
- Pressure: Ulcers are caused by pressure on the skin limiting blood flow to the skin. Constant pressure on any part of the body reduces blood flow to the tissues.
- Limited exercise: Lack of blood flow makes the skin more susceptible to damage that leads to the development of bedsores. Blood flow is crucial for supplying the tissue with oxygen and other nutrients. Without these nutrients, the skin and nearby tissues can be damaged and die.
- Friction: Friction occurs when the skin rubs against clothing or bed linen. Friction makes sensitive skin more susceptible to injury, especially when the skin is moist. Shearing occurs when two surfaces move in opposite directions. In people with reduced mobility, this type of pressure tends to occur in non-padded areas such as muscles, fat and low-lying bones such as the spine, coccyx, shoulder blades, hips, heels and elbows. For example, if the bed is lifted, the patients head slips onto the bed. When the tailbone moves, the skin around it stays in place but is pulled in the opposite direction. They are most common in bony parts of the body such as heels, elbows, hips and the base of the spine. They usually develop and form within a few hours.
You May Like: Bentonite Clay For Ulcerative Colitis
Pressure Ulcer Of Sacral Region Stage 4
- 2016201720182019202020212022Billable/Specific Code
- L89.154 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM L89.154 became effective on October 1, 2021.
- This is the American ICD-10-CM version of L89.154 – other international versions of ICD-10 L89.154 may differ.
- Healing pressure ulcer of sacral region, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, sacral region
- Applicable To annotations, or
Pressure Ulcer Of Sacral Region Stage 3l89153
Chapter 12 – Diseases of the skin and subcutaneous tissue » Other disorders of the skin and subcutaneous tissue » Pressure ulcer of sacral region, stage 3
Hierarchy Tree View
YOU AGREE THAT THE INFORMATION PROVIDED ON THIS WEBSITE IS PROVIDED AS IS, WITHOUT ANY WARRANTY OF ANY KIND, EXPRESSED OR IMPLIED, INCLUDING WITHOUT LIMITATION WARRANTIES OF MERCHANTABILITY OR FITNESS FOR ANY PARTICULAR PURPOSE, OR NON-INFRINGEMENT OF ANY THIRD-PARTY PATENT, COPYRIGHT, OR ANY OTHER THIRD-PARTY RIGHT. IN NO EVENT SHALL THE CREATORS OF THE WEBSITE OR WASHINGTON UNIVERSITY BE LIABLE FOR ANY DIRECT, INDIRECT, SPECIAL, OR CONSEQUENTIAL DAMAGES ARISING OUT OF OR IN ANY WAY CONNECTED WITH THE WEBSITE, THE USE OF THE WEBSITE, OR THIS AGREEMENT, WHETHER IN BREACH OF CONTRACT, TORT OR OTHERWISE, EVEN IF SUCH PARTY IS ADVISED OF THE POSSIBILITY OF SUCH DAMAGES.
Also Check: What Is An Ulcer In Your Mouth
Symptoms Of Stage 3 And Stage 4 Pressure Ulcers
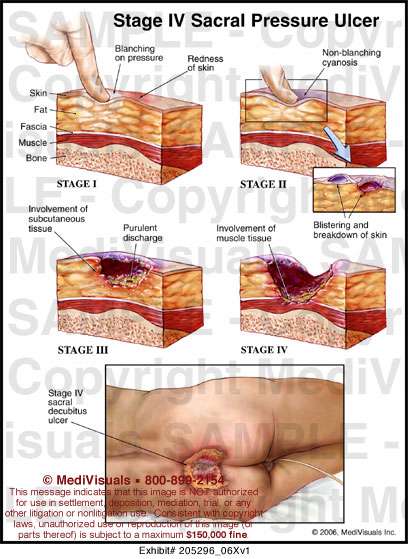
Stages 3 and 4 pressure ulcers have deeper involvement of underlying tissue with more extensive destruction. Stage 3 involves the full thickness of the skin and may extend into the subcutaneous tissue layer granulation tissue and epibole are often present. At this stage, there may be undermining and/or tunneling that makes the wound much larger than it may seem on the surface. Stage 4 pressure ulcers are the deepest, extending into the muscle, tendon, ligament, cartilage or even bone.
Figure 1: Stage 4 sacral pressure ulcerFigure 2: Stage 3 pressure ulcer on hip
Donât Miss: Is Alcohol Bad For Ulcerative Colitis
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Also Check: What To Avoid Eating If You Have An Ulcer
Stages Of Decubitus Ulcers
Stages of decubitus ulcers are classified from Stage I to Stage IV according to the severity of symptoms.
Stage Iâ In fair-skinned individuals, a defined skin area is characterized by persistent redness. Darker skin may come with hues of red, purple of blue. Compared to the other adjacent body area, the changes in the defined area involve skin temperature, sensation, and palpable or felt tissue consistency. When the define area is pressed, the skin does not turn to whiteâ a key indicator that decubitus ulcer has already started to occur.
Stage IIâ At this stage, the decubitus ulcer is still superficial. A blister, an abrasion, or a shallow crater or open sore has formed the surrounding area of which may appear to be irritated and red in color.
Stage IIIâ The superficial ulcer appears like a deep crater, where thick skin loss involves impairment in the skinâs underlying tissue. The depth of damage may reach the fascia, but does not pass through it.
Stage IVâ Further impairment takes place along with the fully thick skin loss. The depth of damage reaches the bone, muscle, or the supporting tendons and joint capsule. Furthermore, sinus tracts may also characterize Stage IV decubitus ulcers.
Audit Considerations & Strategies
- The original coder did not code the pressure ulcer excision. Adding either the right or left hip excision would drive the case from a medical DRG to a surgical DRG
- The procedure code may have been overlooked because the surgeon documented that the tissue was excised rather than documenting that an excisional debridement was performed
- Documentation of excision or excised is sufficient to code PCS root operation: Excision
- Always carefully review the entire medical record including the Progress Notes for bedside procedures, especially for patients with pressure ulcers
- Per Coding Clinic1, the body part value for an excisional debridement performed on a muscle in the sacral region is the Hip muscle. If the documentation specifies that the right side or left side of the sacral ulcer was debrided, then a single code can be assigned. If the documentation does not specify laterality, assign codes for both the right and left hip muscles.
- Since only excision of sacral pressure sore was noted, both the 0KBN0ZZ and 0KBP0ZZ codes were assigned
- Coding Clinic likely allows coders to assume both the right and left hip muscles when laterality is not specified because sacral pressure ulcers often develop on the lower back which would include portions of the left and right hips
- Cases with a principal diagnosis of stage 3 or 4 pressure ulcer automatically result in DRG 592: Skin ulcers with MCC
- ICD-10 only requires one code to be assigned for the pressure ulcer and stage
Reference
You May Like: Ways To Prevent Pressure Ulcers In Hospitals
L895 Pressure Ulcer Of Ankle
Pressure ulcer of unspecified ankle
Pressure ulcer of right ankle
L893 Pressure Ulcer Of Buttock
Pressure ulcer of unspecified buttock
Pressure ulcer of right buttock
Recommended Reading: What Are The Side Effects Of An Ulcer
Diagnosing A Stage 4 Bedsore
A doctor determines the by its appearance. In the case of a stage 4 bedsore, the large wound has passed the bodys fatty tissue layer, exposing muscles, ligaments, or even bone.
In some cases, however, health care professionals may not be able to immediately diagnose a late-stage bedsore by examining it.
A stage 4 bedsore may be initially diagnosed as:
- UnstageableWhen a doctor cannot see the bottom of an open sore, they must clean it out to properly stage it.
- Suspected Deep Tissue Injury This diagnosis happens when the surface of a patients skin looks like a stage 1 or 2 sore, but it is actually affecting deeper tissues underneath.
Also Check: Chances To Win Social Security Disability With Ulcerative Colitis
Pressure Ulcer Of Sacral Region Stage 4 L89154
The ICD10 code for the diagnosis “Pressure ulcer of sacral region, stage 4” is “L89.154”. L89.154 is a VALID/BILLABLE ICD10 code, i.e it is valid for submission for HIPAA-covered transactions.
- L89.154 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2019 edition of ICD-10-CM L89.154 became effective on October 1, 2018.
- This is the American ICD-10-CM version of L89.154 – other international versions of ICD-10 L89.154 may differ.
- Healing pressure ulcer of sacral region, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, sacral region
Read Also: Can You Gain Weight With Ulcerative Colitis
What Is The Cause Of Sacroiliitis
What causes sacroiliitis? Inflammation of the sacroiliac joint causes most of the symptoms of sacroiliitis. Many medical conditions cause inflammation in the sacroiliac joint, including: Osteoarthritis -This type of wear-and-tear arthritis can occur in the sacroiliac joints and results from the breakdown of ligaments.
What Is Sacroiliac Dysfunction
Sacroiliac joint dysfunction occurs when the sacroiliac joints of the pelvis become stiff or weak. The condition can develop at any age. Symptoms typically are felt on one side of the back. SIJ dysfunction is found in 10% to 25% of people who complain of low back pain. It is most often diagnosed in females.
Don’t Miss: What Foods To Eat When You Have A Stomach Ulcer
Complications From Stage 4 Bedsores
Those with a stage 4 bedsore are at high risk of life-threatening complications.
If left untreated, a stage 4 bedsore may lead to:
- AmyloidosisThis is an incurable condition where protein builds up in the body and prevents organs from functioning properly.
- InfectionThose with a stage 4 bedsore are at a very high risk of infections, according to Johns Hopkins Medicine. These infections can affect the skin, bones, blood, and other organs.
- Renal FailureThis occurs when the kidneys can no longer remove waste from the body, causing damage. It can be fatal if left untreated, but recovery may be possible.
- DeathMany of the conditions listed above can be fatal if left untreated. According to an article in the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores.
It may be considered a if a nursing home patient dies from an untreated bedsore.
Donât Miss: What To Eat If You Have Gastric Ulcer
How Do You Treat A Pressure Ulcer In The Tailbone
Caring for a Pressure Sore
Also Check: How Is Ulcerative Colitis Caused