The Link Between Psoriasis And The Immune System
No one ever really considered that the immune system had any real role in psoriasis, or its painful outbreaks. Not until a new drug Cyclosporine was offered to arthritis patients. What happened next was both surprising and unexpected. Patients who were prescribed the immune suppressing drug for their arthritis symptoms , began to report a decrease in their skin attacks. Without warning, researchers were faced with the theory that the immune system could be causing psoriasis.
It didnt take long before researchers began to figure out the mystery of psoriasis in regards to how the immune system can impact it.
The Role of the Immune System on the Skin
The immune system is responsible for standing guard and attacking any invaders which penetrate the body. Since the skins main job is to act as the bodys first defense mechanism against invasion, it is no wonder that the immune system works in close connection with each layer of the skin. Heres how it all works:
1. Immune cells patrol the entire body for dangers. How Well Does Humira Work for Ulcerative Colitis
2. When an invader is detected, these immune send out chemical and nervous system messages to the immune system to ready itself for an attack
Crohns Disease Or Ulcerative Colitis
- In Crohnâs disease or ulcerative colitis, some adults may start to see results within 4 weeks after starting Humira treatment, but most people see an improvement by 8 weeks. In adults with Crohn’s disease, roughly one-third of patients may achieve remission by 4 weeks after starting treatment.
- In clinical studies in children 6 years and older with Crohn’s disease, more than half of the patients on Humira saw symptom relief and many achieved remission at 26 weeks
- In ulcerative colitis studies in children 5 years of age and older, the majority of patients were in remission after 8 weeks of treatment. In addition, many children who responded by week 8 were in remission at 1 year, so the results can be long-lasting.
Crohnâs disease is an inflammatory bowel disease which leads to long-term inflammation of the gastrointestinal tract, usually affecting the intestines, but other areas may be involved as well. Typical symptoms of Crohnâs disease include stomach pain, an urgency to have a bowel movement, weight loss, diarrhea and tiredness.
Ulcerative colitis inflammation affects only the large intestine and ulcers develop along the lining of your colon and rectum. Symptoms may include diarrhea, often with blood or pus, stomach cramping, rectal pain, weight loss, tiredness, or fever.
What You Need To Know About Psoriasis How Fast Does Humira Work For Ulcerative Colitis
Is Your Stomach to Blame?
Who would have thought that a severe psoriasis outbreak could start because of something going wrong inside of your stomach and intestines? Yet, new research developed by psoriasis expert Edgard Cayce shows a distinct link between a leaky gut and a scaly psoriatic episode. According to Cayce, the primary source of psoriasis can be found in the intestinal tract, where toxins are leached into the body. This causes the immune system to react by thickening the skin. At the same time, the skin tries to purge the toxins through its layers, which can cause scabs and sores to form.
Could Arthritis Be the Cuplrit?
The intestines arent the only link to psoriasis found by researchers arthritis seems to also contribute to it. As many as one-third of all psoriasis patients eventually develop some form of psoriatic arthritis. Unlike normal forms of arthritis, those with psoriatic arthritis do not exhibit a rheumatoid factor when their blood is tested. This indicates that the arthritic condition comes solely from either the psoriasis itself or the underlying cause of the skin affliction.
Could a Virus Be the Cause?
Arthritis has been linked to certain virus and so have other auto-immune disorders. This leads some researchers to think that psoriasis too may start with a virus, which is what kicks the immune system into overdrive.
You May Like: Ulcerative Colitis Is It Hereditary
Is Your Ulcerative Colitis Treatment Effective
First, you should know what effective treatment looks like. Your treatment is successful if you are able to form stools without bleeding, cramping, or urgency, says Sunanda V. Kane, MD, a gastroenterologist and a professor of medicine at the Mayo Clinic in Rochester, Minnesota, and a member of the Crohns and Colitis Foundations education committee.
There are two components of effective treatment controlling symptoms and then maintaining that control and both are important parts of truly successful treatment. The goals of therapy include to induce clinical remission and to prevent damage from untreated disease over time, says Jessica Philpott, MD, PhD, a gastroenterologist at the Cleveland Clinic in Ohio. Basically, the goal is to minimize the impact of the disease on you in a way that works best for you and to help you live the life you want to live.
How Long Does Adalimumab Take To Work

Clinical studies have shown that some people start to see results within 4 weeks but most people see them by 8 weeks. If you havent started to notice any difference to your symptoms after 12 weeks then you should contact your doctor, although you should receive regular monitoring from your doctor via appointments and/or blood tests.
Recommended Reading: How To Tell Stomach Ulcer
Tell Your Doctor Or Ibd Team Immediately If You Develop
Around 1 in every 10 people taking adalimumab may have:
- Injection-site reactions
- Upper respiratory tract infections
- Tummy pain or being or feeling sick
- Low white blood cell count or anaemia
- Headaches
- Muscle pain
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.
You May Like: Ulcerative Proctitis Vs Ulcerative Colitis
Antibody Formation To Integrin Inhibitors
Antibody formation to integrin inhibitors has also been described. However, dose adjustment to natalizumab has not been permitted due to safety concerns, and postmarketing experience for vedolizumab is limited thus far. The ENACT -1 trial evaluated natalizumab for induction of remission in CD and described antibody formation in 8% of patients at week 12 of the study. Of the patients who formed antibodies, 14% were on natalizumab monotherapy, 6% were on concomitant oral corticosteroids, and 3% were on other immunosuppressants. Similarly, in the ENACT-2 trial examining natalizumab maintenance therapy, 9% of patients developed antibodies against the drug. Overall, 6% of patients were found to have persistently positive antibodies, while 3% of patients had transient antibodies. Although the presence of antibodies to natalizumab can be evaluated in a commercially available assay, dose adjustment and use of concomitant immunosuppression are not permissible due to the risk of progressive multifocal leukoencephalopathy, a severely debilitating and possibly fatal brain infection. Practically, the only option with loss of response to natalizumab is discontinuation of the drug. If a patient did respond to natalizumab and then had secondary loss of response due to antibody formation, switching medications within the same class would be a reasonable option.
Signs Your Ulcerative Colitis Treatment Isnt Working
After a while on one treatment plan, you may find that your medication doesnt work as well as it used to. Dr. Philpott says that an increase in your bowel movements, trouble or pain passing stool, weight loss, fevers, blood in stool, and fatigue could be signs that its time to discuss a change with your doctor. But, she cautions, It is important to be aware that sometimes these symptoms can occur for a different reason. That is why your healthcare provider should do some tests when this occurs, to identify what is causing the problem.
According to Kane, If you are feeling worse on the medication than off it, it is time to have a discussion with your doctor. Dont be afraid to speak up. Your doctor assumes everything is okay unless you say something, says Kane. She recommends you start by saying something like: Im not sure that my medicine is doing what its supposed to because and then going into detail about your symptoms. Your doctor will appreciate your honesty, she adds.
Philpott says its also important to be prepared going into your appointment. Things to discuss with your healthcare provider would be what the specific symptoms are, when they started, and if notice a fluctuation over time. For example, she says, if youre taking an injection and notice that symptoms start recurring when youre due for the next injection, thats important to note.
Read Also: Foods To Avoid With Ulcerative Colitis
Key Points About Stelara
- Stelara is approved to treat Crohn’s disease.
- The loading dose of Stelara is given by infusion and thereafter is given by injections at home.
- People taking shots for allergies should talk to their doctor about possible allergic reactions and Stelara.
- Common side effects include infections, injection site reactions, and vomiting.
- If you are pregnant or plan to become pregnant, you and your doctor should decide if you should take Stelara.
- It’s thought that Stelara does pass into breastmilk.
- Stelara must be refrigerated.
Key Points About Remicade
- Remicade is given by IV.
- Remicade is approved for Crohn’s disease and ulcerative colitis.
- Three starting doses are given .
- After the starting doses, it’s given about every eight weeks .
- Common side effects are abdominal pain, nausea, fatigue, and vomiting.
- If you are pregnant or plan to become pregnant, you and your doctor should decide if you should take Remicade.
Read Also: What Are Some Symptoms Of An Ulcer
What Should You Know About Biologic Administration Doses And Schedules
A variety of biologic drugs are used to treat Crohn’s disease and ulcerative colitis. Some biologics treat both conditions, while others treat only one. There are several ways biologics are administered, dosed, and scheduled. Talk to your gastroenterologist and health care team about the specific usage guidelines for your prescribed medications.
Biologics used to treat Crohn’s disease and ulcerative colitis include a class of drugs called tumor necrosis factor-alpha inhibitors that target specific inflammatory proteins in the immune system. Some of these include:
Other biologic drugs known as integrin receptor antagonists block a protein on the surface of cells that cause inflammation. This process keeps the proteins from leaving the blood vessels and entering tissues. Examples of integrin receptor antagonists are Tysabri and Entyvio .
A third type of biologic targets interleukin proteins in the immune system, including IL-12 and IL-23, to reduce inflammation. Stelara is an example of an interleukin inhibitor that treats IBD.
Key Points About Cimzia
- Cimzia is approved to treat Crohn’s disease.
- Cimzia is usually given at home by injection.
- Cimzia is given initially three times in a series of two injections, two weeks apart, followed by two injections every four weeks.
- Common side effects include respiratory infections, viral infections, rashes, and urinary tract infections.
- If you are pregnant or plan to become pregnant, you and your doctor should decide if you should take Cimzia.
- A low amount of Cimzia may pass into the breastmilk.
- Cimzia needs to be refrigerated.
Also Check: Stomach Ulcer Blood In Stool
Ask About Adding Another Medication
Sometimes one medication isnt enough to tackle severe UC symptoms. Your doctor might give you a second medication to help you manage your condition. For example, you might need to take both a biologic and an immunosuppressant drug.
Taking more than one medication can increase the odds of treatment success. It can also increase your chances of experiencing side effects. The doctor will help you balance the benefits and risks of the medications you take.
How To Know When You May Need To Switch Crohns Medication
When you discuss your treatment plan with your doctor, you will be informed how long it may take to see improvement of your symptoms, as well as any potential side effects of the medication. Some drugs take longer to work than others, so it may take a few weeks, or it may take up to a couple of months before you see a benefit, Levy says.
As you undergo your treatment, your healthcare team will closely monitor your symptoms and watch for potential side effects or complications. This will vary by patient, but we objectively assess them at regular intervals, in terms of their clinical status, how theyre feeling, and where their disease is, says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio.
If your symptoms are not improving in the time period in which they are expected, your doctor may either up your dose or change your prescription to a new drug.
If your symptoms have improved, your doctor will still want to know that your insides are healing. Thats why around the six-month mark, you will likely undergo imaging tests to see if your intestines are still inflamed. If you have not achieved endoscopic remission even if you are feeling better your drug therapy may need to be adjusted, Levy says.
Its also possible for medication to work initially and then stop working. Unfortunately, this is not uncommon, Dr. Philpott says.
Your doctor will work with you to adjust or change your therapy as needed.
You May Like: What Is The Medicine For Ulcer
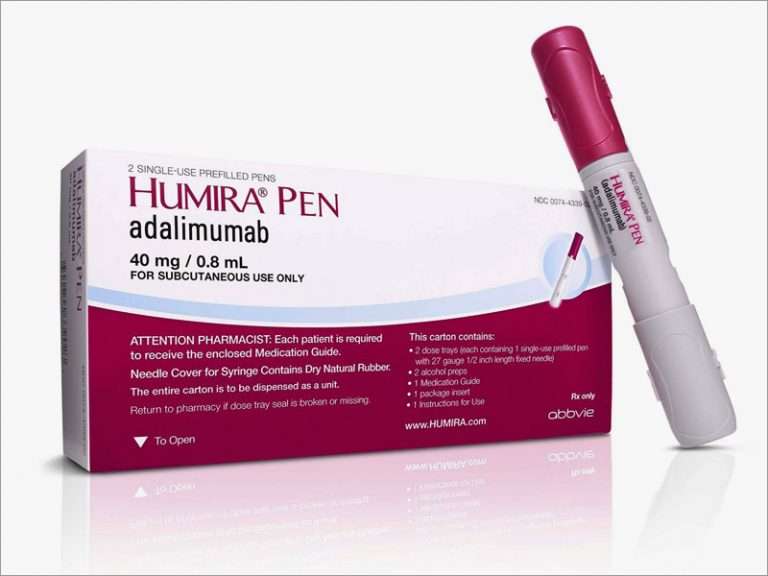
What Are The Typical Dosages Of Humira
When used for certain conditions, your first dose of Humira will be higher than your normal dose. This is called a loading dose, and its given to help the drug start working quickly to treat your condition.
Then, your doctor will lower your dosage over time to reach the right amount for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The maximum dosage for Humira will depend on the condition its being used to treat.
The information below describes dosing schedules that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
Dosage for ulcerative colitis
When Humira is used for ulcerative colitis in adults, treatment starts with a loading dose of 160 mg. This can be given as one dose in a single day or split into two doses over 2 days. For example, you might take 80 mg on day 1 and another 80 mg on day 2.
Two weeks after your loading dose , youll receive an 80-mg injection. And 2 weeks after that , youll start taking 40 mg every other week.
Humira is available in a starter kit that helps you follow this dosing schedule. The kit contains prefilled Humira pens.
Dosage for hidradenitis suppurativa
Two weeks after your loading dose , youll receive an 80-mg injection. And 2 weeks after that , youll start taking either 40 mg weekly or 80 mg every other week.
Dosage for rheumatoid arthritis
Dosage for plaque psoriasis
Adalimumab In Ulcerative Colitis: Real
Although adalimumab has been recently licensed, multiple lines of evidence from open-label and retrospective studies on adalimumab, administered for compassionate use in ulcerative colitis patients, have been available for several years . Oussalah et al first presented data on 13 ulcerative colitis patients treated with adalimumab in 2008. All of the patients had been previously treated with infliximab, and most of them had been previously treated with thiopurines. Patients were treated with adalimumab, with an induction dose of 160/80 mg at weeks 0 and 2, and then maintained with 40 mg EOW. The primary endpoint was defined as the proportion of patients on adalimumab therapy during the study. After a median follow-up of 41 weeks, the percentage of patients remaining on adalimumab therapy was 32.5%. Eight patients discontinued adalimumab: six due to colectomy, one due to lack of response, and one due to an exacerbation of psoriasis. No significant differences were found in adalimumab withdrawal and colectomy rates between the patients who lost response to infliximab and those who became intolerant. From this small cohort of difficult-to-treat patients who had already been treated with all of the main available therapies, adalimumab treatment potentially avoided colectomy in about half of them.
Read Also: Food For Ulcer Patient In Nigeria
Leaving Abbvie Web Site
You are leaving the AbbVie Web site and connecting to a site that is not under the control of AbbVie. AbbVie is not responsible for the contents of any such site or any further links from such site. AbbVie is providing these links to you only as a convenience and the inclusion of any link does not imply the endorsement of the linked site by AbbVie. You should also be aware that the linked site may be governed by its own set of terms and conditions and privacy policy for which AbbVie has no responsibility.
Conversely, the presence of this link does not imply the linked site’s endorsement of HUMIRA.com or AbbVie.
Do you wish to leave this site?