Sociodemographic And Clinical Characteristics
Patients with IBD UC and n=86 CD) included 51.7% males, 58.2% married, 51.6% resided in urban areas, 76.9% highly literate, and 82.4% non-smokers. The average age was 27.0±7.3 years, with the majority ranging from 20 to 35 years. Normal BMI was a predominant feature , and 31.9% were overweight. Patients’ other sociodemographic characteristics are shown in .
Kaplan-Meier analysis of the probability of improvement in IBD symptoms in relation to with H. pylori infection and IBD treatment strategy
How Is H Pylori Treated
If you dont have symptoms, you dont need to be treated. If youve been diagnosed with H. pylori, avoid taking nonsteroidal anti-inflammatory drugs. These drugs can increase your risk of developing an ulcer.
H. pylori-caused ulcers are treated with a combination of antibiotics and an acid-reducing proton pump inhibitor.
- Antibiotics: Usually two antibiotics are prescribed. Among the common choices are amoxicillin, clarithromycin , metronidazole and tetracycline.
- Proton pump inhibitor: Commonly used proton pump inhibitors include lansoprazole , omeprazole , pantoprazole , rabeprazole or esomeprazole .
- Bismuth subsalicylate: Sometimes this drug is added to the antibiotics plus proton pump inhibitor combinations mentioned above. This drug protects the stomach lining.
Combination treatment is usually taken for 14 days.
One newer medication, Talicia®, combines two antibiotics with a proton pump inhibitor into a single capsule.
Also Check: Mouth Ulcers Treatment Home Remedies
What To Expect After H Pylori Treatment Gastroenterologist Explains
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
What you need to know:
The standard h. pylori treatment course eradicates it in most cases. However, you have a 20% chance of treatment failure. Your doctor often needs to re-test for h. pylori to confirm its eradication.
Treatment of H. pylori improves your symptoms and decreases the risk of ulcers, gastric cancers, and others.
Persistence or recurrence of your symptoms may indicate h. pylori treatment failure.
However, symptoms are not an accurate assessment of treatment failure. Testing is a must.
Read Also: Alginate Dressings For Treating Pressure Ulcers
Immunohistochemical Stain For H Pylori
Tissue sections were stained with immunohistochemical stain using a polyclonal antibody directed against the whole H. pylori organism . Negative controls were sections treated as above, but instead of incubation with the primary antibody, they were incubated with 1% bovine serum albumin/PBS. The H. pylori organism appeared as spiral-shaped, rods or coccoid forms stained with a brown color.
Can H Pylori Cause Ulcerative Colitis
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
Read Also: Medications Used For Ulcerative Colitis
Molecular Mechanism By Which H Pylori Induces Immunosuppressive Tregs
TGF- and IL-10 are two important and well-recognized immunoregulatory factors,, and these molecules are associated with IBD onset and Treg-modulated intestinal mucosal homeostasis,,, which suggest that tolerogenic DCs may induce and maintain Treg differentiation via IL-10- and TGF–dependent mechanisms. Pretreatments with TGF– and IL-10-neutralizing antibodies reversed the ameliorated colitis pathology and the upregulation of Treg/Th17 ratio after H. pylori stimulation further proved this hypothesis,. Intestinal epithelial cells derived from IL-10/ mice only express RelA -B subunit), but not phosphorylated Smads, after pathogen stimulation. Meanwhile, TGF- was shown to activate Smad signaling to inhibit Toll-like receptor expression and NF-B pathway-related proinflammatory cytokine secretion. In addition, Engler et al. revealed a significant correlation among CDX2, MUC2, and TGF-, and demonstrated the activation of the TGF–dependent Samd-CDX2-MUC2 axis after H. pylori infection or extraction treatment can increases intestinal mucus secretion and ameliorate experimental colitis . In summary, these evidences indicated TGF- and IL-10 are critical factors for Treg differentiation and activation of protective Smad signaling after bacterial pathogen stimulation.
Testing For H Pylori Antigen In The Stool
Monoclonal antibody testing for H. pylori Ag in stool was performed for confirmation following detection of the organism in colonic tissue by both Giemsa and Immunohistochemical methods.
Testing for H. pylori antigen in the stool was done to confirm infection and to assess cure after therapy. Successful eradication of H. pylori was confirmed by a negative result 4 wk after the end of treatment.
Also Check: Foods To Avoid With Ulcerative Proctitis
Association Between Helicobacter Pylori And Inflammatory Bowel Disease
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| First Posted : January 29, 2019Last Update Posted : June 30, 2021 |
Introduction:
Helicobacter pylori has been linked to a variety of gastric and extra gastric diseases. Chronic infection with H. pylori causes histologically evident gastritis in all colonized individuals and is the predominant risk factor for gastric and duodenal ulcers as well as gastric adenocarcinoma. However, increasingly robust experimental and epidemiological evidence suggests that H. pylori may at the same time be beneficial to its carriers, as it efficiently prevents allergic disorders and chronic inflammatory conditions .
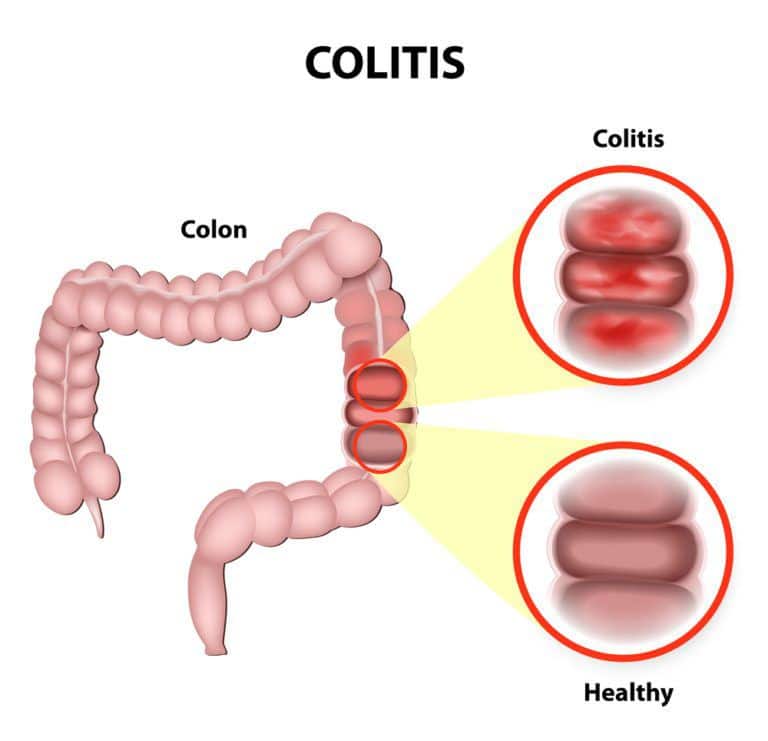
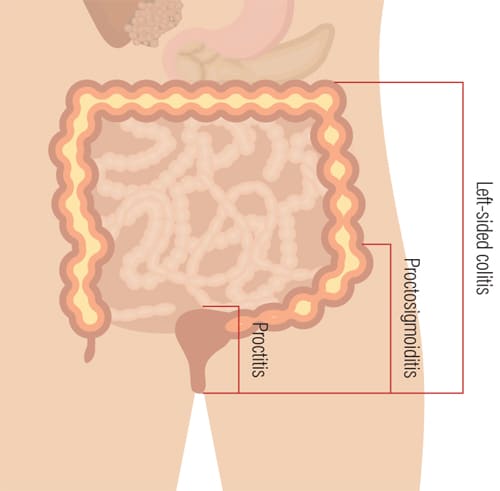
Inflammatory bowel disease is characterized by chronic, nonspecific intestinal inflammation with an unexplained pathology and an alternating relapsing and remitting clinical progression. IBD is divided into two subtypes: ulcerative colitis and Crohn’s disease . Most studies in the IBD field attribute its etiology to the complex interactions among immune dysfunction, genetic susceptibility of the host, and environmental risk factors.
PATIENT AND METHOD :
Inclusion Criteria:
Exclusion Criteria:
Patient And Public Involvement
We informed the patients about the aims and concerns of the study and how it will add to better understanding of their disease aetiology and triggering factors, which was highly appreciated by the patients, and motivated them to be a part of the cohort intended for the long-term follow-up by the clinicians. However, it was not appropriate or possible to involve patients or the public in the design, conduct, reporting or dissemination plans of our research. All the laboratory and clinical data were reported to the study participants, where we discussed the study findings in a simple language.
Recommended Reading: Drinking Alcohol With Ulcerative Colitis
Association Between H Pylori And Ibd
Recently, emerging epidemiologic studies and animal experiments revealed an inverse correlation between H. pylori infection and IBD onset, suggesting that H. pylori colonization exerts a special protective effect on autoimmune diseases. Since the twenty-first century, improving hygienic conditions and socioeconomic status have reduced the H. pylori infection rate and this trend has concurrently been accompanied by an increased IBD incidence in most countries. Most experts in the IBD field interpret this phenomenon based on the hygiene hypothesis: H. pylori infection during childhood contributes to immune system development and may prevent the onset of autoimmune or allergic diseases. Moreover, due to the initiation of H. pylori eradication for peptic ulcers, the incidence of IBD has increased steadily in these regions. Further clarification of the protective effect of H. pylori on IBD and the underlying mechanism will be important for H. pylori infection management strategies and the treatment and prevention of IBD .
Fig. 1: H. pylori infection induce tolerogenic DCs and immunosuppressive Tregs.Fig. 2: The molecular mechanism underlying the protective effect of H. pylori on IBD.
What Causes H Pylori Infections
Its still not known exactly how H. pylori infections spread. The bacteria has coexisted with humans for many thousands of years. The infections are thought to spread from one persons mouth to another, like by kissing.
The bacteria may also be transferred through contact with vomit or stool. This can happen when a person does not wash their hands thoroughly after using the bathroom. H. pylori can also spread through contact with contaminated water or food.
Dont Miss: Stomach Ulcer Treatment Over The Counter
Recommended Reading: What Is Good For Ulcers In Your Mouth
Study Population And Sampling
We conducted a prospective observational study at Alexandria University Student Hospital that is affiliated with Alexandria University, Egypt and serves students, faculty and staff members. AUSH comprises outpatient clinics and inpatient and emergency departments with a bed capacity of 1000. We enrolled patients aged 18 years with confirmed IBD and commenced IBD treatment . Patients with irritable bowel syndrome were excluded according to the Rome III criteria.
Clinicians on the staff of the Internal Medicine Department of the AUSH selected the treatment . The prescribed treatment is the standard of care adopted by the AUSH for treating patients with IBD. Details of the treatment regimens and the parameters employed to select standard or biological treatment are described in .
Covariates Associated With Cu
According to results of univariable analysis , female sex, comorbid allergic rhinitis, asthma, renal disease, diabetes, rheumatic disease, malignant tumor, and atopic dermatitis appeared to be associated with increased risk of CU, but all the associations were not statistically significant .
|
Table 2 Univariable Analysis of Covariates Associated with Chronic Urticaria |
Dont Miss: Best Medicine For Stomach Ulcer Pain
Also Check: Acupuncture For Ulcerative Colitis Treatment
Epidemiological Evidence Suggests An Inverse Association Between Active H Pylori Infection And Ibds
All meta-analyses and almost all original articles covering the topic consistently find a strong negative association between H. pylori colonization and the IBDs. However, several aspects remain underexamined. These include the effects of H. pylori eradication therapy on IBD risk: do patients exhibit a higher IBD risk after successful treatment of their H. pylori infection with antibiotics? Or is the protective mechanism still active even after successful eradication? Another aspect worthy of investigation is the genetic makeup of the colonizing strain: do some strains protect better than others? Can tolerance determinants’ or protective determinants’ be identified that contribute to the reduction in IBD risk? Such detailed questions require mechanistic studies that ideally use various complementary models of IBD. The experimental data available to judge the effects of active H. pylori infection on chronic intestinal inflammation in innate and adaptive models of IBD are discussed below.
The Potential Protective Effect Of H Pylori Infection On Ibd
Numerous studies have reported a lower H. pylori infection rate in patients with CD and/or UC than in non-IBD control individuals,,,,,,,,,,,,,,,,,,,, although a small number of studies showed no significant association,, . The inverse correlation between IBD and H. pylori infection suggests that the gastric mucosa colonization of H. pylori can potentially protects against the pathogenesis of IBD via a special mechanism. Two meta-analyses, provide more powerful evidence supporting this protective effect of H. pylori infection on the prevalence of IBD . However, the significant heterogeneity, among the included studies and the potential publication bias largely limited the confidence of this negative correlation. Differences in H. pylori detection methods, IBD diagnostic criteria, study sites, participant ages, and histories of antibiotic therapy potentially contribute to the severe heterogeneity, which was not resolved by a subgroup analysis. However, a recent meta-analysis without statistical heterogeneity and publication bias also reported an inverse correlation between H. pylori infection and IBD prevalence in an Asian population .
Table 1 Prevalence of H. pylori infection in patients with IBD compared with the control population
Read Also: Ulcerative Colitis Kidney Stones Type
Association Between Helicobacter Pylori Infection And Ulcerative Colitis
Xi Jin* , Yi-peng Chen*, Shao-hua Chen, Zun Xiang
Department of Gastroenterology, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, P.R. China.* These authors contribute equally to this paper as the first author.
Corresponding author: Xi Jin, Digestive Department, The First Affiliated Hospital, College of Medicine, Zhejiang University, No.79 Qingchun Road, Hangzhou, Zhejiang 310003, P.R. China. Fax: 86-571-87236611 Tel: 86-571-87236603 Email: jxfl007com.More
Citation:Helicobacter PyloriInt J Med Sci
Association Between Helicobacter Pylori Infection And Ulcerative Colitis: A Meta
Abstract
Background: Ulcerative colitis , a chronic inflammatory disease that can cause bloody diarrhea, remains a major global disease burden. While Helicobacter pylori infection is postulated to be able to reduce the occurrence of UC, its role in the disease itself remains contentious. Hence, this meta-analysis aims to examine whether H. pylori infection can lower the chance of developing UC.
Method: A systematic search was conducted through three electronic databases, namely Cochrane, PubMed, and Embase, with the addition of individual hand searching to analyze the association between ulcerative colitis and H. pylori infection in the adult population. Relevant articles selected through eligibility criteria were assessed for quality by using the Newcastle-Ottawa Scale. Furthermore, a random-effects meta-analysis was conducted to estimate the pooled odd ratios along with their 95% confidence intervals . Higgins test and funnel plots were also conducted.
The present study adds to the growing body of evidence supporting the potential protective effects of H. pylori infection on the occurrence of UC. However, further primary research with prospective study design needs to be conducted to confirm our findings.
Keywords
Don’t Miss: What Not To Eat When You Have Ulcerative Colitis
Demographic Anthropometric And Serologic Data Of Enrolled Patients
As shown in Table Table1,1, the age and gender distribution were balanced between patients from two groups. BMI in UC group was lower than that in control group but not reached statistical significance. The differences in the rates of hypertension and diabetes between two groups were also not significant. However, compared with UC group, rate of smoking history was approximately twice time higher in control group , reinforcing the previous hypothesis that smoking was protective for UC. In addition, two inflammation and infection associated markers were significantly higher in UC group, reconfirming the involvement of inflammation in disease pathogenesis.
Dendritic Cells Capture H Pylori Antigens In The Gastric Cavity
Although numerous epidemiological studies and meta-analyses support the inverse correlation between H. pylori infection and IBD onset, the protective mechanism by which the upper digestive tract colonization of H. pylori can protect against IBD remains unclear. As the most powerful antigen-presenting cell and the unique activator of naive T lymphocytes , DCs have a key role in modulating adaptive immunity through the presentation of pathogen antigens and induce Th0 cells to differentiate into different lymphocyte subsets. Using two-photon microscopy to observe transgenic pCD11c-YFP mice, Kao et al. reported that CD11c+DCs are located near the gastric luminal surface and submucosal layer, and the number of DCs in the lamina propria was dramatically increased and DCs moved closer to the epithelial surface after H. pylori infection. Moreover, through a three-dimensional co-culture system that includes monocytes, DCs and a Caco-2 cell monolayer in a type I bovine collagen system, Leonard et al. observed DCs can move to the surface of Caco-2 cell monolayer or integrated with it. These studies indicated DCs can migrate through the intestinal epithelium to sense gastrointestinal tract antigens without impairing the integrity of the epithelial barrier.
Read Also: What Are The Best Foods To Eat With An Ulcer
When And How Your Doctor Will Confirm The Eradication
Your doctor will confirm the eradication fro H. pylori after at least four weeks after the end of the treatment course .
Your doctor will confirm the eradication using one of:
It is vital to stop PPIs one or two weeks before the test. PPI may affect the results of h. pylori eradication .
Also, h. pylori blood tests are not accurate in assessing the eradication. Antibodies persist in your blood. Hence theyre not able to differentiate between current and prior infection .
The Crosstalk Between Hp Eradication And The Immune Response
In addition, H. pylori eradication therapy may trigger the onset of IBD. However, the evidence supporting this hypothesis is limited and inconclusive, because limited supportive data are available. One case report from Jovanovic et al. examined one 28-year-old male patient who received 2 weeks of eradication therapy for ulcer-like dyspepsia symptoms. Six months after therapy, he experienced crampy abdominal pain, mild periodical fever, and watery diarrhea, and an endoscopic examination revealed segmental stenotic and Crohns-like lesions in the upper portion of the small intestines. In addition, Tursi reported two severe cases of CD with multiple ulcers and full-thickness lymphoid infiltrates after H. pylori eradication therapy. The authors hypothesized that the breakdown of the equilibrium between the Th1 and Th2 responses and subsequent Th1 polarization might favor the onset of CD in some genetically susceptible individuals. However, in a small-sample H. pylori eradication cohort study of six patients with quiescent CD, statistically significantly differences in the CDAI , CRP , and fecal calprotectin levels were not observed after H. pylori eradication. Further studies are urgently needed to reveal the relationship between H. pylori eradication and IBD onset or progression.
You May Like: What’s The Difference Between Ulcerative Colitis And Crohn’s Disease
Diagnostic Strategy In Helicobacter Pylori
As reviewed, there may be several causes of H. pylori-negative DUs . Accordingly, the first and most important action on encountering a patient with unexplained DU is to double check that he/she is truly H. pylori-negative, trying to rule out false negatives of H. pylori diagnostic methods. This may be done by using more than one H. pylori diagnostic test, by taking biopsies from several gastric sites and by testing H. pylori after stopping PPIs and antibiotic treatments. If biopsy-based tests are negative, consider performing non-invasive tests, such as C-urea breath test or serology. DU patients truly H. pylori-negative, the second most important step would be to exclude NSAID use. If this risk factor is not easily recognized by the patient, the unrecognized or surreptitious NSAID use should be intentionally and carefully searched and the measurement of serum and urine salicylate levels may be considered. If surreptitious NSAID use is ruled out , biopsies from the duodenum should be obtained to discard isolated H. pylori duodenal colonization and also diseases of the duodenal mucosa . If the aetiology of the ulceration remains unexplained, serum gastrin levels should be measured to rule out ZollingerEllison syndrome. Obviously, a careful clinical history should always be obtained and the habits and the concomitant diseases of the patient determined. The recommended diagnostic strategy for the patient with H. pylori-negative DU is summarized in .
Helicobacter pylori