Who May Be Liable For Stage 2 Bedsores
Any member of a nursing home health care team may be accountable for a Stage 2 bedsore, including:
- A doctor that fails to diagnose a Stage 2 bedsore
- A nurse or caregiver that overlooks a Stage 2 bedsore
- A nurse or caregiver that does not clean a Stage 2 bedsore properly, leading to infections
- A nurse or caregiver that fails to reposition a patient, provide adequate hygiene care, or perform other duties to prevent Stage 2 bedsores
Regardless of who is at fault, the nursing home will be liable for the victim’s Stage 2 bedsores and resulting losses. Your nursing home abuse attorney will help you determine all possible responsible parties during your free legal case review.
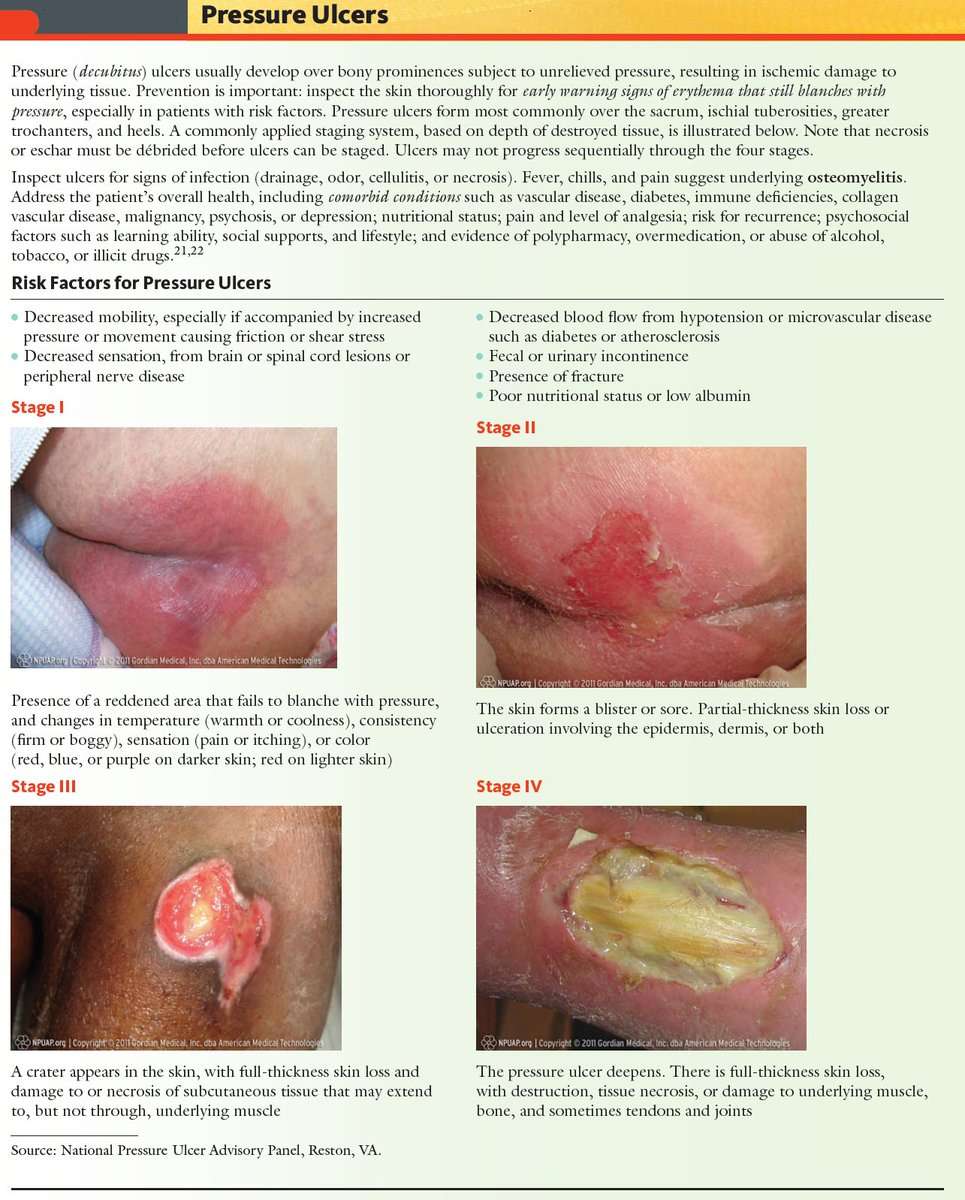
Stages Of Decubitus Ulcers
The National Pressure Ulcer Advisory Panel has developed a series of four stages of a decubitus ulcer to aid in diagnosis and treatment.Stage I: The skin is discolored but not broken. Light-complexioned people may have red marks. Dark complexioned people may have a discoloration that is blue or purple. In some people, the discoloration is white.Stage II: Skin breaks open and the ulcer is shallow with a reddish or pinkish wound bed. There may be tissue death around the wound, or a fluid-filled blister.Stage III: Ulcer on the skin is deeper, affecting the fat layer and looking like a crater. Pus may be in the wound.Stage IV: Ulcer moves to deeper layers of muscle or bone. A dark material called “eschar” may be inside the ulcer.Unstageable: An ulcer that is yellow or green. It might have a brown scab covering it, or be soft and look pus filled. A dry and stable ulcer surface is the body’s natural protection and should be allowed to continue healing. However, if extensive tissue damage is evident, the covering might need to be removed for treatment.
How Are Bedsores Treated
Specific treatment of a bedsore is discussed with you by your healthcare provider and wound care team and based on the severity of the condition. Treatment may be more difficult once the skin is broken, and may include the following:
- Removing pressure on the affected area
- Protecting the wound with medicated gauze or other special dressings
- Keeping the wound clean
Healthcare professionals will watch the bedsore closely. They will document size, depth, and response to treatment
Recommended Reading: Medicine To Help Stomach Ulcer
Preventing Stage 2 Bedsores
The best way to prevent stage 2 bedsores is to identify stage 1 bedsores and treat them before they worsen. Stage 1 bedsores have not broken the skin and usually look like reddish or discolored spots on the body. Stage 1 bedsores usually can be cured within a few days while stage 2 bedsores can take a few weeks to heal.
Nursing home attendants and nurses should regularly check residents at risk for signs of developing bedsores. Caretakers should check patients skin from head to toe. These skin assessments should take place at least once a day.
Patients who are at high risk of developing bedsores should be checked as often as is reasonable. Those at risk are often elderly or have a health condition that limits their mobility. People are at higher risk of developing bedsores if they use a wheelchair, spend a lot of time in bed, or need assistance to move. Conditions that can raise the risk of developing sores include mental conditions like alzheimers and physical conditions like paralysis.
Identifying A Stage 2 Bedsore
Stage 2 bedsores can be identified as an intact blister or shallow open sore. These sores are often red or pink and surrounded by red and irritated skin. These sores may also be moist if pus or fluid is present.
Human skin is made up of layers. The topmost level is called the epidermis. A stage 2 sore has broken the epidermis to create an open wound. The second layer of skin, the dermis, is visible in stage 2. In some cases, the dermis is broken.
Stage 2 bedsores have broken the skin but have not broken past the dermis to fat. The deeper a sore goes, the more difficult it will be to treat and the longer it will take to heal. People who are at risk of developing bedsores should receive regular skin checks to identify bedsores before they progress past stage 2.
Signs of a stage 2 bedsore include:
- Intact or ruptured blister
- Redness or discoloration
Identifying a stage 2 sore as soon as possible is imperative. Complications can occur when bedsores go unnoticed and untreated. In serious situations, bedsores can become life-threatening or lead to amputation. If a sore becomes infected, the infection can spread to the blood, heart, or bones.
Notify a doctor or other healthcare provider if you or a loved one has developed a stage 2 bedsore. A health professional can decide the best plan of action to treat the bedsore properly.
Recommended Reading: Ulcerative Colitis Colon Cancer Screening
The Challenge To Manage Pressure Ulcers
We all want to avoid pressure ulcers. Considerable progress has been made in this area the past few years. Nevertheless, pressure ulcers remain a challenge. B. Braun offers different solutions including products for skin care, wound bed preparation and infection management, as well as exudate management. Taking action right from the start helps you to prevent the aggravation of existing pressure ulcers and to support the healing process.
You May Like: How To Cure Skin Ulcer
Appendix 1 Pressure Ulcer Grading
One of the most widely recognised systems for categorising pressure ulcers is that of the National Pressure Ulcer Advisory Panel . Their international classification recognises four categories or stages of pressure ulcer and two categories of unclassifiable pressure injury, in which wound depth and/or extent, or both, cannot be accurately determined unclassifiable pressure ulcers are generally severe and would be grouped clinically with Stage 3 or Stage 4 ulcers :
The two additional categories of unclassifiable wounds are:
- Unstageable/unclassified Obscured fullthickness skin and tissue loss: Fullthickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
Read Also: What Are The Symptoms Of A Duodenal Ulcer
What Are The Symptoms Of Stage 2 Pressure Ulcers
Stage 2 pressure ulcers are open, shallow, broken wounds with a red base. Intact or incompletely ruptured blisters may also be present with clear fluid or pus seeping from the affected area, and the skin to it adjacent may be discolored. It may involve both the dermis and epidermis of the skin.
Stage 2 bedsores are common in ankles and heels, back of the head, hip, shoulder blades, and tailbone. However, it can develop in any part of the body under constant pressure. Still, areas near bones are at a higher risk.
There is more significant pain in stage 2 bedsores than in stage 1 bedsores. The pain decreases as the sore worsens but becomes harder to treat, leading to fatal complications.
Stage 4 Bedsore Prevention
The best way to prevent a stage 4 bedsore is by being proactive. If your loved one is at risk for bedsores, you can help them take the following precautions.
To prevent stage 4 bedsores, you can:
- Avoid buttons on clothes and wrinkles in bedding
- Avoid doughnut cushions, as they can add pressure to surrounding areas
- Change bedding and clothing on a regular basis
- Check skin daily
Also Check: Is Peppermint Tea Good For Ulcerative Colitis
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Read Also: How Do Doctors Test For Ulcerative Colitis
Complications From Stage 4 Bedsores
Those with a stage 4 bedsore are at high risk of life-threatening complications.
If left untreated, a stage 4 bedsore may lead to:
- AmyloidosisThis is an incurable condition where protein builds up in the body and prevents organs from functioning properly.
- InfectionThose with a stage 4 bedsore are at a very high risk of infections, according to Johns Hopkins Medicine. These infections can affect the skin, bones, blood, and other organs.
- Renal FailureThis occurs when the kidneys can no longer remove waste from the body, causing damage. It can be fatal if left untreated, but recovery may be possible.
- DeathMany of the conditions listed above can be fatal if left untreated. According to an article in the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores.
It may be considered a if a nursing home patient dies from an untreated bedsore.
Also Check: What Do You Do If You Have An Ulcer
Also Check: What Foods Irritate Stomach Ulcers
Diet And Lifestyle Changes To Avoid Pressure Sores
Changes to avoid pressure sores include:
- Make sure you eat a healthy and nutritious diet. This includes a balanced diet and fluids/water. And if necessary,youre your doctor about vitamin and nutritional supplements .
- Low body weight or being overweight can cause pressure sores, so make sure you maintain heathy body weight
- If youre malnourished or at risk of malnutrition, protein, fluid and energy intake should be increased.
- Be aware of using good hygiene practices.
- Maintain activity levels, where appropriate.
- Make sure you quit smoking.
Symptoms Of Stage 2 Bedsores
The most notable symptom of a stage 2 bedsore is an open wound that has broken the top layer of skin called the epidermis. Stage 2 bedsores may also reach the dermis, which is the layer of skin below the epidermis.
Stage 2 bedsores can develop anywhere. However, areas close to bones are at a greater risk.
Bedsores often form around the:
- Ankles and heels
- Shoulder blades
Clear fluid or pus may leak from the affected area, and the nearby skin may be discolored.
Additionally, Johns Hopkins University notes that patients with stage 2 bedsores complain of significant pain more so than those with stage 1 bedsores. The pain may lessen as the sore worsens, but it will become harder to treat and can lead to deadly problems.
You May Like: Offloading The Diabetic Foot For Ulcer Prevention And Healing
Prevention Of A Decubitus Ulcer
At risk individuals should be checked for signs of the development of a decubitus ulcer every day. Caregivers need to examine the person’s body from head to toe, paying particular attention to bony areas where decubitus ulcers tend to develop. They should look for areas of skin that don’t turn white when pressed. Other preventative measures include:
- Changing the person’s position every two hours
- Using supporting items like pillows or foam pads reduce pressure over pressure points
- Keeping skin clean and dry and applying moisturizing lotions made especially for fragile skin
- Providing the person will well-balanced, nutritious meals and 8-10 glasses of water daily
- Helping the person do daily range-of-motion exercising
- Cleaning carefully after urination or bowel movement and applying cream formulated for fragile skin if necessary
Causes Of Stage 2 Bed Sore
Bedsores or pressure injuries occur in the bloodstream that stops functioning correctly. Having to lie still and not get enough sleep reduces blood flow affecting surrounding tissues.
Stage 1 bedsores do not break the skin however, sitting at the same place when the skin forms may tear the skin up and cause Stage 2 bedsores to develop.
A nursing home ill-tended may be associated with swollen feet or bed. A lack of training and understaffing may inhibit the ability of staff to accommodate resident mobility needs.
If stage one bedsores are not treated quickly or effectively, they may develop into them. At this time, bedsores have slipped through skin layers to form open blisters that usually cause irritation or discoloration.
Patients with mobility issues often risk bedsores .
Symptoms are asymptomatic, may result in life-threatening conditions if left untreated, and are rare for bedsores.
Proper treatment of aging adults is helpful in recovery. Stage 2 bedsores are signs that nursing homes have abused or neglected their staff or patients.
Read Also: What Do You Do For A Peptic Ulcer
Summary Of Findings For The Main Comparison
NMA evidence for individual network: proportion with complete healing interventions versus saline gauze
1Majority of evidence at high risk of bias imprecision: very wide CI .2Imprecision: very wide CI .3Majority of evidence at high risk of bias imprecision: wide CI and direct evidence on collagenase from three studies, 11 events .4Majority of evidence at high risk of bias : imprecision: wide CI and direct evidence on dextranomer from one study, seven participants and four events .5Majority of evidence at high risk of bias imprecision: wide CI .6Majority of evidence at high risk of bias inconsistency: heterogeneity in direct evidence imprecision: wide CI .7Majority of evidence at high risk of bias inconsistency: significant difference between direct and indirect estimates imprecision: very wide CI .8Imprecision: wide CI .9Majority of evidence at high risk of bias : imprecision: wide CI and direct evidence on tripeptide copper gel from one study, six participants and five events .
In this section, we present the results for the individual NMA. Results for the group network are given in Appendix 5.
Interventions and comparisons
The individual network comprised 21 interventions: 13 eligible dressings six topical agents and two supplementary linking interventions .
Risk of bias for the individual network
We report risk of bias in three ways :
Network metaanalysis results
Also Check: How Do You Get Ulcers In Your Stomach
What Is A Pressure Injury
A pressure injury is an area of injured skin. A pressure injury happens when force is applied on the surface of the skin. This force can be a constant pressure on an area of skin or a dragging force between the skin and another surface. These injuries usually happen over bony parts of the body . A pressure injury can become life-threatening if it advances to a deep wound or becomes infected.
Read Also: How To Heal Ulcerative Colitis Flare
Stage 4 Decubitus Ulcers
This is the most severe type of decubitus ulcer stage and has the deepest wound. Not only is the skin damaged, but joints, muscles and tendons around the skin can also be damaged and are often exposed. This deep open wound is a problem, because it leads to severe infections and diseases that can ravish the immune system of patients. Once the bone becomes infected during this stage, it can lead to death or the need for amputation.
The stages of decubitus ulcers progress quickly and must be managed before they reach stage 4. These sores are often preventable and measures must be taken to ensure that infection, death and amputation do not occur.
Stage 4 Bedsore / Decubitus Ulcer
Stage 4 Bedsore is the last and most serious stage of all bedsores. In a stage 4 bed sore the patient has large-scale destruction of tissue, muscle and skin occurs. Such massive loss of tissue can also include, along with damage to muscle, bone, and even supporting structures such as tendons and joints. Stage 4 bed sores or decubitus ulcers usually require surgery to remove decayed or necrotic tissue. If aggressive treatment of a stage 4 bedsore is not taken, then further necrosis and infection can lead to septacemia, possible needed amputation and even death.
Stage 4 medical treatment include debridement, constant changing of dressing & cleansing for proper wound care, electrical stimulation and surgery. Stage 4 surgery may consist of excising of pressure ulcer, surrounding scar, bursa, soft tissue calcification, and underlying necrotic or infected bone. On deeper stage 4 bedsores and decubitus ulcers a flap surgery is needed to close the wound, fill in the dead space thus enhancing vascularity of the healing wound, and distributing pressure off the bone. All stage 4 bedsore were Stage 3 bedsores at one time, but due to the lack of quality medical and nursing care, the pressure sore continued to get worse and progressed.
Neglect is the Major Cause of a Stage 4 Bedsore
You May Like: Best Over The Counter Medicine For Stomach Ulcers
Appendix 6 Assessment Of Risk Of Bias
1. Was the allocation sequence randomly generated?
Low risk of bias
The investigators describe a random component in the sequence generation process such as: referring to a random number table using a computer randomnumber generator coin tossing shuffling cards or envelopes throwing dice drawing of lots.
High risk of bias
The investigators describe a nonrandom component in the sequence generation process. Usually, the description would involve some systematic, nonrandom approach, for example: sequence generated by odd or even date of birth sequence generated by some rule based on date of admission sequence generated by some rule based on hospital or clinic record number.
Unclear
Insufficient information about the sequence generation process provided to permit a judgement of low or high risk of bias.
2. Was the treatment allocation adequately concealed?
Low risk of bias
Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation sequentiallynumbered drug containers of identical appearance sequentiallynumbered, opaque, sealed envelopes.
High risk of bias
3. Blinding was knowledge of the allocated interventions adequately prevented during the study?
Low risk of bias
Any one of the following.
High risk of bias
Any one of the following.
Unclear
4. Were incomplete outcome data adequately addressed?
Low risk of bias