The 2019 Clinical Practice Guidelines 1 Recently Launched Jointly By Epuap Npiap And Pppia Recognises The Critical Significance Of Sub
The primacy of clinical judgment of qualified health professionals pervaded the CPG text, rightly in our view. Of the many observations about the CPGs, there was strong recognition of the incipient etiological processes associated with PU/PI development. PU/PIs are wounds, and like other wounds, PU/PIs in the early stages of cell death and necrosis show measurable signs of localized inflammatory edema. Measurement of these by subjective tests alone is impossible, or near impossible, said Martin Burns, BBIs CEO.
The days of subjective skin and tissue assessments of this #1 reported patient harm being the only tool available to nurses in their diagnosis of PU/PIs are ending. We are very pleased for patients, providers and payors that the CPGs state that healthcare practitioners, using their own qualified clinical judgement, consider using a sub-epidermal moisture/edema measurement device as an adjunct to routine clinical skin assessment1, added Burns.
The CPGs reiterated the health-disparity of patients with darkly pigmented skin. Such patients have higher incidence of more severe PU/PI and are four times more likely to die from PU/PI associated causes than patients with lightly pigmented skin2. CGP recommendation 2.7 states that healthcare practitioners, using their own qualified clinical judgement in assessing darkly pigmented skin, consider assessment of skin temperature and sub-epidermal moisture as important adjunct assessment strategies1.
References
Prevention And Treatment Of Pressure Ulcers/injuries: Clinical Practice Guideline
PPPIA is pleased to be a part of an international collaboration with the European Pressure Ulcer Advisory Panel and National Pressure Injury Advisory Panel, to produce the most the most extensive evidence-based international pressure injury guideline . The PPPIA, who are represented in the Guideline Governance Group and all small working groups are proud to be leaders at the global level in producing this guideline.
Risk Assessment And Prevention Of Pressure Ulcers
About this Guideline
Define early interventions for pressure ulcer prevention, and to manage Stage I pressure ulcers. This best practice guideline assists nurses who work in diverse practice settings to identify adults who are at risk of pressure ulcers. This guideline focuses its recommendations on:
- Practice Recommendations including assessment, planning, intervention and discharge/transfer of care
- Educational Recommendations for supporting the skills required for nurses working with adults at risk for pressure ulcers
- Organization & Policy Recommendations addressing the importance of a supportive practice environment as an enabling factor for providing high quality nursing care, which includes ongoing evaluation of guideline implementation.
Revised: 2011 Supplement: 2005 Evidence Boosters: 2017
Related File
Don’t Miss: Can You Donate Blood If You Have Ulcerative Colitis
Individualized Clinical Practice Guidelines For Pressure Injury Management: Development Of An Integrated Multi
1Louis Stokes Cleveland VA Medical Center, Cleveland, OH, United States
2Department of Orthopaedics, Case Western Reserve University, Cleveland, OH, United States
3Institute for Biomedical Informatics, University of Kentucky, Lexington, KY, United States
4Department of Computer Science, University of Kentucky, Lexington, KY, United States
5Department of Population and Quantitative Health Sciences, Case Western Reserve University, Cleveland, OH, United States
Acp Clinical Practice Guidelines

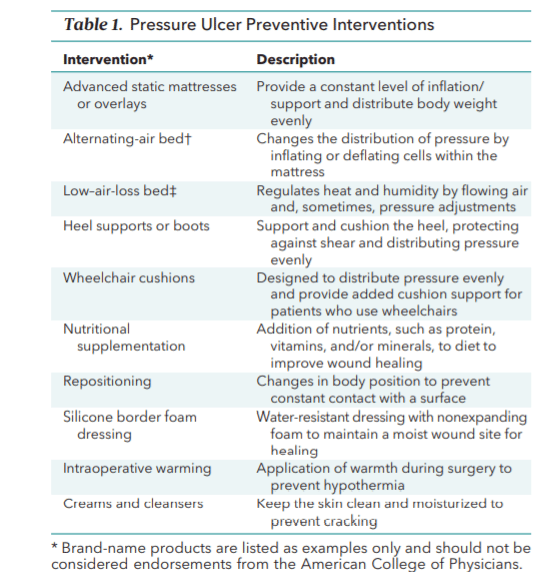
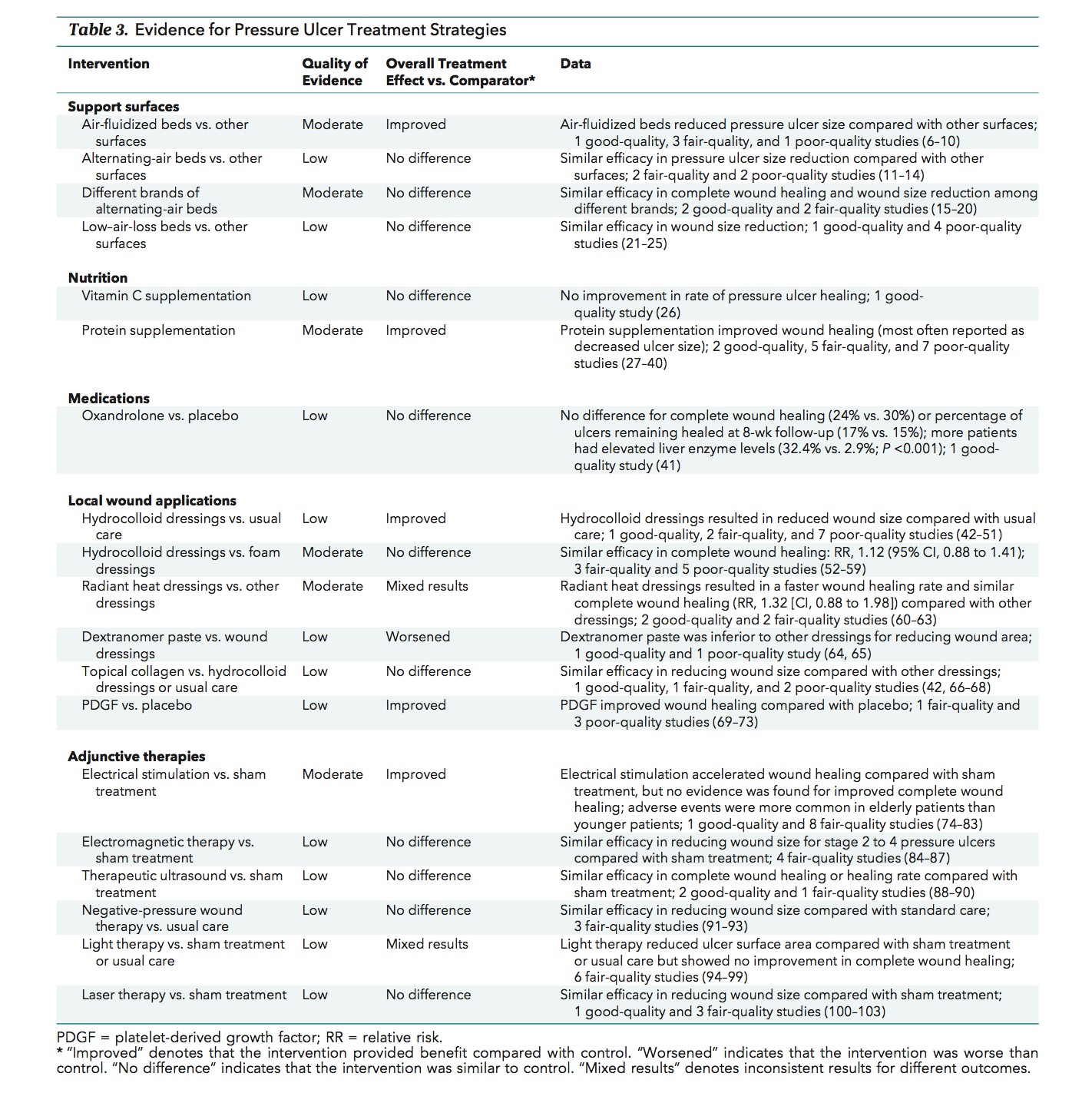
The 2015 American College of Physicians clinical practice guidelines for risk assessment, prevention, and treatment of pressure ulcers included the following recommendations and statements :
References
Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System. J Wound Ostomy Continence Nurs. 2016 Nov/Dec. 43 :585-597. . .
NPIAP pressure injury stages. National Pressure Injury Advisory Panel. Available at . Accessed: April 29, 2022.
Woolsey RM, McGarry JD. The cause, prevention, and treatment of pressure sores. Neurol Clin. 1991 Aug. 9:797-808. .
Abrussezze RS. Early assessment and prevention of pressure ulcers. Lee BY, ed. Chronic Ulcers of the Skin. New York: McGraw-Hill 1985. 1-9.
Schweinberger MH, Roukis TS. Effectiveness of instituting a specific bed protocol in reducing complications associated with bed rest. J Foot Ankle Surg. 2010 Jul-Aug. 49:340-7. .
Zhao G, Hiltabidel E, Liu Y, Chen L, Liao Y. A cross-sectional descriptive study of pressure ulcer prevalence in a teaching hospital in China. Ostomy Wound Manage. 2010 Feb 1. 56:38-42. .
Pham B, Stern A, Chen W, Sander B, John-Baptiste A, Thein HH, et al. Preventing pressure ulcers in long-term care: a cost-effectiveness analysis. Arch Intern Med. 2011 Nov 14. 171:1839-47. .
Recommended Reading: Why Do I Keep Getting Mouth Ulcers
What Additional Resources Are Available To Identify Best Practices For Pressure Ulcer Prevention
A number of guidelines have been published describing best practices for pressure ulcer prevention. These guidelines can be important resources to use in improving pressure ulcer care. In addition, the International Pressure Ulcer Guideline released by the National Pressure Ulcer Advisory Panel and the European Pressure Ulcer Advisory Panel is available. A Quick Reference Guide can be downloaded from their Web site at no charge.
Resources
Clinical Practice Guideline 3: Pressure ulcers in adults: prediction and prevention. Rockville, MD: Agency for Healthcare Policy and Research May 1992. AHCPR Pub. No. 92-0047. Archived at: .
Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. Consortium for Spinal Cord Medicine Clinical Practice Guidelines. J Spinal Cord Med 2001 Spring 24 Suppl 1:S40-101.
National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel . Quick Reference Guide version of the NPUAP/EPUAP International Pressure Ulcer Prevention Guidelines: Available at: and .
The following guidelines are available for a fee:
American Medical Directors Association: Pressure Ulcers in the Long-Term Care Setting. Available at: http://www.amda.com
Clinical Practice Guidelines For Intervention And Care Of People With Pressure Ulcers Or Risk Of Suffering
- Gustavo David Matiz Vera Renata Virginia Gonzalez Consuegra, RN Julian Daniel Hernandez Martinez Lizeth Xiomara Guzman Carrillo, RN
- Sigma Affiliation
Popular Works for Vera, Gustavo David Matiz by View
| Title |
|---|
Popular Works for Vera, Gustavo David Matiz by Download
| Title |
|---|
View Citations
Citations
Read Also: Can I Live A Normal Life With Ulcerative Colitis
Permission To Translate The International Pressure Ulcers/injuries Guideline
The 2009 Quick Reference Guide was translated into 17 languagesother than English.
The 2014 Quick Reference Guide was translated into 13 languages other than English,and the full Clinical Practice Guideline was translated into two languages other than English.
The EPUAP, NPIAP, and PPPIA welcome translations of the 2019 Quick Reference Guide into languages other than English.
The organizations have established processes for translation and for dissemination of translated versions. Permission must be sought before commencing a translation. Visit the EPUAP website for information on requirements for undertaking a translation and to seek permission to undertake a translation.
For questions about translation please contact:.
The Purpose Of The Guideline
The purpose of the guideline is to implement evidence-based guidelines for caregivers of palliative care patients on pressure ulcer prevention. This guideline aims to improve the knowledge and practice of caregivers and enables them to take measures to prevent pressure ulcer development among palliative care patients, thereby improving the quality of life of palliative care patients.
Also Check: What Is It Like To Have An Ulcer
Pressure And Shear Injury
It is possible to determine the potential source of pressure and shear injury based on the patients posture, activities, mobility, lifestyle and current support surfaces such as sleeping and sitting surfaces. When pressure is exerted near a bony prominence, the risk of pressure injuries increases by 35 times. Shear injuries may happen when trying to change the positions of the patient.
The International Guideline 3rd Edition
are proud to announce that the International Guideline is now available. The goal of this international collaboration is to develop evidence-based recommendations for the prevention and treatment of pressure injuries for use by health professionals throughout the world. An explicit scientific methodology has been used to identify and critically appraise all available research.
The guideline presents recommendations made on the best evidence available at time of publication as consistent with the guideline methodology. Nothing in this guideline is intended as endorsement of a specific product. The guideline developers do not give any approvals for use of guideline branding or logos to endorse products. Nothing in this guideline is intended as advice regarding credentialing standards, coding standards or reimbursement regulations.
For the International Guideline , small working groups included representatives from Associate Organisations of the Partner Organisations . Associate Organisations are:
Also Check: Ulcer Symptoms Blood In Stool
What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
Criteria For Selection Of Studies
Type of participants
Any palliative care patients who are prone to pressure ulcer development .
Type of intervention
The following criteria were included in the study:
Any measures used to prevent pressure ulcers among bedridden adult patients were included.
No pressure ulcer at the time of recruitment to the study.
Studies focusing solely on educational interventions that were not accompanied by other interventions.
Exclusion criteria
Also Check: Can A Heating Pad Help Ulcerative Colitis
What Items Should Be In Our Bundle
The sections above have outlined best practices in pressure ulcer prevention that we recommend for use in your bundle. However, your bundle may need to be individualized to your unique setting and situation. Think about which items you may want to include. You may want to include additional items in the bundle. Some of these items can be identified through the use of additional guidelines .
Action Steps
Identify your bundle of best practices.
3.5.1 How do we customize the bundle for specific work units?
Patient acuity and specific individual circumstances will require customization of the skin and pressure ulcer risk assessment protocol. It is imperative to identify what is unique to the unit that is beyond standard care needs. These special units are often the ones that have patients whose needs fluctuate rapidly. These include the operating room, recovery room, intensive care unit, emergency room, or other units in your hospital that have critically ill patients. In addition, infant and pediatric patients have special assessment tools, as discussed in section 3.3.5.
Action Steps
- Identify the units that will require customization of the skin and risk assessment protocols.
- Modify the bundle, the assignment of roles, and the details of the unit to meet these special features.
Additional Information
The International Guideline Qrg App
|
Announcing the Official Mobile App of the EPUAP, NPIAP, and PPPIA – 2019 International Pressure Ulcer/Injury Guideline! You’re invited to the launch of our exciting new app! We’ve taken the years of time and dedication poured into the International Guideline, and turned it into a useful Mobile App. This beautiful app places all of the Quick Reference Guideline content at your fingertips today… Find out more now! |
Guideline purchase links and support documents,and information about requesting permissions forreproductionand translated versions are available.News and statements from the guideline development team relating to guidelinecontent can be found at News and Statements.
Please direct all enquiries to
Read Also: Decaf Coffee And Ulcerative Colitis
What Bundle Of Best Practices Do We Use
Given the complexity of pressure ulcer prevention, with many different items that need to be completed, thinking about how to implement best practices may be daunting. One approach that has been successfully used is thinking about a care bundle. A care bundle incorporates those best practices that if done in combination are likely to lead to better outcomes. It is a way of taking best practices and tying them together in a systematic way. These specific care practices are among the ones considered most important in achieving the desired outcomes.
The pressure ulcer bundle outlined in this section incorporates three critical components in preventing pressure ulcers:
- Comprehensive skin assessment.
- Standardized pressure ulcer risk assessment.
- Care planning and implementation to address areas of risk.
Because these aspects of care are so important, we describe them in more detail in the subsequent subsections along with helpful clinical hints. While these three components of a bundle are extremely important, your bundle may stress other aspects of care. It should build on existing practices and may need to be tailored to your specific setting. Whatever bundle of recommended practices you select, you will need to take additional steps. We describe strategies to ensure their successful implementation as described in Chapter 4.
The challenge to improving care is how to get these key practices completed on a regular basis.
Resources
Additional Information
Tools
Practice Insights
How Should A Standardized Pressure Ulcer Risk Assessment Be Conducted
As discussed above, one purpose of comprehensive skin assessment is to identify visible changes in the skin that indicate increased risk for pressure ulcer development. However, factors other than skin changes must be assessed to identify patients at risk for pressure ulcers. This can best be accomplished through a standardized pressure ulcer risk assessment.
3.3.1 What is a standardized pressure ulcer risk assessment?
After a comprehensive skin examination, pressure ulcer risk assessment is the next step in pressure ulcer prevention. Pressure ulcer risk assessment is a standardized and ongoing process with the goal of identifying patients at risk for the development of a pressure ulcer so that plans for targeted preventive care to address the identified risk can be implemented. This process is multifaceted and includes many components, one of which is a validated risk assessment tool or scale.
Other risk factors not quantified in the assessment tools must be considered. Risk assessment does not identify who will develop a pressure ulcer. Instead, it determines which patients are more likely to develop a pressure ulcer, particularly if no special preventive interventions are introduced. In addition, risk assessment may be used to identify different levels of risk. More intensive interventions may be directed to patients at greater risk.
Action Steps
Ask yourself and your team:
3.3.2 Why is a pressure ulcer risk assessment necessary?
Action Steps
Ask yourself and your team:
Don’t Miss: What Are The Signs You Have An Ulcer
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Skin integrity .
Tools
Detailed instructions for assessing each of these areas are found in Tools and Resources .
Action Steps
The 2014 International Pressure Ulcer Guideline: Methods And Development
Emily Haesler PhD BN PG DipAdv Nurs
Adjunct Associate Professor
Curtin University, School of Nursing, Midwifery and Paramedicine, Perth, Western Australia, Australia
Correspondence to E. Haesler:
Associate Professor
Emily Haesler PhD BN PG DipAdv Nurs
Adjunct Associate Professor
Curtin University, School of Nursing, Midwifery and Paramedicine, Perth, Western Australia, Australia
Correspondence to E. Haesler:
Associate Professor
Also Check: Is Having Ulcerative Colitis A Disability
World Stop Pressure Ulcer/injury Day
What do you have planned to stop pressure injuries in your workplace? Stop Pressure Injury Day is the perfect opportunity to raise awareness. To help you implement evidence-based pressure injury prevention, the NPIAP/EPUAP/PPPIA are offering the 2019 International Pressure Injury Guideline FOR FREE if you order 16-19 Nov 2022. Visit the Guideline Sales site to review the conditions and order your copy of the Guideline.
General Statement On Use Of The Npuap/epuap International Classification System
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Emily Haesler . Cambridge Media: Osborne Park, Western Australia 2014
Recommended Reading: Foam Dressings For Treating Pressure Ulcers